Medical & Surgical Urology
Open Access
ISSN: 2168-9857
ISSN: 2168-9857
Case Report - (2021)Volume 10, Issue 8
Self-mutilation is a rare situation including all practices leading to tissue or organ damage, with a vital or functional risk without intent of suicide. It is most often observed in vulnerable psychotic conditions, particularly schizophrenia. The diagnosis of self-mutilation is clinical and its management requires collaboration between the urologist and the psychiatrist. We report two cases of genital self-mutilation in our clinic.
Self-mutilation; Strangulation of the penis; Urethral meatus stenosis
Self-mutilation includes all practices leading to tissue or organ damage, with a vital or functional risk without intent of suicide [1]. This is a rare situation often occurring in the context of an underlying psychotic condition. Management requires collaboration between urologist and psychiatrist [2]. We report two cases of genital self-mutilation in our clinic.
Patients 1
It was about a 29-year-old male patient with no previous medical history who was seen in the emergency department for acute urinary retention after putting a ring around his penis. The patient was seen 13 hours later after the strangulation of the penis. The anamnesis did not reveal any psychotic history or drug use.
The physical examination revealed: a tense and painful distended bladder on palpation; a very tight metal ring threaded around the penis, located 2cm distal the root of the penis. The strangulation was responsible of a swelling of the penis downstream of the strangulation up to the level of the glans without any sign of necrosis while the upstream portion was normal in appearance.
The ring was removed with a metal saw after interposing a protective metal between the ring and the penile skin.
The removal of the ring allowed the patient to empty his bladder; there was neither urethrorrhage nor haematuria. He was put on medical treatment based on analgesics and anti-inflammatories. A regression of the inflammation was obtained on the 2nd day and the patient was discharged on post-operative day 3 with a referral to a psychiatrist for further management (Figure 1 and 2).
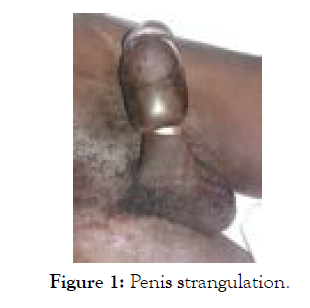
Figure 1: Penis strangulation.
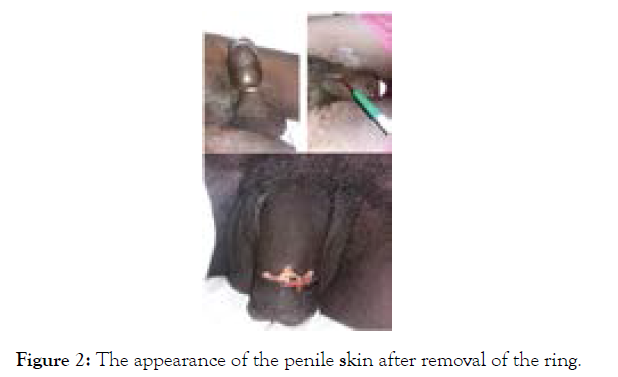
Figure 2: The appearance of the penile skin after removal of the ring.
Patient 2
A 49-year-old patient was referred to us with lower urinary tract symptoms including frequency and difficulty passing urine characterized by inability to empty the bladder and straining. The anamnesis revealed that the patient was undergoing psychiatric treatment (haldoloperidol) and a notion of complete sectioning of the penis which had required an urethroplasty six years previously. The examination revealed an alteration in his general status WHO 2, mucous membranes paleness, absence of a penis with stenosis of the neo urethral meatus and a discrete painless distended bladder. The testicles were in intrascrotal position with a normal appearance. Urine culture did not reveal any urinary tract infection. The ultrasound examination of the urinary tract revealed an intravesical mass measuring 81 × 6.5 × 7.2 mm in its postero-inferior diameter with a stage 4 right uretero-hydronephrosis.
The patient underwent emergency dilation of the urethral meatus and placement of a transurethral catheter to drain hematic urine; he was then followed for his bladder tumor (Figure 3 and 4).
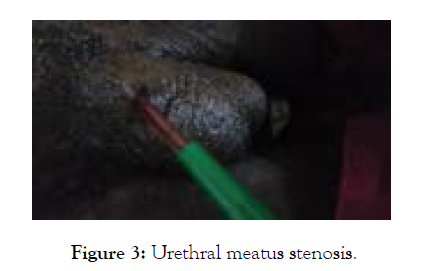
Figure 3: Urethral meatus stenosis.
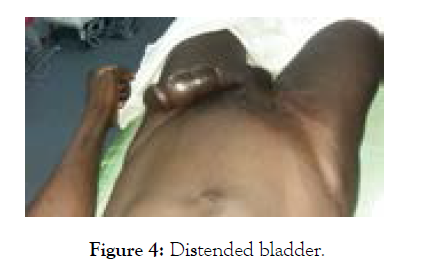
Figure 4: Distended bladder.
The incidence of self-injurious behavior is not well known, and is usually not reported by the patient or the family. Its prevalence ranges from 1 to 4% in America and between 4.6 and 6.6% in the United Kingdom [2]. It can be the consequence of various pathologies and is not pathognomonic of any particular condition [3]. However, self-mutilation is most often observed in vulnerable psychotic conditions, particularly schizophrenia, but can also be secondary to depressive disorders, personality disorders or mental retardation [4]. This state of psychotic vulnerability was established in one of our patients after complete sectioning of the penis that was diagnosed as schizophrenic and put on neuroleptic medication (Haloperidol). These psychotic patients experience profound genital confusion with feelings of low self-esteem, loss of the notion of physical integrity, rejection of the penis, and the sensation of being a woman [5]. Other factors are also incriminated in self-mutilation such as alcohol abuse [6] and narcotic (drug) use. Different organs can be affected to varying degrees in male genital self-mutilation. Removal of the testicles is the most common assault, followed by laceration of the scrotal or penile skin and finally sectioning of the penis [7]. In our study the penis was the organ involved and the testicles were spared in both cases. The diagnosis of self-mutilation is clinical, the consultation time is generally less than 6 hours, and the family and friends are alerted by the haemorrhage occurring after sectioning an organ, which leads the patient to seek urgent medical attention. In the case of strangulation of the penis, as was the case with one of our patients, edema of the penis, difficulty passing urine or urinary retention is the reasons for referral [8]. Strangulation can lead to complications such as penile tumefaction, amputation, urethral fistula or Fournier's gangrene [9]. These complications are related to the material used, the duration of the strangulation and the severity of the stricture. The management of our first patient was strait forward by removal of the ring which prevented these complications.
Re-implantation of the penis is recommended after penile section, despite a maximum delay of 6 hours allowed for this, as per authors, with microsurgery, it can be attempted up to 24 hours in case of ischemia [10]. The repair must concern the urethra as well as the vascular and nerve structures and the corpora cavernosa [11]. A cutaneous ureterostomy is indicated in case of impossibility or failure of penile re-implantation. Our second patient did not have a re-implantation of the penis; this could be explained by the non-availability of microsurgical material or the poor conditions of conservation and transport of the amputated penis which do not guarantee the success of the re-implantation. Ureterostomy can be complicated in the long term by stenosis responsible for symptoms of the lower urinary tract, which is observed in the second patient. The prognosis of self-injury is poor, due to resistance to treatment and the permanent risk of recurrence [12] even if the patient is under psychotropic treatment.
Genital self-mutilation is most often encountered in young adults and is characterized by its rarity and an underlying psychiatric condition, particularly schizophrenia. Its management requires collaboration between the urologist and the psychiatrist. The prognosis of these patients is unfavorable because of the risk of recurrence, but also of the irregularity observed in their follow-up, which can lead to the late discovery of long-term complications such as the stenosis of the cutaneous urethrostomy encountered in one of our patients.
Citation: Traore A, Jalloh M, Mboji MM, Diallo A, Thiam NM, Diaw EM, et al. (2021) Genital Self-Mutilation: Report of 2 Cases. Med Surg Urol 10:259.
Received: 04-Aug-2021 Accepted: 20-Aug-2021 Published: 27-Aug-2021 , DOI: 10.35248/2168-9857.21.10.259
Copyright: © 2021 Traore A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.