Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Research Article - (2020)Volume 8, Issue 1
Background: in sub-Saharan Africa, the co-morbidity of diabetes mellitus and HIV is still poorly assessed. This study aimed to determine the incidence and risk factors of diabetes mellitus among PHAs with HIV followed on an outpatient basis at the adult day hospital (HDJ) in Bobo-Dioulasso, Burkina Faso.
Methods: A retrospective cohort study was conducted and concerning period from January 2008 to December 2015 at the adult HDJ. The diagnosis of diabetes mellitus was based on the basis of 2 blood glucose levels >7 mmol/l or patient having a status of diabetes mellitus confirmed. The Cox proportional risk method was used to identify risk factors for the development of diabetes mellitus. The significance level was set at p value < 5% for all statistical tests. Data were analyzed by STATA13 software.
Results: we included 4,500 patients. The incidence of diabetes mellitus was 4.7 per 1000 person-years. Diabetic subjects were predominantly infected with HIV1 (89.4%); the age group 36-45 years was the most represented (34.6%). We observed a predominance of females (61.5%) and an abnormal body mass index (BMI) for 42.9% of cases.
The majority of diabetics were detected at WHO stage 3 (42.5%), had arterial hypertension (38.0%), had abnormal glomerular filtration rate (30.0%) and had CD4 counts of less than 350 cells/μl for 70.0% of the cases. among them 38% had hypertension; 30% had abnormal glomerular filtration rate and 70% had a low CD4 count of less than 350 cells/μl. In multivariate analysis only age >55 years was identified as an independent risk factor for the occurrence of diabetes mellitus during follow-up.
Conclusion: Diabetes mellitus was found among PLWHIV from the day hospital cohort in Bobo Dioulasso. Age was the risk factor found for the onset of diabetes. Integrated approach for patient’s management in different units in sub-Saharan Africa is suitable facing double epidemiological burden.
Burkina faso; Diabetes HIV; Incidence; Risk factors
Diabetes mellitus is a chronic metabolic disease whose in the world prevalence has been estimated by the World Health Organization (WHO) at 10% [1]. In sub-Saharan Africa, the prevalence of diabetes mellitus is increasing in Africa due to the ageing of the population and the accelerated urbanization leading to a sedentary lifestyle in modern African societies [2,3]. In 2013, the prevalence of diabetes mellitus was estimated at 4.9% in Burkina Faso [4].
The advent of highly active antiretroviral therapy (ART) has significantly increased the life expectancy of HIV-infected patients. As a result, morbidity, mortality and new HIV infections have fallen by 35% since 2000 [5]. In Burkina Faso, HIV prevalence has fallen from 7.17% in 1997 to 0.7% in 2018[8]. Since 1st January 2010, free ART allowed to increase ART coverage in Burkina Faso with more than 100 medical care facilities (public, private, religious and associative). Despite the efficiency of ARV treatment, the life expectancy of HIV-positive people has remained lower than that of the general population [6].
This excess mortality is partly related to immunodeficiency but mainly to organic and metabolic diseases such as diabetes mellitus and heart disease which are not used for Acquired Immune Deficiency Syndrome (AIDS) AIDS classification [7-12]. However, few studies have been carried out on patients co-affected by HIV and diabetes in our country and more precisely at the Day Hospital (HDJ) of Bobo-Dioulasso.
The present study determined the incidence and the risk factors for the onset of diabetes mellitus in People living with HIV (PLWHIV) outpatient followed at the HDJ in Bobo-Dioulasso, Burkina Faso.
Study setting
The study setting was the Adult day hospital (HJD in french) of the Infectious Diseases Department of the Sourô Sanou Teaching Hospital (CHUSS in french) in Bobo Dioulasso (Burkina Faso). Burkina Faso is a country in West Africa and Bobo-Dioulasso is the second largest city and the economic capital. The Day Hospital has been an outpatient referral unit for PLWHIV since 2005.
Type and period of study
This was a retrospective cohort study concerning the period from January 2008 to December 2015.
Study population
We have included all the HIV outpatients who were followed at the CHUSS adult day hospital between January 2008 and December 2015. The recruitment process was exhaustive.
Data collection
extracted from the ESOPE database. This database was filled by physicians during patient ’ treatment initiation and follow-up visits.
Data analysis
The data were analyzed using STATA 13 software. The characteristics of the study population at the initial visit were described by their size and the respective frequencies of the qualitative variables, and the means and standard deviations of the quantitative variables.
For the univariate analyses, Pearson's chi2 test was used for comparisons of proportions and Student's test for comparisons of means. The Cox proportional hazards method was used to identify factors of the onset of diabetes mellitus. The significance level was a p-value less than 5% for all statistical tests.
Ethical considerations
This study was conducted as part of routine care. All information collected was kept strictly confidential and anonymous; patient names were not included in the exported data.
During the study period, corresponding to eight (8) years 4500 outpatients were included and followed up at the Bobo- Dioulasso day hospital (Figure 1).
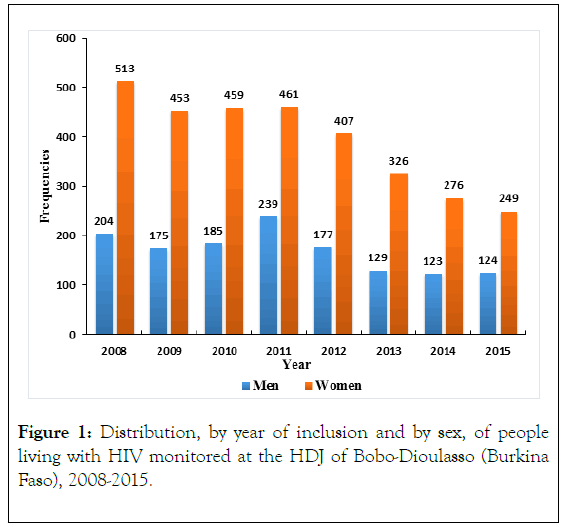
Figure 1. Distribution, by year of inclusion and by sex, of people living with HIV monitored at the HDJ of Bobo-Dioulasso (Burkina Faso), 2008-2015.
Socio-demographic data at inclusion
The average age was 37 ± 10.1 years-old and ranged from 14 to 78 years-old. The most represented age groups were 26-35 yearsold and 36-45 years-old with proportions of 32.6% and 34% respectively. There was a predominance of females with a sex ratio of 0.43 (Table 1).
| Socio-demographic characteristics | Number of cases | Percentages | |
|---|---|---|---|
| Age group (years) | |||
| ≤25 | 387 | 8.6 | |
| [26-35] | 1,467 | 32.6 | |
| [36-45] | 1530 | 34 | |
| [46-55] | 828 | 18.4 | |
| ≥55 | 288 | 6.4 | |
| Sex | |||
| Female | 3144 | 69.90% | |
| Marital status | |||
| Married | 2,502 | 55.60% | |
| Single | 866 | 19.30% | |
| Widowed | 795 | 17.70% | |
| Divorced | 332 | 7.40% | |
| Profession | |||
| Farmers | 297 | 6.60% | |
| Traders | 484 | 10.80% | |
| Civil servants | 788 | 17.50% | |
| Unemployed | 2401 | 53.30% | |
| Others | 530 | 11.80% | |
| Residence area | |||
| Hauts Bassins (town) | 4077 | 90.60% | |
| Other | 423 | 9.40% | |
Table 1: Socio-demographic characteristics of persons living with HIV monitored at the HDJ, Bobo-Dioulasso (Burkina Faso), 2008-2015.
Clinical data at first visit
The mean Body Mass Index (BMI) was 20.6 ± 4.4 kg/m² range from 6.8 to 46.1 kg/m² with a median of 20.1 kg/m². More than half of the patients, 57.1% had a normal BMI. At inclusion, WHO clinical stage 3 patients were predominant in the study population with a proportion of 44.5% (n=2001). At the initial visit 98.9% of the study population had had their blood pressure checked and of these 18% (n=800) had arterial hypertension.
Biological data at the first visit
At inclusion, CD4 lymphocyte counts were performed in 78.5% of cases. The mean CD4 count was 262.8 ± 223.7 cells/μl ranged from 1 to 2002 cells/μl, with a median of 212.5 cells/μl. More than three-quarters (72.3%) of the patients had a CD4 cell count less than 350 cells/μl. The mean initial blood glucose level was 4.9 ± 1.03 mmol/l, with a median of 4.8 mmol/l. In the study population 80.3% (n=3613) of the patients included had baseline creatinine levels; among these; 19.2% (n=695) had renal impairment (ranging from mild to end-stage renal disease) and 4.9% were on mandatory dialysis.
Antiretroviral therapy
During the study period 81.6% of patients were on ARV treatment (n=3645). According to treatment protocols 8.2% (n=367) of the patients included were on triple therapy with at least one protease inhibitor; 73.4% were on therapy without protease inhibitors (n=3307) and treatment was absent in 18.4% of cases (n=826).
Incidence of diabetes mellitus
At the end of the observation period, we counted 104 cases of diabetes mellitus among the 4500 patients monitored, i.e. a frequency of 2.3%; 46 of these patients were known to have diabetes before the 1st visit to the HDJ (1%). In addition, 58 new cases of diabetes mellitus were counted during an observation period of 12330 person-years, i.e. an incidence density of 4.7 per 1000 person-years.
General characteristics of diabetic PLWHIV
Among the 104 diabetic patients, the age group 36-45 years was the most represented with 34.6% of the population. However, the incidence of diabetes was higher in the age group of patients > 55 years with a proportion of 6.3% (p=0.0001).
Among the diabetic patients the female sex was predominant with 61.5% of the subjects. Taking into account a gender distribution, the frequency of diabetes was higher in male patients with a proportion of 3% (p=0.066).
At the initial visit, 45.2% of the diabetic subjects were at the WHO stage 3. However, the frequency of diabetes was higher in stage 4 patients with about 3%. This difference was not statistically significant, p=0.462. The BMI could be evaluated in 94.6% of patients included and 94.2% of diabetic subjects (data missing in 06 patients). More than half of the diabetic patients (57.1%) had a normal BMI. However the frequency of diabetes was higher in patients with a BMI ≥ 30 kg/m² with a proportion of 8.2% compared to patients with a normal BMI 2.3%. (p=0.0001). High blood pressure was present in 38.8% of diabetic patients. The frequency of diabetes was higher in patients with hypertension (5%) compared to patients with normal blood pressure (1.3%) p=0.0001.
More than 89.4% of the diabetic subjects were infected with HIV 1. However, taking into account the distribution of the study population according to the different serotypes, the frequency of diabetes mellitus was higher in patients infected with HIV 2 and those with dual HIV 1 and 2 with a proportion of 3.1%. Glomerular filtration rate (GFR) was assessed in 80.3% of patients and 79.8% of diabetics. Among the patients in whom GFR was assessed at the initial visit (n=3613), 2.3% were diabetic. In the group of diabetic subjects (n=83) more than half (70%) had a normal GFR. However, the frequency of diabetes was higher in the population of patients with mild renal impairment compared to the other patients, at 4.3%. This difference was statistically significant with a p=0.026.
Among the diabetic patients who had an initial CD4 count (n=79, missing data 25); 70% had a CD4 lymphocyte count at inclusion ˂ 350 cells/μl. However, taking into account a class distribution, the frequency of diabetes was higher in the group of patients with a CD4 count between 350 and 500 cells/μl (3.3%). This difference was not statistically significant, p=0.141.
Risk factors for the development of diabetes mellitus during follow-up
In univariate analysis the probability that a patient would develop diabetes mellitus during follow-up was a function of age greater than 25 years, presence of hypertension, crude RR 1.96 (95% CI [1.00-3.82]), CD4 count between 350 and 500 cells/μl, crude RR 1.96 (at 95% CI [1.00-3.82]) (Table 2).
| Age group | Diabetes | p | ||
|---|---|---|---|---|
| absent | present | Total | ||
| ≤25 | 385 (99.2%) | 3 (0.7%) | 388 (100%) | - |
| 26-35 | 1449 (98.8%) | 17 (1.2%) | 1466 (100%) | - |
| 36-45 | 1495 (97.6%) | 36 (2.4%) | 1531 (100%) | - |
| 46-55 | 797 (96.4%) | 30 (3.6%) | 827 (100%) | 0.0001 |
| >55 | 270 (93.7%) | 18 (6.3%) | 288 (100%) | - |
| Total | 4396 (97.7%) | 104 (2.3%) | 4500 (100%) | - |
Table 2: Distribution of PLHIV followed at HDJ by age group and presence of diabetes, Bobo-Dioulasso (Burkina Faso), 2008-2015.
However, a BMI between 18.5-25 kg/m² at baseline had a protective effect against the occurrence of diabetes mellitus with a crude RR of 0.34 (95% CI [0.14-0.81]). In multivariate analysis (COX model) only age >55 years was identified as an independent risk factor for the occurrence of diabetes mellitus at follow-up (Table 3).
| Associated factors | Gross RR [IC95%] | p | Adjusted RR [IC95%] | p |
|---|---|---|---|---|
| Age (years) | ||||
| ≤25 | 1 | - | - | - |
| 26-45 | 3.17 [1.36-7.37] | 0.007 | 4.11 [1.35-12.50] | 0.013 |
| 46-55 | 3.63 [1.46-9.01] | 0.005 | 3.23 [0.93-11.24] | 0.065 |
| >55 | 10.20 [4.06-25.63] | 0.0001 | 17.38 [4.81-62.76] | 1E-04 |
| Reason for serology | ||||
| Management of mother-to-child transmission | 1 | - | - | - |
| Clinical suspicion | 3.14 [0.42-23.23] | 0.261 | 1.42 [0.17-11.62] | 0.745 |
| Volunteer | 5.19 [0.70-38.24] | 0.106 | 2.17 [0.27-17.38] | 0.463 |
| BMI | ||||
| ˂18.5 | 1 | - | - | - |
| 18.5-25 | 0.34 [0.14-0.81] | 0.015 | 0.37 [0.12-1.14] | 0.083 |
| 25.1-30 | 0.64 [0.25-1.62] | 0.355 | 1.12 [0.35-3.54] | 0.847 |
| ≥30 | 1.48 [0.58-3.79] | 0.41 | 1.70 [0.47-6.10] | 0.412 |
| High blood pressure | ||||
| Absent | 1 | - | - | - |
| Present | 2.01 [1.19-3.37] | 0.008 | 1.20 [0.62-2.33] | 0.591 |
| Taux de CD4 | - | - | - | - |
| ˂350 | 1 | - | - | - |
| 350-500 | 1.96 [1.00-3.82] | 0.047 | 1.71 [0.81-3.63] | 0.161 |
| >500 | 0,85 [0.30-2.40] | 0.758 | 0.76 [0.17-3.30] | 0.718 |
| Protease Inhibitor (PI) | ||||
| No PI | 1 | - | - | - |
| PI | 0.77 [0.37-1.59] | 0.494 | 0.62 [0.26-1.45] | 0.267 |
| Type of HIV | ||||
| HIV1 | 1 | - | - | - |
| HIV2 | 2.01 [0.62-6.47] | 0.239 | - | - |
| HIV 1 and 2 | 1.65 [0.59-4.60] | 0.332 | - | - |
| WHO Stadium | ||||
| Stage 1 | 1 | - | - | |
| Stage 2 | 0.76 [0.37-1.53] | 0.442 | - | - |
| Stage 3 | 0.63 [0.33-1,18] | 0.153 | - | - |
| Stage 4 | 0.98 [0.39-2.46] | 0.979 | - | - |
| ARV treatment | ||||
| Untreated | 1 | - | - | |
| Treated | 0.43 [0.15-1.29] | 0.114 | - | - |
Table 3: Risk factors for the occurrence of diabetes mellitus at Bobo-Dioulasso (Burkina Faso), 2008-2015.
This was a retrospective study and it had limitations. The absence of the variables "diabetes" and "diabetes treatments" in the database could lead to a classification bias with underreporting of diabetes mellitus cases. Possible data storage and transfer bias could be suggested for patients transferred from other health facilities. In fact, there is no solid interconnection between the different management structures and the absence of a pathology heading that does not classify AIDS on the patient transfer form. As the analysis is based on consultation data, we do not have some classic risk factors for diabetes in our database. However, these limitations inherent to most retrospective studies have not affected the quality of the results obtained, which have elicited comments from us.
Frequency of diabetes mellitus in the study population
The proportion of diabetics found in our study was higher than that reported by Sagna et al [13] (1.17%) and Sawadogo et al [14] (1.3%) and Dia et al [15] (1.2%). This could be explained by the longer and more recent period of our study; also the prevalence of diabetes mellitus in the general population is relatively increasing over the years [1]. However, the proportion reported by Henry et al [16] in Grenoble, France, which was about 3.9%, was higher than ours. This result could be explained by: the relatively younger age of our study population (average age 37 ± 10.1 years versus 56 ± 6 years); the non-completion of the diagnostic assessment of diabetes mellitus (measurement of glycated hemoglobin and Hyper Glycemia Per Os (HGPO)) could, to some extent, minimize the actual prevalence of diabetes in our study population. In addition, the prevalence of diabetes is higher in northern countries than in developing countries like ours [1,17]. The prevalence of diabetes in the general population of Burkina Faso (4.9%) was higher than in our study, as found in other sub-Saharan African countries [4,11,12,18].
Incidence of diabetes mellitus in the study population
Two studies conducted in 2000 and 2012 found incidences of diabetes mellitus in HIV-infected individuals of 1.53 and 1.55 per 100 person-years respectively, higher than the results of our study [19,20]. Justman et al found 1.50 per 100 person-years [21]; LO and Tripathi et al found 13.10 per 1000 person-years and 11.35 per 1000 person-years, respectively [22,23]. This lower incidence in our study could be explained by: the relatively younger age of our study population compared to these different studies. The existence of a difference in diagnostic techniques for diabetes mellitus in people with HIV; these different studies also included the measurement of glycated hemoglobin and HGPO. The biological monitoring of HIV-infected people, which is still weak in our countries compared to Western countries [12,24-27].
Risk factors for the onset of diabetes mellitus
Tien et al., Justman et al., and Tripathi et al., have identified advanced age and obesity as risk factors for the development of diabetes mellitus in people with HIV disease [19,21,23]. Sawadogo et al. noted in their study as risk factors for the occurrence of metabolic pathologies (such as diabetes), WHO clinical stage 3 and 4 and BMI ≥ 25.2 kg/m² [14]. Classic risk factors for the development of diabetes mellitus, such as age and obesity, are found in the general population as well as in the HIV-infected population [18,28]. In addition, other factors more intrinsic to HIV infection such as immunosuppression and the type of antiretroviral treatment have been described in several studies [12,25-27,29-32].
This study found a low incidence of diabetes mellitus among people with HIV compared to the general population. Nevertheless, there is a need for increased biological monitoring of diabetic HIV-infected individuals. This requires innovative strategies for biological monitoring and treatment protocols, and the strengthening of continuing education on diabetes and HIV/AIDS for healthcare workers. These efforts will contribute to improve not only the quality of life but also the survival of diabetic patients living with HIV. A case-control study aimed at identifying the various pathologies classified as non-AIDS and determining their risks of occurrence should be initiated.
Citation: Poda A, HJema A, Zoungrana J, Meda ZC, Kabore F, Sawadogo I, et al. (2020) Incidence and Risk Factors of Diabetes in People Living with HIV in Bobo-Dioulasso, Burkina Faso. 8:193. DOI: 10.35248/2329-8731.20.08.193.
Received: 09-Jan-2020 Accepted: 23-Jan-2020 Published: 30-Jan-2020 , DOI: 10.35248/2329-8731.20.08.193
Copyright: © 2020 Poda A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.