Journal of Developing Drugs
Open Access
ISSN: 2329-6631
ISSN: 2329-6631
Case Reports - (2022)Volume 11, Issue 2
Introduction: Hysterical paralysis is a kind of psychogenic disease and an uncommon disorder of uncommon type of conversion disorder. His diagnosis is difficult, and organic diseases that may cause corresponding disorders must be excluded. It is often associated with a trauma or a social event. Patient concerns: Here we report a case of 41 year old female who had continue neck and shoulder pain for 2 years.
Patient concerns: Here we report a case of 41 year old female who had continue neck and shoulder pain for 2 years.
Diagnosis: She happened to have hysterical paralysis after peripheral nerve block and improvement using physical therapy and antidepressant therapy. Interventions: During the event we recorded the characteristics of hysteria in detail, the slow recovery process of hysteria, the various examinations in the process, and analyzed several possibilities of possible problems. Finally, the diagnosis of hysteria made us unable to ignore the incidence of such symptoms in patients with pain.
Outcomes: We use acupuncture and rehabilitation therapy of traditional Chinese medicine to gradually restore the health.
Conclusion: This case indicated us patients with pain cannot ignore the emergence of hysteria. If they mistook organic diseases for traumatic intervention, it may lead to medical disputes
Hysteria paralysis; Cervical nerve root block; Trauma; Antidepressant therapy; Physical therapy
Hysterical paralysis, a formation of conversion disorder, which presents with the loss of sense and motor function [1]. It is often associated with a trauma or a social event [2]. The prevalence of the patients with conversion disorder, which is accompanied by pathological findings about the spine, is admitted to be 1%–3.8% [3]. Fishbain noted that virtually all patients with this problem complained of pain in the affected “paralyzed” part. It is possible that this phenomenon may not take place without the perception of pain on the part of the patient in the affected extremity [4]. So hysterical paralysis should be considered in patients with pain accompanied by unexplained limb paralysis.
A 41 year old female patient was admitted to the pain department due to continue neck and shoulder pain for 2 years. The pain was located in the back of the right neck and shoulder, which cover 5 to 6 cervical nerve distribution area, and radiation to the rear of the right upper limb, also She often described her right lower limb sored and distending, intermittently accompanied by walking instability. Pain points can be found in her right neck and back, and the strength of the limbs are no problem, and the pathological signs were all negative. Cervical magnetic resonance imaging showed that there were multiple segments of cervical disc herniation, and Computed Tomography showed cervical degeneration (Figure 1).
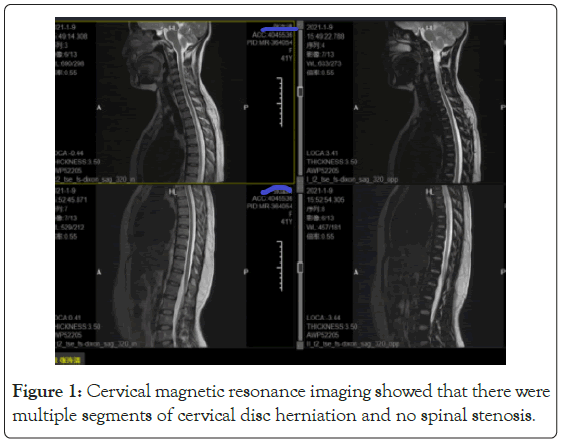
Figure 1: Cervical magnetic resonance imaging showed that there were multiple segments of cervical disc herniation and no spinal stenosis.
The 5 to 6 cervical intervertebral disc radiofrequency ablation was planned, and some symptoms were relieved after the operation, 2 days later the Peripheral nerve block and pain point injection were planned. The C6 transverse process of cervical vertebra was selected, and Thoracic erector spine muscle block, and Pain point injection. The drugs given were 0.25% lidocaine, compound betamethasone and vitamin B12 mixture total 10 ml, and each 2 ml. No abnormality was found during and after treatment.
9 hours later, the patient complained of general discomfort, such as acid distension and numbness. She also complained of numbness in his right hand and decreased muscle strength of his right lower limb. When she went to the toilet at night, she felt that his right lower limb was hard to walk and numbness seriously, in the morning and complained of numbness in her right upper and lower limbs. The muscle strength of the right upper limb decreased to 1-3 grades, (not stable all the time) and the muscle strength of the right lower limb decreased to 1-3 grades, and accompanied with hypoesthesia.
There was no hypoesthesia in the chest, bilateral sensation symmetry, tendon reflex, symmetrical existence of both upper limbs, and muscle tension are normal as same as both lower limbs, and paraplegia of single upper limb and single lower limb. MRI (Magnetic Resonance Imaging) examination of cervical vertebra was performed immediately (Figure 2). No structural abnormality was found. Routine blood exams showed no inflammatory or systemic disorder. Vital signs were stable.
Figure 2: MRI examination of cervical vertebra was performed immediately, cervical spinal cord signal were normal. There was no subcutaneous or subdural hemorrhage.
1 day later, the patient's symptoms aggravated progressively. Numbness appeared on the right chest, which was demarcated by the sternal midline. The left side was normal, and there was a sense of compression in the throat dysphonia happented. Numbness gradually affected the right face. Taking the nose as the demarcated line, Brain MRI+DWI (Diffusion Weighted Imaging) scan and Spine MRI+DWI scan were performed immediately again (Figure 3). Intracranial lesions and abnormalities of cervical spinal cord and nerves were not all found. Early spinal cord edema could not be excluded. Hormone, mannitol, vitamin B1 and B12 were given.
Figure 3: Brain MRI + DWI scan and spine MRI + DWI showed normal. Coronal plane of cervical MRI showed no edema signal of nerve emission and DWI showed spinal cord signal were normal.
CTA (Computed Tomography Angiography) angiography of the neck showed no abnormality blood routine and biochemical analysis are normal (Figure 4). The condition did not improve and aphasia appeared intermittently. Hysteria was considered.
Figure 4: CTA angiography of the neck showed no abnormality.
This patient was diagnosed as dissociative disorder and somatization disorder by psychiatrist, and gave olanzapine 5 mg before going to bed, and citalopram was orally taken 10 mg in the morning. 20 mg was given in the 3 days later. Language ability returned to normal. Combined with rehabilitation exercise, we also gave shock stimulation to the pain area, and the patient's limb muscle strength gradually recovered. The patient's limb muscle strength recovered, with upper limb grade 4 to 5 and lower limb grade 4. During this period, she repeatedly suffered from discomfort, abdominal distension and general numbness. After 20 days, her condition was stable, and her muscle strength recovered completely. Occasionally, she felt ant walking in her limbs, and her muscle strength reached grade 5. However, her walking posture was abnormal, she was improved and discharged from hospital. Electromyogram was also showed normal. After one month, she was followed up all patients returned to normal, and they were still given citalopram 20 mg and olanzapine 5 mg orally.
The diagnosis of hysterical paralysis should be cautious especial after treatment [5-9]. Conversion disorders have been observed in medical practice for many centuries but the exact cognitive and emotional processes as well as the underlying neurophysiological substrates remain poorly known [10-12]. Conversion is defined by the presence of neurological symptoms (such as Paralysis, Anesthesia, Blindness and so forth) that cannot be attributed to organic brain injury but appear to be triggered by particular emotional stressors or conflicts [11]. It is often associated with a trauma or a social event and complained of pain in the affected “Paralyzed” part. After analyzing the protagonist of this case, we found that she was disadvantaged economically, had limited education, and experience difficulty in expressing her distress. Her father was dead for hemiplegia in his 50 years. Her repeated pain area involved right arm and lower extremity before treatment, and numbness and nerve conduction abnormality caused by local anesthetic drugs after treatment made her emotion broken up, and anxiety obviously. Even through which can resulted in the emergence of hysteria paralysis [5-7]. The rear of paralysis is same as the hemiplegia of cerebral infarction what her father had [5]. Computed tomography, magnetic resonance imaging and electrodiagnostic studies are used to conform normal many times.
Peripheral nerve block usually be treated in pain medicine. Low concentration of local anesthetics, can break the vicious circle of pain effectively [13]. Compound vitamin B12 and small dose of steroid can reduce neuroinflammation, improve muscle tissue fatigue in innervated area. As for peripheral injection, intraneural injection or nerve bundle injection, it can be determined by visual ultrasound, but it is found that even intraneural injection will not necessarily lead to nerve injury [14], and the appearance of such visualization cannot reduce the incidence of nerve injury [15]. Does this mean that intraneural injection is not the cause of nerve injury? Ischaemia has been identified as one of the causes of peripheral nerve injury. Topical application of local anaesthetic to the rat sciatic nerve demonstrated acute reductions in peripheral nerve blood flow but no significant histological changes. Direct neurotoxicity of local anaesthetics is related to exposure to excessive concentrations or doses [16]. Although all local anaesthetic agents have some neurotoxic potential, it is likely that ropivacaine is less toxic than other agents such as lidocaine [17]. Further more introvescular injection also lead serious complication because of steroid. Use of observed blood in the needle hub to predict intravascular injections was 97% specific, but only 45.9% sensitive [13]. It showed repeated aspiration in the course of drug injection can improve the detection rate of steroid in blood. The infusion of steroid often leads to serious complications, especially for the particles on the blood vessels will lead to serious complications, such as spinal cord and brain infarction. Graham investigated 1340 patients into the cervical intervertebral foramen and found 78 cases of ridge plug in different parts. such as brain and spinal cord. Magnetic resonance imaging can find the infraction quickly in 24 hours. When encountering a patient with paralysis, therefore imaging and electrophysiological studies are often necessary, but costly. Our MRI result showed normal (Figure 3). Electromyography of muscles and nerves was consistent the same with that before operation, which finally excluded the complications of nerve block and steroid intravascular injection. Hysterical paralysis was considered made clearly.
According to research, hysterical paralysis usually takes 6 months to recover completely, and some patients still have residual pain problems.
In this case, we treated used antianxiety drugs and antidepressant drugs, and applied rehabilitation treatment. The patient's muscle strength recovered completely in 3 weeks. Yongquan acupoint stimulation therapy is also used in traditional Chinese medicine. We have also combined this method in this patient (Figure 5).
Figure 5: Yongquan acupoint stimulation therapy is also used in traditional Chinese medicine.
After this case, we must pay attention to hysterical paralysis for patients with non-organic paralysis. Special for pain patients. Preoperative psychological state assessment is also particularly important, whether the adjustment of psychological state should be carried out before treatment, and whether traumatic operations such as surgery or nerve block can be regarded as an aggravating factor are still worth considered. This study was approved by the Ethics Committee of the First Hospital of Jiaxing and conducted in accordance with the Declaration of Helsinki. Signed informed consent was obtained from the patient before surgery.
Citation: Ma L, Yao M (2022) Hysteria Paralysis Happened after Cervical Nerve Root Block Treatment: A Case Report. J Develop Drugs.11: 165.
Received: 25-Jan-2022, Manuscript No. EOED-22-16013; Editor assigned: 28-Jan-2022, Pre QC No. EOED-22-16013 (PQ); Reviewed: 11-Feb-2022, QC No. EOED-22-16013; Revised: 16-Feb-2022, Manuscript No. EOED-22-16013 (R); Published: 28-Feb-2022 , DOI: 10.35248/2329-6631.22.11.165
Copyright: © 2022 Ma L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited