
Journal of Perioperative & Critical Intensive Care Nursing
Open Access
ISSN: 2471-9870

ISSN: 2471-9870
Research - (2021)Volume 7, Issue 1
Heart surgery encompasses not only physical concerns but also long lasting psychological harms depleting postsurgery quality of life. Complementary therapies as progressive muscle relaxation (PMR) is undertaken to decrease the fatigue and improve the quality of sleep among these patients. This study was undertaken to assess the effect of PMR on sleep quality and fatigue among these patients. Randomized controlled design was undertaken, 33 patients in experimental group and 32 patients in control group were selected. Quality of life and fatigue was assessed using standardised questionnaires before surgery, post surgery at 2 weeks and 6 weeks. Experimental group was provided with PMR program preoperatively. Statistically significant reduction in fatigue, sleep quality improvement at 6 week (p<0.05) and no significant reduction in fatigue (p-0.797) and sleep quality improvement was noted at 2 week (p- 0.822). Benefits of PMR are established with the findings of the present study. PMR is an effective way to ease the patient’s journey from a major surgery to routine life with less of pharmacological dependence.
Valvular heart surgery, Progressive muscle relaxation, Fatigue, Quality of sleep
Worldwide, cardiovascular disorders pose the greatest health hazard. According to WHO, the specific cardiovascular conditions are as rheumatic heart disease, ischemic heart disease, hypertension, stroke, cardiomyopathy, myocarditis, endocarditis, congenital heart disease and other circulatory disorders [1,2]. Due to rising chronic disease burden, there is upsurge in cardiac surgeries and catheter based interventions being performed as well as there are various innovations in form of minimally invasive cardiac operation, cardiac bypass techniques [3,4]. Cardiac surgeries in themselves are unique and contribute to significant morbidity [4]. Coronary Artery Bypass Graft (CABG) remains the most commonly performed cardiac surgical procedure followed by Valvular Heart Disease (VHD) [5]. The epidemiology of VHD has changed significantly over the past 50 years in developed countries [6]. Major etiologies of VHD include rheumatic, degenerative, traumatic, congenital, and infectious heart diseases [7]. In India, rheumatic fever is labelled as malignant causing multivalve involvement [8]. Rheumatic heart disease (RHD) is leading non-communicable lethal disease in low and middle income countries accounting for 1.4 million deaths per year and has serious complications as atrial fibrillation, infective endocarditis etc. [9]. Major VHDs are stenosis and regurgitation, aortic stenosis and mitral regurgitation remains the most common lesion requiring surgical intervention [10]. Recommended medical treatments may slow the rate of functional deterioration but physiological and hemodynamic changes later in the disease course, indicates surgical repair or replacement of the diseased valve although minimally invasive therapies as balloon valvuloplasty, trans-catheter aortic valve replacement, Mitraclip technique are also indicated, if patients are not unsuitable for the surgery [11-13]. Surgery performs a major role in treatment of VHD. Returning to normal life after cardiac surgery poses a huge physical, mental and social challenge. Major complaints experienced after cardiac surgery are reported as post-operative pain, decreased quality of life, arrhythmia, electrolyte imbalance, infections, systemic problems and anticoagulation related issues [14]. After surgery, these patients are vulnerable to develop the depression, anxiety, post traumatic stress disorder, depleted quality of life, fragility, psychological stress related to scarring, body image, sexual life, parenting, medicines, treatment and disease course [15].
Deprivation of total sleep time, decreased sleep efficiency, fragmented sleep, and increased daytime napping has been reported in numerous studies [16,17]. Sleep returned to the normal levels by the eighth recovery week after surgery [18]. Findings suggest that management of major symptoms and control of the patient's sleeping environment as well as psychological care after discharge may improve patient condition [19]. Fatigue is a universal complaint in cardiac population. It peaks between 2 to 4 weeks postoperatively. Fatigue is strongly associated with low levels of independent functioning, great emotional distress, depression and poor cardiac function [20-23]. Preventive management for sleep and fatigue should be undertaken especially during first 6 months after discharge. Complementary therapies as PMR are modalities for assisting these patients to recover from the postoperative complications. Relaxation therapies have a great impact in improving sleep quality and reducing anxiety as well as there are documented benefits of their effectiveness in pre and post-operative period of patients with stoma surgery, hysterectomy, advanced cancer, multiple sclerosis, haemodialysis and chronic obstructive pulmonary disease [24,25] and cardiac surgery as well [26,27]. PMR was developed by Jackson in 1929, it involves voluntary tensing and relaxation of major muscle group progressively in a pattern for defined time duration and its benefits include stress reduction, improved sleep quality, relieving pain and muscle tension [28]. The need for using PMR therapy as an alternative therapy for reducing anxiety, fatigue and improving quality of sleep among heart surgery patients was felt imperative, especially in a tertiary care hospital where the need for an integrative approach to health care plays an important role.
Quantitative approach, randomised controlled design (time series) was selected. Inclusion criteria were as adult patients (Age>18years) admitted at preoperative cardiac ward who were able to follow the instructions provided in hindi or english and were willing to participate in the study. Exclusive criteria were as patients suffering from syndromal psychiatric illness, recently underwent any relaxation training including progressive muscle relaxation, getting psychotrophic drugs, history of musculoskeletal and neurological disorders, severe liver and renal dysfunction, impaired hearing. Sample size was calculated as 60 subjects, 30 in each group based on statistical analysis of pilot study at α=5% and power 80%. Consort diagram shown in Figure 1. Purposive sampling with random allocation of subjects into control and experimental group using sequentially numbered opaque sealed envelopes. Data collection tools were as subject data sheet, Pittsburgh sleep quality index (PSQI), Fatigue assessment scale and activity log sheet.
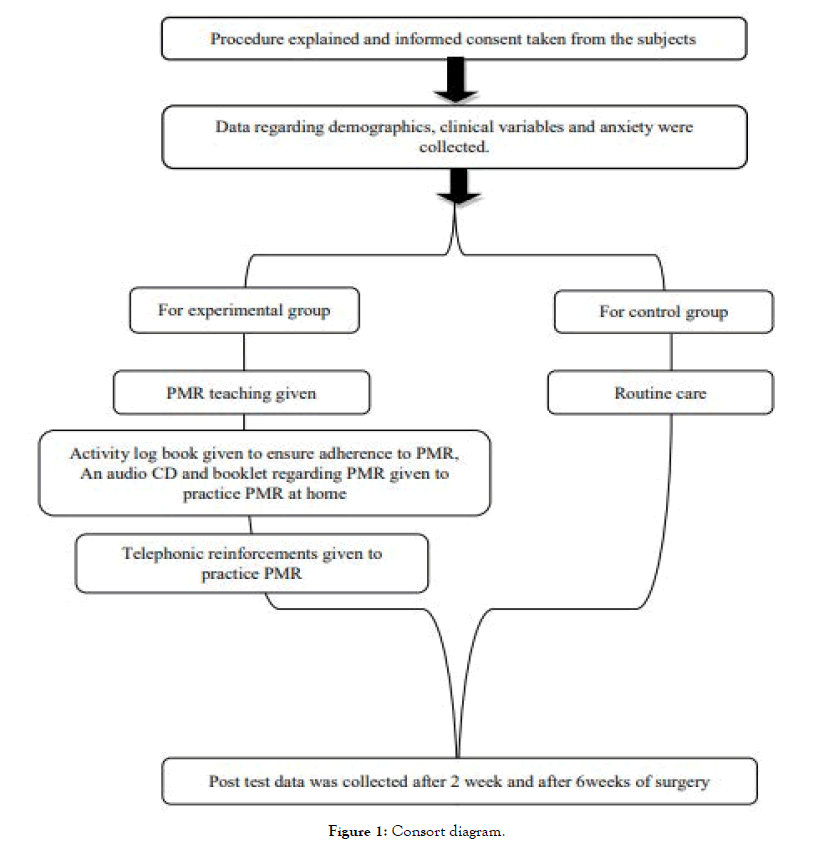
Figure 1. Consort diagram.
Tool 01 was subject data sheet and has two sections- sociodemographic (consists of age, gender, education, marital status, place of residence, family type, occupation and socio economic status) and clinical profile (consists of diagnosis, duration of disease, name of surgery, previous history of any surgery and co morbidities). This tool was developed by researcher. Content validation was established by 2 medical and 3 nursing experts. Necessary changes were incorporated as per the expert’s suggestion. Cronbach alpha was found to be 0.83 using test-retest methods. Tool 02 was Pittsburgh sleep quality index (PSQI). It was a standardized tool developed by Buysse DJ used to measure quality and patterns of sleep in the older adults. It differentiates poor from good sleep by measuring 7 domains- Subjective sleep quality, Sleep latency, Sleep duration, Habitual sleep efficiency, Sleep disturbances, Use of sleep medication, and daytime dysfunction over the last month. Scoring of the answers was based on a 0-3 scale, where by 3 reflect the negative extreme on the likert scale. A global sum of 5 or greater indicates a poor sleeper. The tool has high internal consistency with cronbach alpha of 0.83. Tool 3 was fatigue assessment scale; it was a self developed rating scale consisting of 10 items (which measures fatigue of a person during various activities in a week in terms of physical, social, psychological and spiritual domains and its relationship with time of the day). Scores from 0 (no fatigue) to 10 (worst possible) with a total score range of 0 to 100. No fatigue, very little, mild, moderate, severe, worst denotes 0, 1-9, 10-30, 31- 60, 61-80, 81-100 respectively. Content validity was established by 2 medical and 3 nursing experts. Necessary changes were incorporated as per expert’s suggestion. Inter-rater correlation co efficient was 0.81. Tool 4 was activity log book. It was a structured activity log book prepared for checking the adherence of the experimental group subjects to progressive muscle relaxation. All tools were translated to Hindi with the help of language experts from Hindi section, and back translation to English was done to ensure original meaning was not lost during translation.
Intervention- progressive muscle relaxation
1. The whole process of this relaxation takes approximately 15 min.
2. Lie down comfortably on a bed facing upward/you can also sit in a reclining chair.
3. Loosen tight clothes; remove glasses, watch or jewelry.
4. Tense and relax specific group of muscles (palm, forearm, upper arm, shoulder, neck, eyes, forehead, scalp, eyebrow, chest, abdomen, buttock, thigh, lower leg, feet, sole muscles) as per the instruction. Start with relaxation technique.
5. First of all take a deep breath, hold it for 2 sec, then breathe out slowly. Again do it one more time.
6. Feel a wave of relaxation sweeping all over your body.
7. Again take a deep breath, hold it for 2 sec, then breathe out slowly.
Data collection procedure was as- subjects meeting the inclusion criteria were enrolled. Consent was obtained. Randomization was done. Demographic data, baseline fatigue and quality of sleep were assessed on the day of admission. The intervention PMR was carried out for experimental group subjects. Preoperatively, patients were provided with introductory booklet on PMR and were provided with demonstration of PMR by researcher for duration of 15-20 minutes on the same day in a calm, quiet, warm and comfortable room. All doubts of subjects were clarified. Ward staff were requested to cooperate in the intervention. On the third post-operative day, Subjects were provided with the audio-record of PMR (in CD/mobile phone) and activity log sheet. Subjects were verbally instructed and reinforced to practice PMR once a day, every day at the same time for 6 weeks and fill the activity log sheet after doing PMR. Subjects in experimental group were followed on their practice and telephonic reinforcements were given on weekly basis. Data regarding fatigue and sleep of quality were reassessed for both groups at 1 week of discharge (2 week after surgery) and 1 month (6 week after surgery). Activity log book were collected from the intervention group. Control group received the routine care. Researcher obtained the competency in PMR from a certified PMR instructor. Pilot study was conducted among 10 subjects and was found to be feasible. Confidentiality of information and anonymity of subjects was maintained. Ethical permission was obtained (Reference number-IECPG/217/24.02.2016).
Data analysis
Data were analyzed using SPSS version 20. Both descriptive (frequencies, percentages, mean, standard deviation, median and range) and inferential statistics (t test, chi-square test and Repeated measure ANOVA, oneway ANOVA, Wilcoxon rank sum test and Pearson correlation) were used.
The groups were comparable in terms of sociodemographic, clinical profile, baseline fatigue and quality of sleep (p>0.05) (Tables 1-3).
| Socio-demographic characteristics | Experimental Group (n=32) |
Control Group (n =33 ) |
p-value | |
|---|---|---|---|---|
| Mean +/- SD Frequency (%) | Mean+/- SD Frequency (%) | |||
| Age (in years) | 39.39±14.25 | 38.57±13.62 | 0.839 | |
| Sex | Male | 21(70.0) | 14(46.7) | 0.067 |
| Female | 9 (30.0) | 16(53.3) | ||
| Marital Status | Married | 22(73.3) | 22(73.3) | 1.000 |
| Unmarried | 8 (26.7) | 8(26.7) | ||
| Education | Primary | 11 (36.7) | 13(43.3) | 0.753 |
| Secondary | 15(50.0) | 14(46.7) | ||
| Graduate | 3 (10.0) | 3 (10.0) | ||
| Post graduate | 1 (3.3) | 0 | ||
| Occupation | Employed | 11(36.7) | 5(16.7) | 0.08 |
| Unemployed | 19(63.3) | 25(83.3) | ||
| Residence | Rural | 16(53.3) | 23(76.7) | 0.058 |
| Urban | 14(46.7) | 7 (23.3) | ||
| Religion | Hindu | 24(80.0) | 25(83.3) | 0.492 |
| Muslim | 6 (20.0) | 4(13.4) | ||
| Christian | 0 | 0 | ||
| Sikh | 0 | 1 (3.3) | ||
| Family type | Joint | 3 (10.0) | 2 (6.6) | 0.640 |
| Nuclear | 27(90.0) | 28(93.4) | ||
| Economic status | < 5000 | 0 | 4 (13.4) | 0.133 |
| 50,00-10,000 | 20(66.6) | 20(66.6) | ||
| 10,000-20,000 | 9(30.0) | 6 (20.0) | ||
| >20,000 | 1 (3.3) | 0 | ||
| *statistically significant, p<0.05, b chi square test | ||||
Table 1: Socio-demographic characteristics of patients in experimental and control group N=65.
| Clinical characteristics of patients | Experimental Group (n=30) |
Control Group (n=30) |
p-value | |
|---|---|---|---|---|
| Duration of illness(Year) c | Median (range) | Median (range) | 0.267 | |
| 3.5(1-15) | 3(1-7) | |||
| Frequency (%) | Frequency (%) | |||
| Diagnosis b | Mitral Valve Disease | 14(46.7) | 19(63.3) | 0.032* |
| Aortic Valve Disease | 10 (33.3) | 9(30.0) | ||
| Tricuspid Valve Disease | 0 | 2(6.7) | ||
| Multi valve disease | 6 (20.0) | 0 | ||
| NYHA b | 1 | 0 | 2 (6.7) | 0.343 |
| 2 | 15(50.0) | 15(50.0) | ||
| 3 | 15(50.0) | 13(43.3) | ||
| 4 | 0 | 0 | ||
| Surgery b | Mitral valve replacement | 14(46.7) | 19(63.4) | 0.066 |
| Aortic valve replacement | 10(33.3) | 9 (30.0) | ||
| Tricuspid valve replacement | 0 | 1 (3.3) | ||
| Double valve replacement | 6 (20.00) | 0 | ||
| valve repair | 0 | 1 (3.3) | ||
| Previous surgery b | Yes | 5 (16.6) | 2 (6.7) | 0.228 |
| No | 25(83.4) | 28(93.3) | ||
| Co morbidities b | Yes | 5 (16.6) | 1 (3.3) | 0.085 |
| No | 25 (83.4) | 29 (96.7) | ||
| *statistically significant, p<0.05, b chi square test; c Wilcoxon rank-sum test | ||||
Table 2: Comparison of clinical characteristics subjects in experimental and control group N=65.
| Groups | Pre test Fatigue score F1 | Pre test quality of sleep S1 |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Experimental group (n=30) | 25.80 ± 4.02 | 4.47 ± 1.83 |
| Control group (n=30) | 26.67 ± 4.76 | 4.70 ± 1.98 |
| P value | 0.450 | 0.638 |
Table 3: Comparison of pre test scores of fatigue and quality of sleep N=65.
Effect of PMR on fatigue
Table 4 and Figure 2 depict statistically significant (p-0.001) decrease in fatigue in both groups. There was no statistically significant decrease in fatigue level from preoperative period to two weeks after surgery in both the groups (p-0.125 and p-0.69). In experimental group, there was statistically significant decrease in fatigue from preoperative period to six weeks after surgery (p- 0.0001) as well as from 2 weeks after surgery to six week after surgery (p-0.0001) while in control group, there was no statistically significant decrease in fatigue level from preoperative period to six week after surgery (p-00.084) as well as from 2 weeks after surgery to six week after surgery (p-0.052). Table 5 depicts that groups were comparable in terms of baseline fatigue (p-0.450), although there was no significant difference between groups at two weeks after surgery (p-0.797). Statistically significant difference in fatigue is noted at six weeks (p-0.001) between the groups.
| Variable | Groups | Pre test | Post test 1 | Post test 2 | $Over all P value |
Pre test Vs post test1# |
Pre test Vs post test 2# |
Post test 1 Vs post test2# |
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ±SD | Mean± SD | P value | P value | P value | |||
| Fatigue scores | Experimental group(n=30) | 25.80 ± 4.02 |
24.43 ± 3.42 |
13.00 ± 2.42 |
0.0001* | 0.125 | 0.0001* | 0.0001* |
| Control group (n=30) | 26.67 ± 4.76 |
24.70 ± 4.50 |
22.73 ± 2.28 |
0.0001* | 0.069 | 00.084 | 0.052 | |
| #Paired t test, $ Repeated measure ANOVA *statistically significant p value < 0.05 Pre test-preoperative measurement Post test 1-measurement on 2weeks after surgery Post test 2-measurement on 6 weeks after surgery |
||||||||
Table 4: Comparison of pre test and post tests scores of fatigue within the groups N=60.
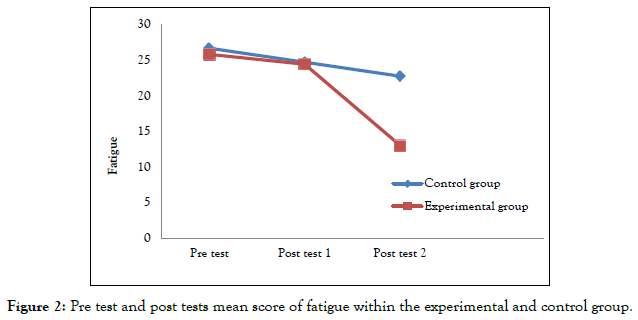
Figure 2. Pre test and post tests mean score of fatigue within the experimental and control group.
| Variable | Groups | Pre test F1 |
Post test 1 F2 |
Post test2 F3 |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Fatigue scores | Experimental group(n=30) | 25.80 ± 4.02 | 24.43 ± 3.42 | 13.00 ± 2.42 |
| Control group(n=30) | 26.67 ± 4.76 | 24.70 ± 4.50 | 22.73 ± 2.28 | |
| P value between the groups | 0.450 | 0.797 | 0.001* | |
| test :independent t-test *statistically significant p value < 0.05 Pre test-preoperative measurement Post test 1-measurement on 2weeks after surgery Post test 2-measurement on 6 weeks after surgery |
||||
Table 5: Comparison of pre test and post tests scores of fatigue between experimental and control group N=60.
Effect of PMR on quality of sleep
Table 6 and Figure 3 depicts that the sleep quality improved in experimental (p-0.0001) and control group (p-0.045). Experimental group had significant improvement in sleep quality from preoperative period to second week after surgery (p-0.0001) also from second week after surgery to six week after surgery (p-0.0001), although there was no significant improvement from preoperative to second week after surgery (p-0.056). While in control group, there was no significant improvement in sleep quality from preoperative period to two weeks after surgery (p-0.069), preoperative period to six week after surgery (p-0.734) and from two weeks after surgery to six weeks after surgery (p-0.057). Table 7 depicts that the groups were comparable in terms of quality of sleep at baseline (p-0.638). There was no statistically significant difference between groups at two weeks after surgery (p-0.822) although there was statistically significant between the groups at six weeks after surgery (p-0.0001).
| Variable | Groups | Pre test | Post test 1 | Post test 2 | Over all p value$ | Pre test Vs post test1# |
Pre test Vs post test 2# |
Post test 1 Vs post test2# |
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | P value | P value | P value | |||
| Quality of sleep scores | Experimental group(n=30) | 4.47 ± 1.83 | 5.57 ± 1.56 | 2.83 ± 1.08 | 0.0001* | 0.056 | 0.0001* | 0.0001* |
| Control group (n=30) | 4.70 ± 1.98 | 5.47 ± 1.85 | 4.57 ± 1.45 | 0.045* | 0.069 | 0.734 | 0.057 | |
| #Paired t test, $Repeated measure ANOVA *statistically significant p value < 0.05 Pre test-preoperative measurement Post test 1-measurement on 2weeks after surgery Post test 2-measurement on 6 weeks after surgery |
||||||||
Table 6: Within the group comparison of quality of sleep among experimental and control group N=60.
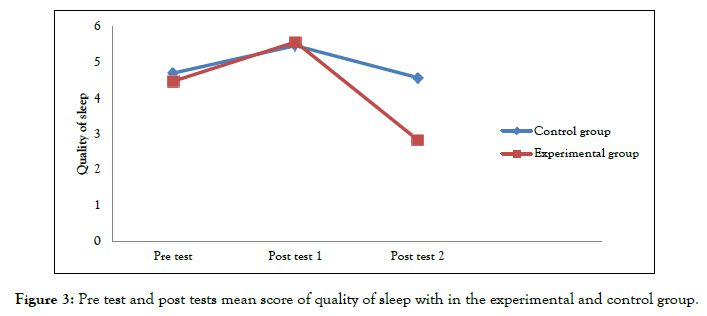
Figure 3. Pre test and post tests mean score of quality of sleep with in the experimental and control group.
| Variable | Groups | Pre test S1 |
Post test 1 S2 |
Post test 2 S3 |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Quality of sleep scores | Experimental group(n=30) | 4.47±1.83 | 5.57±1.56 | 2.83 ± 1.08 |
| Control group (n=30) | 4.70±1.98 | 5.47±1.85 | 4.57± 1.45 | |
| P value between the groups | 0.638 | 0.822 | 0.0001* | |
| test :independent t-test p*statistically significant value < 0.05 Pre test-preoperative measurement Post test 1-measurement on 2weeks after surgery Post test 2-measurement on 6 weeks after surgery |
||||
Table 7: Comparison of pre test and post tests scores of sleep quality between experimental and control group N=60.
Fatigue and sleep quality
Results of the present study revealed that there was a significant reduction of fatigue in experimental group as compared to control group; these findings are congruent with findings of Dehkordi et al. [29], DayapoÃÂ??lu et al. [30] and Akgün ÃÂ??ahin [31]. Findings of the present study depicted a statistically significant improvement in the quality of sleep after 6 weeks in the experimental group as compared to control group. Saeedi et al. [32] and Akgün ÃÂ??ahin [31] also had the similar findings. This is contradictory to the findings of Conway et al. [27], who found that there were no significant differences in sleep quality scores; the reason for such finding may be due to lesser duration of PMR therapy as compare to the present study. However, the qualitative analysis discovered that PMR aided some participants in initiating their sleep. In the present study there was no statistical difference between experimental and control group in terms of fatigue and quality of sleep at 2 week after surgery, as the compliance to PMR was very poor after 1 week of discharge (Table 8). Patients did not really practiced PMR in the immediate post operative period. These findings are congruent with Conway et al. [27] in which it is found that PMR is not effective in the early postoperative period. In the present study subjects were given an audio CD and instruction booklet to assist subjects in practice PMR at home, which is similar to the study by Yildirim and Fadiloglu [33].Similarly Singh et al. [34], Lolak et al. [35] and Cheung et al [36] also used audio tape in their studies. Audio record helps in maintain the consistency of the intervention over time and over the subjects. Carlson and Hoyle [37] found that giving progressive muscle relaxation on individual basis is significantly associated with positive effect.
| Week number | Patient compliant to PMR | Patient noncompliant to PMR |
|---|---|---|
| Frequency (%) | Frequency (%) | |
| 2nd week after surgery (1st week after discharge) | 2 (6.7) | 28 (93.3) |
| Over all compliance in week 3, 4, 5 and 6 | 29 (96.7) | 1 (3.3) |
Table 8: Frequency Distribution of Valve Surgery Patients Compliance to Progressive Muscle Relaxation (n=30).
The duration of treatment is important for the effect. In the present study, progressive muscle relaxation was practiced by patients once a day for 6 weeks, which is in line with the study by Heidarnia [25], Yildrim and Fadiloglu [33] also, administered it for 6 weeks but twice a day. Whereas Zaho et al. [38] administered it for 12 weeks. The routine follow-ups after cardiac surgery were conducted at 2 weeks and 6 weeks of surgery. So in the present study the follow-ups were intentionally kept at the same time. The present study provides support for the utility of relaxation therapy such as progressive muscle relaxation in reducing fatigue and improving quality of sleep. Dehdari et al. [39] and Kruahong et al. [26] also evaluated the effect of PMR among cardiac surgery patients and found that it is effective and these findings are congruent with the present study findings. PMR as a systematic technique used to achieve a deep state of physical and mental relaxation; it has been proven effective in reducing anxiety and depression in a variety of conditions including insomnia, asthma, coronary artery bypass surgery, and chemotherapy-induced nausea [37]. As this study examined PMR as a complementary nursing therapy, nurses can incorporate the relaxation therapy in to the holistic patient care.
Additional findings
Some of the subjective experience of the patients in the experimental group
Subject 05- “Ye exercise bohot achi cheez h..20 min me hi saarr sharer kasrat ho jaati h..bahut araam milta h…”
(This exercise is very good…in 20 mins exercise of whole body is done…I feel very relaxed after doing it…)
Subject 02-“Acha lagta h wyaaam krke…thodahalka ho jaata h sharer.”
(I feel good after doing the exercise…..the body feels little light)
Subject 07 - “Is exercise ko kr k thoda behtar mehsoos hota h.. tension nahi hota h...”
(I feel little better with this exercise…I feel relaxed as well I don’t have tension..)
“Abhi to araam hai…neend me sudhaar h or chinta me thodi kmi h..”
(it is relaxing…..there is improvement in my sleep and reduction in anxiety)
Subject 25- “mujhe pehle se achha mehsoos kr rhe hain……dheere dheere fayada kr rha h..
(I am feeling better than before..it is benefitting slowly)
Subject 15- “Abhi to neend acha aata h..ye wala exercise kaafi acha he….acha lagta he aapki CD sunke.”
(I have good sleep….this exercise is very good..feels good after listening your CD)
The strengths of the present study lies in its strong experimental design, individualized intervention, weekly reinforcement, teaching learning aids in form of CD, booklet, log sheet. The limitations identified were as single setting study, limited sample size, questionable reliability of compliance to PMR by participants, limited follow-up time, lack of blinding as well as all the procedures of data collection, intervention were done by the same person. Recommendations for the further study are as integration of PMR in pre-service and in-service nurse education program, regular assessment of pre-operative fatigue and sleep quality, use of evidenced based relaxation therapy. Similar studies can be replicated with large sample size, in a multi-centered setting, among different patient population.
As suggested by the findings of the present study, there is significant reduction in fatigue and improvement in quality of sleep among patients who practiced PMR. In order to provide quality care, healthcare professionals should incorporate evidencebased practices on utilising the most advantageous and safe complementary therapies. Nurses should integrate PMR in cardiac rehabilitation programs in order to reduce the psychological burden and dependence on pharmacological measures.
Citation: Archana JT, Ankita S, Gopichandran L, Devagourou V, Milind PH, Gauri SK (2021). Effect of Progressive Muscle Relaxation on Sleep Quality and Fatigue among Post Valvular Heart Surgery Patients. J Perioper Crit Intensive Care Nurs 7: 162. doi:10.35248/2471-9870.21.7.162
Received: 28-Dec-2020 Accepted: 18-Jan-2021 Published: 26-Jan-2021 , DOI: 10.35248/2471-9870.21.7.162
Copyright: © 2021 Archana JT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.