Case Report - (2023)Volume 8, Issue 4
Langerhans Cell Histiocytosis (LCH) is a rare condition with an unknown etiology and variable manifestations that include lung infiltrates, bone lesions, rashes, endocrine, hematopoietic and hepatic dysfunction. It results from neoplastic proliferation of Langerhans cells. Eosinophilic Granuloma (EG) is considered a localized form of the disease.
Here, we report a case of a 5 year-old female patient who presented with a left frontal 3 cm non-tender swelling that had grown rapidly during 2 months. Head Computed Tomography showed a 3 cm lytic bone lesion, while head Magnetic resonance imaging showed extra-axial space occupying lesions with irregular borders and meningeal infiltration. The patient was hence diagnosed with Eosinophilic Granuloma of the skull one year after she was hit on her left frontal skull with a hammer, without a history of hemorrhage or fracture. Total excision was performed through cranioplasty, and full investigations were done to rule out systemic involvement that were all free.
To conclude, EG should be considered in pediatric patients with a history of head trauma even without trauma complications.
Eosinophilic granuloma; Head trauma; Pediatric; Cranioplasty
Langerhans Cell Histiocytosis (LCH) is a rare unifocal or multifocal disorder of the bone and soft tissue, most often appearing as a lytic lesion of the skull [1]. The mildest and most common form is Eosinophilic Granuloma (EG), also known as unisystem Langerhans Cell Histiocytosis (LCH). It is a benign bone lesion with an unpredictable outcome. It can affect children, adolescents, and young adults, and the most commonly involved site is the skull, however, it can involve any organ or system in the human body [2]. Pathologic characteristics of this disease; include clonal proliferation of mononuclear antigen presenting cells from bone marrow [3,4].
The incidence of EG in children -less than 15 years- is 4 to 5 cases per million per year, while in adults, the incidence is 1 to 2 cases per million per year [5]. Males are more commonly affected than females with poorly understood pathophysiology and no recognized pattern of inheritance for the disease.
The most common sign of EG is a tender, enlarged scalp mass on the parietal and frontal bones. However, EG may be asymptomatic and only discovered incidentally on a skull X-ray [1].
In order to differentiate EG from similar conditions; like infections, malignancy and other benign tumors, with the same clinical presentation and laboratory findings, histopathological examination is required [6].
Treatment options; include operative and non-operative choices, depending on the patient’s condition and the location of the tumor [6].
According to the literature, spontaneous regression and recurrence after surgical excision have been reported [4]. Herein, we report a case of EG post head trauma in a pediatric patient treated with excision and cranioplasty successfully.
A previously healthy 5 year-old female who was born to healthy 1st degree cousins, presented to hospital after her mother noticed a left frontal swelling with a “defect” sensation on palpation reaching the periorbital area with mild discomfort and pain.
The swelling had grown gradually over a 2 month duration, with a history of ill-being, feverish sensation, severe loss of appetite with undocumented weight loss, and behavioral changes; including aggressiveness and irritability.
There was no skin rash, ear discharge, diarrhea, polydipsia, change in activity level, or dyspnea.
The only related past history is that the patient was hit with a hammer by her brother on her left frontal area 1 year prior to presentation. At that time, she had no loss of consciousness, headache, vomiting, pain, swelling or any major consequences, hence, she didn’t undergo any imaging studies after the incident and remained asymptomatic until her presentation one year later.
On physical examination, the patient was well, not distressed, glascow coma scale was 15/15, her neuro-examination was unremarkable, and her abdomen was soft and lax.
There was a 3 cm, nontender swelling that was soft in consistency with diffuse smooth border and step-down deformity. No crepitus, paresthesia, pulsation, redness or local rise in temperature were appreciated on palpation.
There was no skin or scalp rash, no jaundice, pallor, edema, lymphadenopathy, ear discharge, orbital or ocular abnormalities, no gum or palatal lesions, and no palpable ascites, or organomegaly.
Radiological investigations showed a bony lytic lesion on head Computed Tomography (CT) Figure 1 and left frontal extra-axial space occupying lesion on MRI (Figure 2).
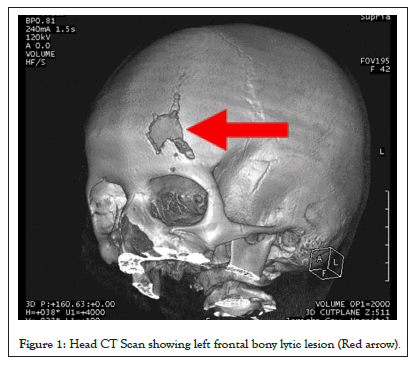
Figure 1: Head CT Scan showing left frontal bony lytic lesion (Red arrow).
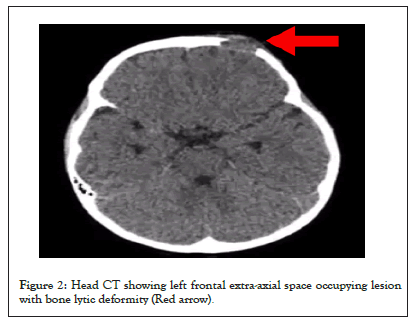
Figure 2: Head CT showing left frontal extra-axial space occupying lesion with bone lytic deformity (Red arrow).
According to her clinical presentation and CT findings, she was referred to the neurosurgical department in a tertiary center for excision and cranioplasty where biopsies were taken.
Pathology reports from biopsies showed neoplastic cells that were positive for Cluster of Differentiation 1a (CD1a), Langerin and s100, consistent with Langerhans Cell Histiocytosis (Figures 3 and 4).
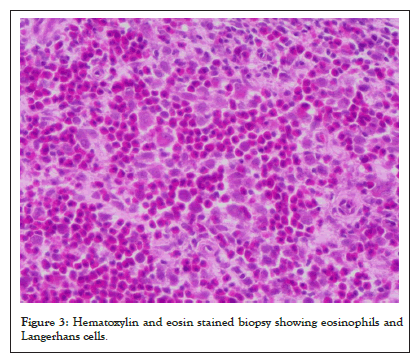
Figure 3: Hematoxylin and eosin stained biopsy showing eosinophils and Langerhans cells.
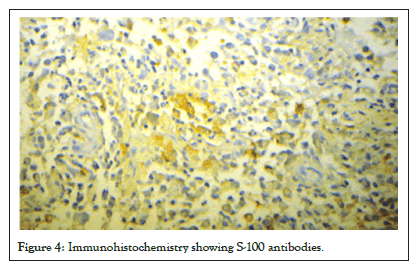
Figure 4: Immunohistochemistry showing S-100 antibodies.
The patient was discharged 5 days post-op and remained in remission with no complaints. Follow-up visits were scheduled to monitor her recovery progress, including evaluation of the incision site, assessment of any potential complications, and checks for any neurological deficits. The patient was advised to follow post- operative care instructions, including avoiding strenuous activity and heavy lifting, and taking prescribed medications.
The pathophysiology of LCH remains controversial and is still unknown. Although recently, most studies agreed that it is a neoplastic process rather than a reactive process due to the recent discovery of activating v-raf murine sarcoma viral oncogene homolog B1 (BRAF) mutations in LCH cells. LCH is a clonal proliferation of Langerhans cells, often associated with lymphocytes, eosinophils, macrophages, and giant cells. BRAF mutations, usually V600E, have been reported in 40%-70% of cases, and recently, MAP2K1 mutations have been reported in BRAF-negative cases [7].
A thorough review of the published EG cases that were related to moderate-to-severe trauma provided various theories that most likely explains this correlation. As mentioned in (Clayton et al. 2017), genetically predisposed persons affected in LCH respond in an exaggerated way to exposure of environmental triggers, (trauma as in our case) compared to their normal phenotype. Together, this stimulates the Notch1 signaling pathway which had cleavage mediated cell-cell communication, associated with tissue growth, cancer, cell death and tumor suppression [8].
On the other hand, another hypothesis proposed other explanations like defected adaptive immune response instructed by LC and T Lymphocytes that release Monocyte Chemoattractant Protein-1 (MCP-1) and C-C Motif Chemokine Receptor 2 (CCR2) in response to blunt injury [9].
Another hypothesis was the involvement of Myeloid Differentiation primary response (MyD88). This protein functions as an essential signal transducer in the interleukin-1 and Toll-like receptor signaling pathways. These pathways regulate the activation of numerous proinflammatory genes [10].
In addition, immune interaction between the clonal proliferation of dendritic cells and T cells leading to a “cytokine storm”. Uncontrolled cytokine production induced by the traumatic process may contribute to transformation of precursor cells into pathologic Langerhans cells.
In our case, the patient developed LCH in the frontal area after a traumatic injury, which was successfully managed with cranioplasty. However, the fact that the patient presented with LCH one year after the traumatic event raises the question of whether the tumor was actually caused by the trauma or if it was a pre-existing condition that was exacerbated by the injury.
After conducting a thorough review of the literature, it was found that the longest reported time interval between an injury and tumor presentation in cases of post-traumatic Langerhans cell histiocytosis was 9 months (Table 1) [2,9-17].
| Case | Age | Sex | Trauma | Time between trauma and simptoms |
|---|---|---|---|---|
| 1 | 10 years old | Male | Head trauma(struck of his head on horizontal metallic bars) | One month and 3 days |
| 2 | 16 months | Male | Blunt orbital trauma (swelling of the left upper eye lid) | Four weeks |
| 3 | 53 years old | Male | Burr holes (by neurosurgeon) | Seven months |
| 4 | 15 year old | Male | Head trauma(he had been hit by a baseball on the left side of his forehead) | Nine months |
| 5 | 4 years old | Male | Fall from 50 cm heightwith bruises on the temple | One month |
| 6 | 8 years old | Male | Hit while practicing Judo on his right parietal area | Two months |
| 7 | 4 years old | Male | Head trauma (was hit by his brother) | Four weeks |
| 8 | 31 years old | Female | Blunt head and chest trauma | Two months |
| 9 | 4 years old | Female | Head trauma | One year |
| 10 | 2 years old | Male | Occular trauma | Three years |
| 11 | 10 years old | Male | Head trauma with 2 injuries | Two months |
| 12 | 8 years old | Male | Head trauma | Three months |
Table 1: Summary of cases of EG with a prior trauma.
This suggests that in most cases, the tumor tends to present within a relatively short time frame following the traumatic event. However, it is important to note that each case is unique and the time interval between injury and tumor presentation may vary depending on individual factors. Therefore, close monitoring and evaluation of patients who have experienced a traumatic event is crucial in order to promptly diagnose and manage any potential complications.
The exact etiology of EG is unclear. In the present case, trauma without hemorrhage or fracture can trigger the development of EG. The interval from the trauma to EG occurrence was 1 year, and this was quite the longest period compared to previous reports. Our case suggests that minor trauma may be an aggravating factor for the progression of EG. Clinicians should be aware of a possible association between solitary EG of the skull and minor head trauma. Eventually, we would like to address the following Research question that requires further data collection and analysis: Does exposure to trauma precede and induce the occurrence of LCH? Is there a strong association between moderate to severe trauma and subsequent occurrence of LCH?
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Abu-Hilal LH, Njoom YM, Barghouthi DI, Thraiee YA, Mtour S (2023) From Trauma To Histiocytoma: Post-Traumatic Eosinophilic Granuloma in a 5-year-old Female. Immunogenet Open Access. 8:220.
Received: 03-Nov-2023, Manuscript No. IGOA-23-27223; Editor assigned: 06-Nov-2023, Pre QC No. IGOA-23-27223 (PQ); Reviewed: 20-Nov-2023, QC No. IGOA-23-27223; Revised: 27-Nov-2023, Manuscript No. IGOA-23-27223 (R); Published: 04-Dec-2023 , DOI: 10.35248/IGOA.23.8.215
Copyright: © 2023 Abu-Hilal LH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.