Journal of Ergonomics
Open Access
ISSN: 2165-7556
ISSN: 2165-7556
Research Article - (2019)Volume 9, Issue 1
Background: The incidence of Low Back Pain (LBP) in the United States is a common occurrence. One proposed cause is poor posture characterized by reduced lumbar lordosis while sitting. Proper retraining of seated posture could potentially increase lumbar lordosis and therefore reduce LBP. Various lumbar support devices, such as the BetterBack device, have been designed to decrease pain and improve posture, however, there is limited evidence to support these claims.
Methods: 18 subjects participated in a two-week study during which they wore the BetterBack device for 15 minutes per day for 14 days. Posture was analyzed using the PostureScreen® and SitScreen® mobile application. Participants rated pain with a Visual Analog Scale (VAS) each day before and after wearing the device.
Results: Average daily pain scores for all subjects after wearing the device were significantly less (p<0.05) than before wearing the device, with a mean decrease of 1.56 cm on the VAS. Pain scores were decreased on day 15 compared to initial scores, but these changes were not significant. Several postural measurements showed significant mean improvements, including the initial sitting thorax angle and forward head shift off of vertical in standing. The trunk thigh angle while sitting with the device on also improved.
Conclusion: The BetterBack device provided effective lumbar support immediately reducing LBP, but did not carryover without the device. Significant improvements were found in some of the postural measurements, however, the interpretation of the effectiveness of the device is limited by a small effect size.
Posture; Low back pain; Lumbar support; Back brace
It has been reported that over 80% of the population will experience Low Back Pain (LBP) at some point over the course of their lifetime [1,2]. Furthermore, LBP is the leading cause of disability in individuals less than 50 years of age in the United States [3]. Occupations that involve prolonged sitting, wholebody vibration and awkward posture increase the likelihood of developing LBP while a combination of these risk factors leads to the greatest incidence of LBP [4].
Makhouse et al. stated that poor posture characterized by reduced lumbar lordosis during prolonged sitting is one of the main causes of LBP [3]. Prolonged seated positions are associated with increased lumbar flexion and greater loads on the ischial tuberosities, causing an increase in the amount of pressure through the lumbar spine [3]. The promotion of normal lumbar lordosis is thought to improve posture and therefore decrease LBP. Maintaining the lordotic curve of the lumbar spine in sitting decreases ligamentous stress, intradiscal pressure, and decreases disc degeneration of the spine [5]. Proper retraining of seated posture is thought to carry over to proper standing posture, decreasing pain and discomfort in the lower back [5].
Szczygiel et al. stated that slumped posture diminishes the natural curvature of the spine and places excessive pressure on the intervertebral discs [6]. According to De Carvalho, the natural physiological position of the spine reduces pain and the risk of overloading, while increased lumbar kyphosis predisposes the individual to LBP [7]. Szczygiel et al [6]. and De Carvalho [8] agree that incorrect sitting posture contributes to many disorders, especially in the cervical and lumbar spine. Additionally, maintaining the physiological curvature of the spine is crucial to the biomechanics of the sitting position, particularly head posture and the position of the pelvis [6].
Previous studies have investigated the use of posture correction devices similar to the BetterBack device, such as the NADA chair. The NADA chair device, as opposed to a conventional chair alone, has been shown to produce greater lumbar lordosis while in a seated position [9]. However, there is limited research on the direct effect of the NADA chair on LBP. The BetterBack device is proposed to retrain proper posture by increasing both anterior rotation of the pelvis and lumbar lordosis. The makers of the BetterBack device claim that wearing the device for 15 minutes a day can retrain the body’s default posture so that when sitting or standing without the device, posture is greatly improved, thereby easing back pain or preventing it. The device is adjustable, allowing it to accommodate to the lordosis of each individual. The device also comes with a center clip to keep the legs together for increased muscle relaxation.
The purpose of this study is to determine the effectiveness of the BetterBack device on improving posture and decreasing LBP during and after wearing the device. Research that investigates the effect of lumbar support devices is limited, despite the high incidence of LBP and poor posture.
The Institutional Review Board (IRB) at William Carey University approved this study (IRB # 2018-110). Subjects for the study were recruited for convenience from the faculty and staff of William Carey University, the University of Southern Mississippi, local church congregations, and through Facebook posts from the William Carey University Physical Therapy Program. Initial recruitment methods included email, Facebook posts, and handdelivered flyers with a description of the study. Participants were included in the study if they 1) Were between 20 and 55 years of age, 2) Were experiencing a current episode of LBP of fewer than six months duration, 3) Experienced pain considered to be moderate to severe in intensity, and 4) Reported pain when sitting. The average onset of LBP occurs between the ages of 20 and 40 [10]. The maximum age of 55 was chosen to decrease the likelihood of subjects having lumbar spinal stenosis, which is a condition that is exacerbated by lumbar extension that is most often diagnosed in individuals over the age of 65 [11]. It has been found that pain of greater than six months in duration is associated with increased use of pain medication [2].
Participants were excluded from the study if they: 1) Were currently receiving medical care for LBP, 2) Currently using prescription pain medications, 3) Had a diagnosis of osteoporosis, neurogenic claudication, or peripheral vascular disease, 4) Had a previous back surgery, 5) Had a report of current pain of greater than six months in duration, 6) Were unable to tolerate mild to moderate pressure on the anterior aspect of the knees, or 7) Reported pain that was considered to be mild, or three or less on a VAS.
There were 21 subjects that met the inclusion criteria and participated in the study. A time and date was set up for pretest assessments of the subjects. All subjects signed an informed consent form prior to participating in the study. The pre-test assessment included completing a demographic sheet (Table 1) and a pain assessment using a ten-centimeter Visual Analog Scale (VAS), in which the subject would place a mark on the line indicating severity of pain from left to right. Prior to taking four different photos using the PostureScreen® and SitScreen® mobile application, posture markers were applied to the participant’s right external auditory meatus, lateral shoulder in line with the acromioclavicular joint, greater trochanter, middle of the lateral knee joint, and lateral malleolus. The examiners followed the instructions from the applications to apply location points on the photos so that the individual posture angles could be generated, but used the previously applied posture markers as reference points to ensure accuracy (Figure 1). The initial assessments were divided among two examiners who took all of the pre-test photos. For each subject, examiners first took a photo of forward and lateral standing and initial sitting postures. A photo was taken after 20 minutes of sitting in the subject’s position of comfort, and the final photo was taken while wearing the BetterBack device in a seated position. All seated and standing lateral photos were taken from the subject’s right side. All subjects sat in identical standard height chairs for pre and post-assessment. The angles and linear distances of posture measured and analyzed in the study were: standing forward head shift off-vertical angle, sitting neck posture angle, sitting thorax angle, and sitting trunk thigh angle.
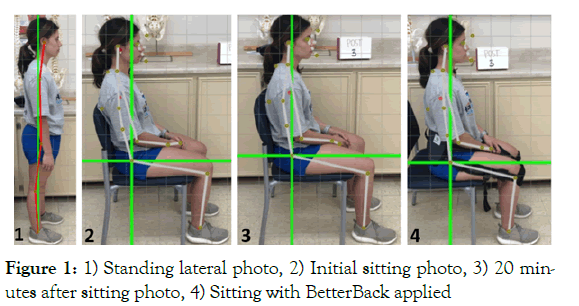
Figure 1: 1) Standing lateral photo, 2) Initial sitting photo, 3) 20 minutes after sitting photo, 4) Sitting with BetterBack applied
Table 1: Participant demographics
| Number of participants | 18 |
| Gender (Male:Female) | 05:13 |
| Age range (Years) | 22-54 |
| Mean age (Years) | 29 |
| Height range (inches) | 55-75 |
| Mean height (inches) | 66 |
The examiners instructed the subjects in the correct application and removal of the BetterBack device and informed the subjects to adjust the device as needed for comfort. Subjects were instructed to adjust the device as needed for comfort. Subjects were told to return to their normal daily routines and to record the use of the BetterBack device for 15 minutes per day over 14 consecutive days in their daily journals supplied by the examiners. Subjects were instructed to record their daily pain levels using a VAS of zero to ten, and a space for optional comments was also provided in the journal. The examiners assisted subjects with the setup of a daily digital reminder to wear the BetterBack device. Participants were scheduled for a follow-up post-test assessment two weeks after the pre-test assessment.
Twenty subjects returned after 14 days for the post-test assessment. The post-test assessment included a post-test survey to assess postural and proprioceptive awareness and the VAS. Daily journals were retrieved from all subjects, and each subject rated their current pain according to the VAS. Photos were taken again as per pre-test methodology. The same two examiners took post-test photos of the same subjects they photographed in pre-testing. The results of the pre-tests and post-tests were compared for each subject.
Three subjects were excluded from the final data analysis. Two subjects discontinued the use of the Betterback device due to increased pain, with one subject reporting an increase in radicular pain while wearing the device and the other subject reporting anterior knee pain while wearing the device. Lastly, a third subject completed the study but had to be excluded due to undergoing unrelated foot surgery and having to take prescription pain medication throughout the second week of the study. Overall, 18 subjects were included in the data analysis of the pain scores ascertained from the VAS in the daily journals and the posture angles generated from the PostureScreen® and SitScreen® mobile applications. The subjects’ demographics are listed in Table 1.
Pain scores from the VAS, reported in Figure 2, were analyzed (Table 2) each day using paired t-tests. Among all subjects, on average, pain scores for each one of the 14 days after wearing the device were significantly less (p<0.05) than the pain prior to wearing the device, with a mean decrease of 1.56 cm on the VAS. This suggests that wearing the brace for 15 minutes has an immediate effect in reducing the pain. The pain on day 15 was decreased, but was not significantly less than it was on the first day of the study prior to wearing the device. The effect size strength for the pain ratings was medium on days one and two, large on days three through 14, and small for day 15.
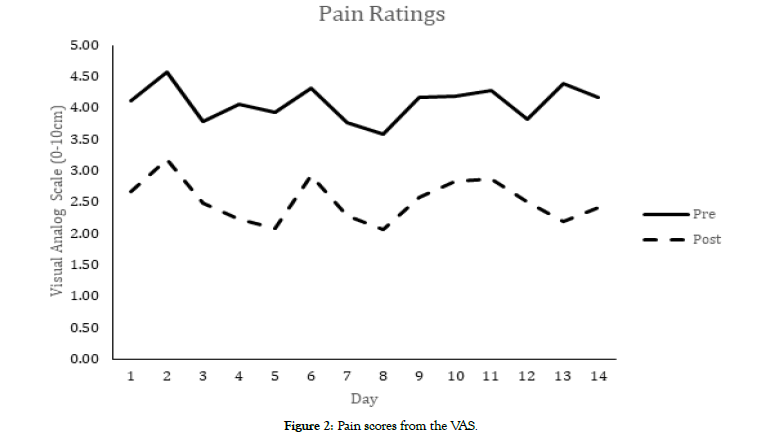
Figure 2: Pain scores from the VAS.
Table 2: Pain analysis.
| VAS report by day | Mean | N | SD | SEM | df | p-value | Effect Size |
|---|---|---|---|---|---|---|---|
| pre1 | 4.11 | 18 | 2.06 | 0.49 | 17 | 0.003 | 0.73 |
| post1 | 2.68 | 18 | 2.07 | 0.49 | |||
| pre2 | 4.58 | 18 | 2.45 | 0.58 | 17 | 0.004 | 0.71 |
| post2 | 3.19 | 18 | 2.52 | 0.59 | |||
| pre3 | 3.78 | 16 | 2.63 | 0.66 | 15 | 0.002 | 0.85 |
| post3 | 2.49 | 16 | 2.16 | 0.54 | |||
| pre4 | 4.06 | 17 | 2.61 | 0.63 | 16 | 0 | 1.05 |
| post4 | 2.22 | 17 | 2.04 | 0.5 | |||
| pre5 | 3.94 | 13 | 2.56 | 0.71 | 12 | 0.001 | 1.19 |
| post5 | 2.09 | 13 | 2.07 | 0.57 | |||
| pre6 | 4.31 | 17 | 2.96 | 0.72 | 16 | 0 | 1.1 |
| post6 | 2.93 | 17 | 3.01 | 0.73 | |||
| pre7 | 3.76 | 16 | 2.69 | 0.67 | 15 | 0.003 | 0.8 |
| post7 | 2.29 | 16 | 2.04 | 0.51 | |||
| pre8 | 3.58 | 15 | 2.1 | 0.54 | 14 | 0.001 | 0.93 |
| post8 | 2.07 | 15 | 1.75 | 0.45 | |||
| pre9 | 4.18 | 17 | 2.65 | 0.64 | 16 | 0.003 | 0.77 |
| post9 | 2.58 | 17 | 2.35 | 0.57 | |||
| pre10 | 4.19 | 18 | 2.92 | 0.69 | 17 | 0.001 | 0.9 |
| post10 | 2.84 | 18 | 2.25 | 0.53 | |||
| pre11 | 4.28 | 18 | 2.57 | 0.61 | 17 | 0.001 | 0.87 |
| post11 | 2.87 | 18 | 1.91 | 0.45 | |||
| pre12 | 3.82 | 14 | 2.23 | 0.6 | 13 | 0.003 | 0.87 |
| post12 | 2.51 | 14 | 2.42 | 0.65 | |||
| pre13 | 4.38 | 16 | 2.52 | 0.63 | 15 | 0 | 1.22 |
| post13 | 2.19 | 16 | 1.93 | 0.48 | |||
| pre14 | 4.17 | 18 | 2.56 | 0.6 | 17 | 0 | 1.22 |
| post14 | 2.41 | 18 | 2.36 | 0.56 | |||
| pre1 | 4.11 | 18 | 2.06 | 0.49 | 17 | 0.093 | 0.32 |
| post15 | 3.38 | 18 | 2 | 0.47 |
Deg: Degrees; N: Number of subjects; SD: Standard Deviation; SEM: Standard Error Mean; df: Degrees of Freedom
Posture screen results were analyzed using paired t-tests. Several positions that were assessed did not reveal significant changes when pre-test and post-test data were evaluated, including the neck angle and trunk thigh angle in initial sitting. The neck posture and thorax angles did not show significant changes after sitting for 20 minutes or sitting with the device. The trunk thigh angle did not show significant changes after sitting for 20 minutes. Significant changes were found in multiple positions, including the thorax angle in the initial sitting position, forward head shift off vertical in the standing position, and the trunk thigh angle while sitting with the device.
The neck angle is defined as the angle created by a line from the base of the neck at the cervicothoracic junction to the external acoustic meatus in relation to vertical. The thorax angle’s axis is located at the approximate level of T6-T8 in the mid torso with the proximal point of reference at the base of the neck at the cervicothoracic junction, and the distal point of reference at the approximate level of T10-L1 in the mid torso. The trunk thigh angle is defined as the angle created by a line from the greater trochanter to the approximate level of T10-L1 in the mid torso in relation to vertical.
The analysis of posture angles is listed in Table 3. The neck posture angle showed a mean improvement of 1.7 degrees across all subjects. The thorax angle showed a mean improvement of 6.14 degrees. Forward head shift off vertical showed a mean improvement of 2.89 degrees. The trunk thigh angle while sitting while wearing the device showed an increase of 4.76 degrees. The effect size strength for the postural measurements was medium for the forward head shift off vertical, neck posture, and thorax angles. The effect size strength was small or negligible for all other posture measurements.
Table 3: Posture analysis.
| Test | Posture Measurements (deg) | Mean | N | SD | SEM | df | p-value | Effect Size |
|---|---|---|---|---|---|---|---|---|
| pre | Standing Lateral View: Off Vertical | 11.42 | 18 | 5.33 | 1.26 | 17 | 0.01 | 0.598 |
| post | Standing Lateral View: Off Vertical | 8.53 | 5.03 | 1.19 | ||||
| pre | Sitting Initial: Neck Posture | 6.45 | 18 | 4.77 | 1.13 | 17 | 0.06 | 0.376 |
| post | Sitting Initial: Neck Posture | 4.75 | 4 | 0.94 | ||||
| pre | Sitting Initial: Thorax | 159.87 | 18 | 8.01 | 1.89 | 17 | 0 | 0.795 |
| post | Sitting Initial: Thorax | 166.01 | 5.68 | 1.34 | ||||
| pre | Sitting Initial: Trunk Thigh | 11.16 | 18 | 4.79 | 1.13 | 17 | 0.38 | 0.0728 |
| post | Sitting Initial: Trunk Thigh | 11.5 | 4.4 | 1.04 | ||||
| pre | Sitting after 20': Neck Posture | 4.54 | 18 | 4.69 | 1.1 | 17 | 0.29 | 0.523 |
| post | Sitting after 20': Neck Posture | 3.97 | 3.04 | 0.72 | ||||
| pre | Sitting after 20': Thorax | 164.24 | 18 | 6.85 | 1.61 | 17 | 0.46 | 0.0228 |
| post | Sitting after 20': Thorax | 164.45 | 5.73 | 1.35 | ||||
| pre | Sitting after 20': Trunk Thigh | 12.76 | 18 | 4.43 | 1.04 | 17 | 0.39 | 0.0744 |
| post | Sitting after 20': Trunk Thigh | 12.27 | 5.57 | 1.31 | ||||
| pre | Sitting with Device: Neck Posture | 6.26 | 18 | 5.99 | 1.41 | 17 | 0.5 | 0.001 |
| post | Sitting with Device: Neck Posture | 6.25 | 5.15 | 1.21 | ||||
| pre | Sitting with Device: Thorax | 164.94 | 18 | 7.66 | 1.81 | 17 | 0.1 | 0.321 |
| post | Sitting with Device: Thorax | 168.02 | 6.62 | 1.56 | ||||
| pre | Sitting with Device: Trunk Thigh | 6.23 | 18 | 3.47 | 0.82 | 17 | 0.03 | 0.458 |
| post | Sitting with Device: Trunk Thigh | 11 | 9.62 | 2.27 |
Deg: Degrees; N: Number of subjects; SD: Standard Deviation; SEM: Standard Error Mean; df: Degrees of Freedom
The post-test questionnaire results (Table 4) were as follows for the 18 subjects included in the final analysis. The post-test questionnaire results indicate that the use of the BetterBack device improved awareness of posture while sitting and standing (94% of subjects), improved their ability to find a position of relief and maintain it (72% of subjects), and improved their posture (78% of subjects).
Table 4: The post-test questionnaire results
| Post-Test Questionnaire | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| Since using the BetterBack, I am now more aware of my posture while sitting and standing. | 5 (27.78%) | 12 (66.67%) | 1 (5.56%) | 0 | 0 |
| Since using the BetterBack, when I am having back pain, I am able to find a position of relief and maintain it. | 3 (16.67%) | 10 (55.56%) | 5 (27.78%) | 0 | 0 |
| I feel that BetterBack has improved my posture. | 3 (16.67%) | 11 (61.11%) | 3 (16.67%) | 1 (5.56%) | 0 |
A significant decrease in pain occurred immediately after wearing the device, however, a carryover of pain reduction from one day to the next was not noted. The large effect size noted for the pain ratings indicates that wearing the BetterBack device for immediate pain relief is a reasonable option for individuals with LBP while sitting. The authors speculate that these positive effects could be due to having less demand on the spinal musculature while wearing the device compared to sitting without the device. The potential increase in muscle activation demand or the worsening of posture without the device seemed to be related to increased pain. In addition, several subjects also reported that using the clip between the two inner leg straps made the device more comfortable. This could indicate that using the clip further decreased the amount of muscle activation required to maintain a comfortable sitting posture. Further research is required to evaluate the effectiveness of the BetterBack device for individuals with LBP from conditions that were outside of the inclusion criteria of this study.
Several angles related to posture were improved significantly. Forward head shift off vertical in the standing position showed a significant improvement. This could indicate that there is some carry over from sitting postures into standing postures after wearing the device while sitting for only 15 minutes a day, as the makers of the BetterBack device claim. Both the neck and thoracic angles were improved in the initial sitting photo, but these improvements were not maintained after 20 minutes of sitting. This could indicate that users may need to wear the device longer than two weeks to see improved posture with prolonged sitting. Wearing the device for a longer period of time, rather than the recommended 15 minutes, could potentially improve additional sitting and standing posture angles. The trunk thigh angle while sitting with the device showed a significant increase of 4.76 degrees. Although this angle became less vertical, the authors do not necessarily feel that this was a negative result. It has been found that sitting in a more active, erect position requires more muscle activity than sitting in other, more relaxed positions [12,13]. Therefore this increased trunk thigh angle most likely reflects a more relaxed sitting position after becoming accustomed to the device and using it for longer periods of time.
The authors have identified potential limitations to this study. The small effect size introduces the potential for error in the interpretation of the posture results that were found to be significant. A larger sample size would be required to improve the effect size strength of the posture results. Another limitation of this study is the possibility of an expectation effect in the results of the self-reported pain level. Since the purpose of the device was explained to the subject, the respondents may have experienced a decrease in pain due to a placebo effect.
Recommendations for future research include increasing the duration of the study beyond two weeks or increasing the amount of time the device is worn each day. By increasing these variables, future researchers could investigate whether more long term pain relief is achieved, or if any other postural changes are improved. The authors suggest repeating the study with broader inclusion criteria, including subjects with chronic pain and of ages greater than 55.The inclusion criteria in this study was potentially too narrow to capture the full spectrum of the population who may benefit from the BetterBack device.
In conclusion, the authors’ opinion is that the BetterBack device can most effectively be used for immediate reduction of lower back pain that is not exacerbated with lumbar extension. Despite the lack of significant postural findings, the authors observed increased lumbar lordosis in subjects while wearing the device. Two of the authors have extensive experience in observational analysis of posture, and two others have training with limited experience. All four were in agreement that the BetterBack device increased lumbar lordosis while it was being worn. The authors feel that potentially a wider range of people than was allowed by the inclusion criteria of this study could benefit from using the BetterBack device, but further research is warranted to make a definitive recommendation. Subjects using the BetterBack device felt as though their posture and awareness of posture improved with the use of the device. Subjects also reported an improvement in their ability to find a position of relief and maintain it as a result of using of the BetterBack device. This indicates that people with postural abnormalities and position dependent pain may experience improved awareness of posture and an increased ability to find positions that minimize their pain.
Citation: Parker AD, Burns JR, Boyd JC, Reynolds LM, Atkins KT, Pollitte WA (2019) Does BetterBack Lumbar Support and Posture Trainer Decrease Back Pain and Improve Posture? J Ergonomics 9:250.
Received: 12-Jun-2019 Accepted: 02-Jul-2019 Published: 10-Jul-2019 , DOI: 10.35248/2165-7556.19.9.250
Copyright: © 2019 Parker AD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.