Endocrinology & Metabolic Syndrome
Open Access
ISSN: 2161-1017
ISSN: 2161-1017
Research - (2019)Volume 8, Issue 2
Background: Diabetic foot is defined as the foot of the diabetic patients with ulceration, infection, and/or distraction of the deep tissues associated with neurological abnormalities and varying degrees of peripheral vascular disease of the lower limb. Diabetic foot ulcers are a common and much feared complication of diabetes. The study is aimed to identify incidence of diabetic foot ulcer in diabetes patients of Nekemte Referral Hospital (NRH).
Methods: A prospective observational study of diabetes mellitus patients who had diabetic foot ulcer was conducted from March15 to June 15, 2018.The data was entered into EPI-manager 4.0.2 software and analyzed using SPSS V.24. The Wagner classification of diabetic foot ulcer was used to assess the severity of foot ulcers. Size of ulcer was determined by multiplying the largest by the second largest diameter perpendicular to the first and the etiology of diabetic foot ulcer was identified by using gram stains.
Results: Over the study period, 644 diabetes patients were admitted to the NRH medical service; of these, 115 (17.86%) had foot ulcers. About 61 (55.7%) were males and mean age of participants was 44.4 ± 14.7. After the gram stain was performed, about 77 (66.96%) of the patients with foot ulcer developed infection. From the diabetes mellitus who had developed diabetic foot ulcer, about 31 (26.96%) of ulcer were located on dorsal/interdigital toes. About 49 (42.61%) of the diabetic foot ulcer patients had previous history of ulcer of any location. Of infected diabetic foot ulcers, Forty two (54.55%) of microorganism isolated was gram positive.
Conclusion: The incidence of diabetic foot ulcer among diabetic patients in Nekemte referral hospital was high. Therefore, East wollega zone health sector and Nekemtereferal hospital diabetic clinic diabetic care providers should strive to reduce its incidence through enhancing the regular diabetic foot evaluation.
Diabetic foot ulcer; Incidence; Nekemte referral hospital
Diabetes mellitus is a non-communicable disease and one of the most common chronic diseases [1]. It is characterized by chronic hyperglycemia with disturbances of carbohydrate, fat and protein metabolism resulting from defects in insulin secretion, insulin action, or both [2].
According to the International Diabetes Federation (IDF), 425 million people were estimated to live with diabetes in 2017, out of which about an estimated 15.5 million adults aged 20-79 years were living with diabetes in Africa Region, representing a regional prevalence of 3.3%. Africa’s most populous countries, including Ethiopia, have the highest numbers of people with diabetes. Ethiopia, which is one of the developing nations, is at a risk of increased diabetes incidence. About 2.57 million of the population is estimated to live with diabetes in 2017 [3].
Complications of DM causes significant physical and psychological morbidity, disability and premature mortality among those affected patients and imposes a heavy financial burden on health service [4]. It is characterized by multiple long-term complications affecting almost every system in the body [5].
Diabetic foot is defined as the foot of the diabetic patients with ulceration, infection, and/or distraction of the deep tissues associated with neurological abnormalities and varying degrees of peripheral vascular disease of the lower limb [6]. Diabetic foot ulcers are a common and much feared complication of diabetes, with recent studies suggesting that the lifetime risk of developing a foot ulcer in diabetic patients may be as high as 15% [7]. Foot infection was defined according to the International Working Group on the Diabetic Foot classification system as at least two clinical signs or symptoms of infection in or around the DFU including purulence, erythematic, pain, tenderness, warmth and/or indurations [8].
Diabetic foot complications are common amongst people living with diabetes. Foot ulcerations are one of the most feared complications for both people with diabetes and health care providers due to their negative impact on lives resulting in overall poor prognosis of the disease leading to long period of hospitalization and substantial health care costs [9].
Foot complications, especially foot ulcers, constitute a major public health problem for diabetes patients in sub-Saharan Africa and are important causes of prolonged hospital admission and death in patients from this part of the continent [10].
Foot ulceration and supervening infection are a major cause of morbidity in diabetes patients. Diabetes foot lesions necessitate more hospital admissions than any other specific complications of diabetes [11]. The prevalence of these infections in DFU has been reported to range between 25 ± 60%. Although the critical nature and prevalence of infected DFUs are well appreciated, the development of these infections in the first place has received less attention [8].
In many less-developed countries, foot infections are especially common where there are no available chiropody services, or lesions are ignored or detected relatively late in the course of the infection after unsuccessful home therapy, such as soaking in hot water or application of unproven home remedies or after seeking medical assistance from traditional healers. In those patient’s diabetes has an infectious etiology. Patients often present to hospital only after gangrene and infection have developed, or after localized infection has progressed to systemic sepsis that might not be amenable to conventional supportive therapy with antimicrobials [12].
Diabetic foot ulcer is the most fatal complication of diabetes mellitus [7]. Despite this, no study has been done on incidence of diabetic foot ulcer in NRH. This study will identify the magnitude of diabetic foot ulcer patients and the most causative organism of diabetic foot infection in this area.
Study setting and study period
A prospective observational study was conducted at NRH from March 15 to June 15, 2018. The hospital is located in Nekemte town, which is located 330 km to the west of Addis Ababa, the capital city of Ethiopia. The hospital is a referral hospital and gives health service for more than 10, 000,000 people living in west Ethiopia. There were about 2420 diabetic patients who have been following diabetic clinic annually.
Study participants and eligibility criteria
Patients >18 years who were be diagnosed as diabetes, diabetic patients who had diabetic foot ulcer, patients who were willing to participate in the study and diabetes mellitus patients who had any visible foot lesions patients were included. Patients with diabetic patients who had traumatic ulcer due to other than normal cause like car accident, burn and any injury to sharpened materials and diabetic patients who were severely ill and unable to communicate throughout the study period were excluded. Patients with Diabetic patients who had traumatic ulcer due to other than normal cause like car accident, burn and any injury to sharpened materials and diabetic patients who were severely ill and unable to communicate throughout the study period were excluded.
With this, 115 patients were selected from the total of 644 diabetes mellitus patients.
Study variables and outcome end points
Incidence of diabetic foot ulcer was the dependent variable and the primary outcome was the incidence of diabetic foot ulcer. The Wagner classification of diabetic foot ulcer was used to assess the severity of foot ulcers. Extent (i.e. size) was determined by multiplying the largest by the second largest diameter perpendicular to the first. The status of diabetic foot ulcer which developed infection or not were identified by using gram stains.
Data collection process and management
Data was collected using questionnaire which was developed after reviewing different literature. One medical doctor, one nurses and one pharmacist were recruited as data collector; one medical doctor was assigned to supervise the data collection process. A pus swab was obtained from the ulcers prior to any ulcer cleaning and avoiding other contamination. The samples were delivered to the laboratory immediately and a thin smear was prepared on Grease or oil free slides. The data collectors as well as the supervisor were given two-day training on the overall data collection procedure. Five percent of the sample was pre-tested to check acceptability and consistency of data collection tool two weeks before the actual data collection.
Data processing and analysis
The data was entered in to computer using EPI-manager 4.0.2 software. Data checking and cleaning was done by principal investigator on daily basis during collection before actual analysis. Analysis was done using statistical software for social sciences (SPSS) 24. Descriptive data was generated and placed in terms of frequency and percentage. Descriptive statistics was used to analyze data in terms of frequency and percentage.
Operational definitions
Diabetic Foot ulcer: The foot of a diabetic patient that has the potential risk of pathologic consequences, including infection, ulceration, and/or destruction of deep tissues.
Grades of diabetic’s foot ulcer: For purpose of this study we used Wagner system for classification of diabetic foot ulcer which uses 6 wound grades (scored 0 to 5) to assess ulcer depth [13].
Grade 0 diabetic foot ulcer: No ulcer, but the foot is at risk for ulceration
Grade 1 diabetic foot ulcer: Superficial ulceration
Grade 2 diabetic foot ulcer: Ulcer with deep infection, but without involvement of the bone
Grade 3 diabetic foot ulcer: Ulcer with osteomyelitis.
Grade 4 diabetic foot ulcer: Presence of localized gangrene on the foot.
Grade 5 diabetic foot ulcer: Presence of gangrene of the whole foot.
Socio-demographic characteristics
Over the study period, 115 diabetes foot ulcer patients were admitted to the NRH medical ward; of these patients, 64 (55.65%) were males. About 26 (22.61%) of them were in the age range of 58-67, while mean age of participants was 44.4 ± 14.7. About 34 (29.57%) of the diabetic foot ulcer were overweight and 16 (13.91%) were obese while the mean Body Mass Index (BMI) was 24.94 ± 3.69 kg/m2. Eighty (69.57%) were married (Table 1).
| Variables | Frequency | Percent | |
|---|---|---|---|
| Sex | Male | 64 | 55.65 |
| Female | 51 | 44.35 | |
| Age | 18-27 | 16 | 13.91 |
| 28-37 | 14 | 12.17 | |
| 38-47 | 15 | 13.04 | |
| 48-57 | 24 | 20.87 | |
| 58-67 | 26 | 22.61 | |
| 68-77 | 20 | 17.39 | |
| Marital Status | Married | 80 | 69.57 |
| Single | 21 | 18.26 | |
| Window | 8 | 6.96 | |
| Divorced | 6 | 5.22 | |
| Monthly Income | <25$ | 30 | 26.09 |
| 25-50$ | 36 | 31.30 | |
| 51-100$ | 25 | 21.74 | |
| >100$ | 24 | 20.87 | |
| Educational level | Illiterate | 24 | 20.87 |
| Primary school | 29 | 25.22 | |
| Secondary school | 22 | 19.13 | |
| Above Secondary school | 40 | 34.78 | |
| BMI | <24.5 | 65 | 56.52 |
| 24.5-29.5 | 34 | 29.57 | |
| >29.5 | 16 | 13.91 | |
Table 1: Socio-demographic characteristics of respondents in Nekemte Referral Hospital, west Ethiopia, 2018.
Incidence of diabetic foot ulcer
Over the study period, 644 diabetes patients were admitted to the NRH medical service; of these, 115 (17.86%) had foot ulcers. Majority of the patients, 23.48% had grade1 diabetic foot ulcer (Figure 1).
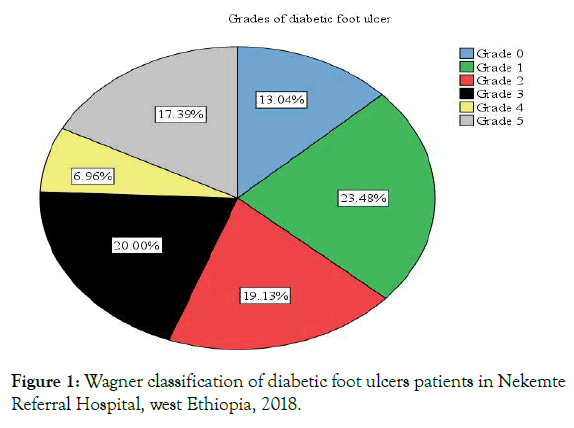
Figure 1. Wagner classification of diabetic foot ulcers patients in Nekemte Referral Hospital, west Ethiopia, 2018.
From the diabetes mellitus who had developed diabetic foot ulcer, about 31 (26.96%) of ulcer were located on dorsal/interdigital toes. About 49 (42.61%) of the diabetic foot ulcer patients had previous history of ulcer of any location, whereas 66 (57.39%) of the patients did not have previous history of ulcer (Figure 2).
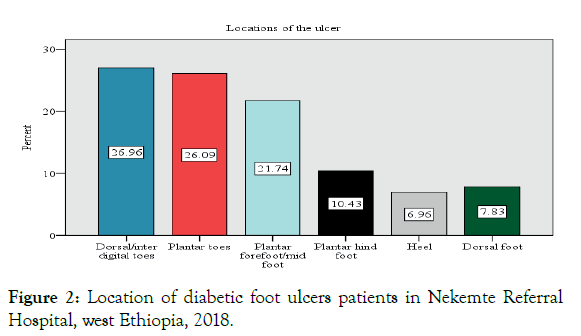
Figure 2. Location of diabetic foot ulcers patients in Nekemte Referral Hospital, west Ethiopia, 2018.
Among the total 115 study participants with DFU, 77 (66.96%) of foot ulcer progressed to infection. Of infected diabetic foot ulcers, forty-two (54.55%) of microorganism isolated was gram positive (Table 2).
| Variables | Frequency (N) | Percent (%) | |
|---|---|---|---|
| Ulcer which develop Infection | Yes | 77 | 66.96 |
| No | 38 | 33.04 | |
| Gram stain result | Gram positive | 42 | 54.55 |
| Gram negative | 20 | 25.97 | |
| Poly microbial | 15 | 19.48 | |
| No bacteria | 38 | 33.04 | |
Table 2: Clinical characteristic of diabetic foot ulcer patients in diabetes mellitus patients admitted to Nekemte Referral Hospital, west Ethiopia, 2018.
This study assessed burden of diabetic foot ulcer at NRH, western Ethiopia. The study found that the incidence of diabetic foot ulcers amongst diabetic patients at the NRH was 17.86%. The study in Taiwan, Singapore and Bangalore, India found the incidence of 2.9%, 8.2% and 8%, respectively which were lower than our study [1,14,15]. The differences might be due to variation in racial difference, differences in life style and socio-cultural variation of study participants. A study was comparable with the study done in Arbaminch and Gondar which found prevalence of 14.8% and 13.6%, respectively [16,17].
The majority of the patients who developed diabetic foot ulcer were males (55.65%). This figure is similar with the study done in Nigeria, Arbaminch and Jimma which was 67.2% and 59.7% and 62.9%, respectively [17-19]. The variation of DFU related to sex, might be reflection of variation in societal role between male and females in western Ethiopia, typically in the study area. Males spent most of their time outside homes doing jobs that need more energy compared to women. The increase in DFUs among diabetic patients, particularly in current study area, is worrying situation for individual families as males are the backbone and the sole earning members of the family, particularly in western Ethiopian population.
The mean age of the diabetic foot ulcer patient was 44.4 ± 14.7 which is comparable with the study done in Jimma which found 44.4 (±15.6) years [19]. However, the mean age of the patients was lower than the study done in Bangalore, India (55.97 ± 11.6years), Indonesia (54.3 ± 8.6 years) and Central Greece (69.7+9.6 years) [1,20,21]. This difference may be due to studies were conducted in different centers offer different qualities of diabetes care.
The majority of the DFU was in grade 1 (23.48%). However, the study done at Ayder referral hospital found that 38% of the patients with foot ulcers were Wagner’s grade 0 [5]. In Nigeria most of the DFU were in grade 4 with distribution of DFU in relation to clinical stages was 40%, 25.7%, 17.1% and 11.4% for stages-IV, III, II and irrespectively [18]. In our study, the distribution of DFU was 6.96%, 20.00%, 19.13% and 23.48% for stages-IV, III, II and I. In Thailand the majority of the patients had grade2 (32.8%) with distribution of the ulcers according to the Wagner classification was as follows: Wagner 1 (22.5%); Wagner 2 (32.8%); Wagner 3 (32.1%); Wagner 4 (11.8%); and Wagner 5 (0.8%) [22].
The most causative organisms for diabetic foot ulcer in NRH during study period for patients was gram positive 42 (54.55%) followed by gram negative 20 (25.97%) and poly-microbial 15 (19.48%). Study in Thailand showed that most causative organisms for diabetic foot ulcer were gram negative, gram positive and poly microbial respectively [22]. The study in Singapore in 2010 showed that gram positive organism is the most prevalent [15]. Similarly, the study conducted in the Switzerland found that the most causative organism for diabetic foot ulcer were gram positive followed by gram negative bacteria [11].
According to the gram-stain results about 77 (66.96%) of the patients presents with diabetic foot ulcer developed infection and 38 (33.04%) of them did not developed any type of infection. This figure is higher than the study done in Australia and Jamaica in which the incidence of diabetic foot infection was 40.1% and 3.7%, respectively [8,23]. This difference in incidence of diabetic foot infection is might be due to the difference in the quality of service, life style of the patients and quality podiatric service.
As strength, the study was conducted among DFU patients as the foot complication of Diabetes mellitus patient is increasing in developing world and this study was a prospective observational study and may be used as baseline information for other researchers. As limitations, culture and sensitivity tests were not done to identify specific strain of the pathogen. Further, the follow-up period was short, thus failing to take into account any non- healing ulcers resulting in infection after this time.
The incidence of diabetic foot ulcer among diabetic patients in Nekemte Referral Hospital was found to be high. Majority of the study participants had foot ulcer Wagner’s grade 1 and most of diabetic foot ulcers were located on dorsal/interdigital toes. Most of the diabetic foot ulcers were progressed to infection and majority of them was gram positive. However, some of diabetic foot ulcer patients didn’t grew any bacteria.
In order to reduce the incidence of diabetic foot ulcer and its associated unwelcomed effects East Wollega zone health sector and Nekemte referal hospital diabetic clinic diabetic care providers should strive to reduce its incidence through enhancing the regular diabetic foot evaluation. Additionally, to minimize the risk of developing diabetic foot infection, health educators should emphasize on the benefit of foot care. In this study gram stains were used to determine whether diabetic foot ulcers were infected or not. Therefore, laboratory services should be strengthened like culture and sensitivity tests to identify specific strain of the pathogen.
We thank Jimma University for funding this study. We are grateful to staff members and health care professionals of NRH, data collectors and study participants for their cooperation in the success of this study.
FB contributes in the proposal preparation, study design, analysis and write up the manuscript. GF contributed to the design of the study, analysis and edition of the manuscripts. KB and DD made a substantial contribution to the local implementation of the study. All authors read and approved the final version of the manuscript.
Ethical clearance was obtained from the ethics review board of Jimma University. Permission was obtained from medical director of the NRH to access diabetes patients and conducts the study. The benefit and risks of the study was explained to each participant included in the study and written consent were obtained from each patient involved in the study. To ensure confidentiality, name and other identifiers of patients and health care professionals were not recorded on the data collection tools.
Not applicable. No individual person’s personal details, images or videos are being used in this study.
The study was funded by Jimma University. The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
No competing interests exist.
Citation: Bekele F, Fekadu G, Bekele K, Dugassa D (2019) Incidence of Diabetic Foot Ulcer among Diabetes Mellitus Patients Admitted to Nekemte Referral Hospital, Western Ethiopia: Prospective Observational Study. Endocrinol Metab Syndr 8:300.
Received: 30-Apr-2019 Accepted: 22-May-2019 Published: 29-May-2019
Copyright: © 2019 Bekele F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : The study was funded by Jimma University. The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.