Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Case Report - (2022)
Male breast enlargement as a result of increase in the amount of glandular breast tissue is referred to as Gynecomastia. It may be due to multitude of causes like drugs, endocrine diseases, physiological enlargement or systemic diseases. Androgen Insensitivity Syndrome (AIS) is one such condition which occurs due to a mutation in the androgen receptor gene. It is a disorder of male sexual differentiation and may presents as gynecomastia in a patient with a karyotype of 46 XY. Phenotypically it can be partial, complete or mild and can present among both men and women as infertility with ambiguous genitalia. In this case report we present a male with gynecomastia later identified as partial androgen insensitivity syndrome.
Androgen insensitivity; Gynecomastia; Karyotype
Benign increase in the size of male breast as a result of proliferation of glandular tissue is referred to as gynecomastia. It may occur physiologically in both the young and elderly. In young it is important to recognize important conditions that may otherwise produce this finding as in testicular tumors, Klinefelter’s syndrome, androgen insensitivity syndrome or primary hypogonadism. This case report focuses on a patient with partial androgen insensitivity syndrome who presented to the hospital with gynecomastia.
A male, 17 years of age presented to the hospital with symmetrical increase in breast size since 3 years. He struggled with initiating conversations and maintaining eye contact since he was socially uncomfortable.. He avoided outdoor physical activity, had few friends and withdrew from social events at school. Developmentally he attained his milestones at a normal age. On examination his height was 168 cm, weight was 60 kg with a body mass index of 21.26 kg/m2. His pulse was 74 beats per minute,blood pressure was 130/90 mmHg, respiratory rate was 24 beats per minute. Both breasts showed symmetrical enlargement (Tanner stage VI),pubic hair was noted (Tanner stage III), testes had a volume of 15 mL (Tanner stage IV) and micropenis was present (Figure 1).
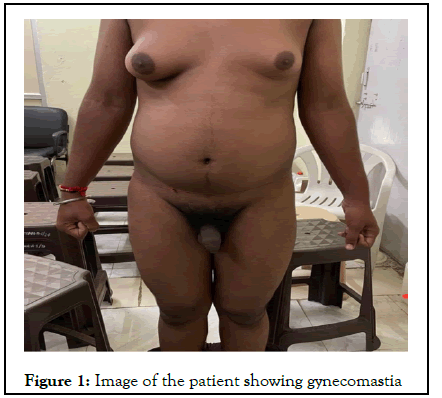
Figure 1: Image of the patient showing gynecomastia
Routine investigations including complete blood count, liver function test, renal function test, blood sugar levels, urine routine and microscopy were within normal limits. The patient was evaluated endocrinologically and was observed to have a serum testosterone of 178 ng/dl (normal range 132-813 ng/dl, Luteinizing Hormone (LH) level of 13.10 mIU/ml (normal range 2.56 to 12.1), Follicle Stimulating Hormone (FSH) level of 2.50 mIU/L (normal range, 1.5 to 9.74), estradiol level of 58.5 pg/ml (normal range, 5.37 to 65.9 pg/ml), β-human Chorionic Gonadotropin (β-hCG) level of 2.39 IU/L ( >25mIU/ml), prolactin of 13.1 ng/L (normal range, 3.7 to 17.9 ng/ml), free T4 level of 1.92 pmol/L (normal range, 0.78 to 2.19), and thyroid stimulating hormone level of 1.7 mIU/L (normal range, 0.465 to 4.68). An ultrasound of the testis was done; the left testis was 4 ×1.9 × 1.7 cm and the right testes were 3.8 × 2 × 1.9 cm. The seminal vesicles and prostate glands were normal in echogenicity and size. An ultrasound of the abdomen and pelvis showed no significant abnormality. MRI brain was done which had no obvious abnormalities. Karyotyping was done with 46 XY identified as the karyotype (Figure 2). Androgen receptor gene mutation was identified using PCR technique. A reduction mammoplasty was done which was uneventful with no post operative complications (Figure 3).Following this the patient was discharged and was followed up in the outpatient clinic.
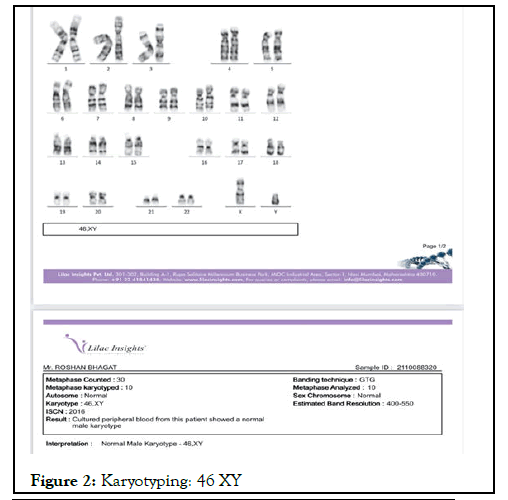
Figure 2: Karyotyping: 46 XY
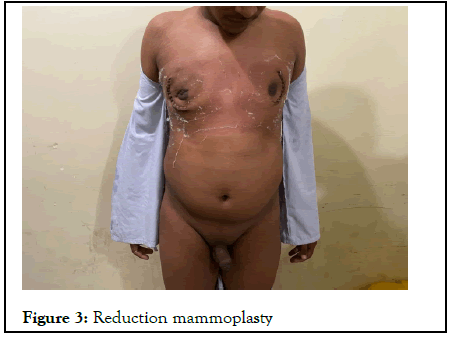
Figure 3: Reduction mammoplasty
Gynecomastia is identified clinically by a rubbery or firm mass that extends concentrically around the nipple as a result of proliferation of the glandular tissue in male breasts. It may occur at any age due to a variety of causes with primary androgen insensitivity as one of the many possibilities [1]. There is imbalance between in the actions of free androgen and free estrogen. In the breast tissue [2]. Physiologically it occurs most commonly among infants followed by adolescents and then the elderly. It may be secondary to drugs that supplement exogenous estrogen like oral contraceptives, tamoxifen or estrogen creams. It may also occur following anti androgen therapies with drugs like finasteride or bicalutamide. Ketoconazole, digitalis, cimetidine and tri cyclic anti-depressants are some examples known to produce gynecomastia. Condition like cirrhosis of liver, chronic pulmonary diseases, chronic kidney disease, hyperthyroidism and certain malignancies may produce an enlargement in the breast tissue. Testicular tumors, Klinefelter’s and androgen insensitivity syndrome though rare are important conditions to rule out when evaluating a case of gynecomastia [3]. Idiopathic gynecomastia may also be encountered in some cases [4]. In our case most normal complete blood counts, renal and liver function test rule out liver cirrhosis and chronic renal disease. Thyroid function tests weren’t suggestive of hyperthyroidism and imaging modalities like MRI brain, USG abdomen and pelvis and an ultrasound of the scrotum were unremarkable. FSH was normal while estradiol and LH levels were raised making AIS a likely possibility as compared to primary hypogonadism [5]. AIS are of 3 phenotypes mild, complete and partial. Mild AIS is rare and presents in Males with infertility or as Kennedy’s disease (bulbar and spinomuscular atrophy). Complete AIS presents in females with inguinal swellings in infants or primary amenorrhea. Pubic and axillary hair may be absent or present in small amounts. The vagina may vary in size being a small dimple or normal in length. The rest of the secondary sexual characters are normal. The proximal part of the vagina, cervix and uterus are absent due to the release of anti-Mullerian hormone from Sertoli cells of testis which may or may not be inguinal. Partial AIS may have varied presentation like gynecomastia, infertility, bifid scrotum, micropenis and hypospadias. Another form may present with normal female external genitalia with clitoromegaly [6]. Our patient presented with gynecomastia and micropenis. Due to the presence of micropenis and ambiguous genitalia at birth mild AIS was ruled out with partial AIS as the likely possibility. Androgen receptor gene is located on the X chromosome at Xq11-12. Most mutations are germ line mutations and are located in the ligand-binding domain. There are 4 functional domains namely- a central DNA-binding domain, an aminoterminal domain and a C-terminal ligand binding domain and a hinge region containing the nuclear targeting signal [7]. In our case a direct PCR sequencing was done which was indicative of partial AIS. Patient with partial AIS are most commonly raised male. Gynecomastia may occur at puberty which requires mammoplasty. In patients that are designated as female and gonadectomy and genitoplasty needs to be done to avoid virilization. Androgen replacement in males and estrogen replacement in females is required at puberty. Psychological distress is common among such patient. Germ cell tumors are more common in partial AIS than complete AIS [8-10].
In Complete AIS patients are feminine and are raised as females. Estrogen replacement therapy following a gonadectomy may be a necessity in such patients as chances of tumours increase in patients over 50 years of age. It is therefore it is essential to completely evaluate a case of gynecomastia. A multitude of factors are responsible for this finding with clues present both on physical examination and on laboratory investigations. In patients with normal FSH but raised LH and estrogen AIS should be considered.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: Acharya S, Bawiskar N, Shukla S, Kumar S, Shinde R (2022) Gynecomastia in a Patient with Partial Androgen Insensitivity Syndrome. Andrology. S1:005.
Received: 16-Feb-2022, Manuscript No. ANO-22-16584; Editor assigned: 19-Feb-2022, Pre QC No. ANO-22-16584(PQ); Reviewed: 05-Mar-2022, QC No. ANO-22-16584; Revised: 12-Mar-2022, Manuscript No. ANO-22-16584(R); Published: 19-Mar-2022 , DOI: 10.35248/2167-0250.22.S1.005
Copyright: © 2022 Acharya S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO