Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Research Article - (2016) Volume 6, Issue 1
In order to increase the medical competence in the ambulance service the National Board of Health and Welfare in Sweden stated in the year 2000 that every ambulance should be manned by at least one Registered Nurse (RN), and the rule entered into force in 2005. Now, nearly ten years have passed, and a question arises: how has the ambulance service and pre-hospital care developed since RNs became part of the ambulance service? Therefore the aim of this study was to explore how the ambulance services have developed since RNs became a part of the pre-hospital emergency care provided by the ambulance service. An explorative descriptive design was used. Data collection was carried out by a focus group interview and through a review of medical guidelines written by the medical directors and
used in the years 1999, 2006 and 2015. A content analysis was conducted based on the collected data. The results shows how the pre-hospital emergency care has developed since RNs started to work in the ambulance service. The main areas of development concerned assessment of patients’ illness and injury, medical treatment, and steering to an optimal level of care, together creating conditions for care based on the individual patient needs. These findings may indicate an increasing independence in decision making among pre-hospital personnel after the RNs become a part of the ambulance service.
Keywords: Registered nurses; Pre-hospital emergency care; Ambulance service; Development; Patient centered care; Content analysis
The ambulance services have over the years developed from a transport organization to an important part of the chain of care for seriously ill or severely injured patients. Historically, the emergency medical technicians (EMTs) and fire fighters have manned the ambulance service in Sweden [1]. In order to increase the medical competence, the National Board of Health and Welfare in Sweden stated in the year 2000 that every ambulance should be manned by at least one Registered Nurse (RN) and the statement entered into force in 2005 [2,3]. In accordance with the regulation, only RNs were permitted to administer medicines, and without at least one RN in the ambulance no medicines could be administered. At present, other countries such as Finland, Belgium and the Netherlands also use RNs in the ambulance service, and England and Wales use RNs to some extent [4]. More common in the chain of pre-hospital emergency care are paramedicbased ambulance service [5] in addition to physician-manned helicopters [6]. It is known that higher qualifications, more training, and experience in pre-hospital emergency care increase survival after out-of-hospital cardiac arrest and for patients suffering from medical conditions such as respiratory illness [7]. But there are no identified studies describing the effect of Registered Nurses (RN) on increased survival in the ambulance service. A study concluded that having RNs in the ambulance service may result in better assessment of patient needs, but the study showed no impact on performed interventions in the ambulance service or on hospital mortality compared to care and assessment performed by EMTs [8]. However, there is little literature describing the role of RNs in the ambulance service [4,9]. Therefore, the aim of this study was to explore how the ambulance services have developed since Registered Nurses became a part of the pre-hospital emergency care in the ambulance service in Stockholm, Sweden.
After the regulation entered into force in 2005 [10] the crew of an ambulance consisted of one RN and one EMT. The RNs have Advance Life Support (ALS) competences and the EMTs have Basic Life Support (BLS) competence, and both are re-certified every year. The ambulance service is provided either by the County Council or by private companies contracted by the County Council. There are approximately 700 ambulances operating in Sweden, and in Stockholm, the capital, there are 71 ambulances and one physician-manned ambulance operating during daytime. In Stockholm with 2.2 million inhabitants, the ambulance service conducts approximately 187 000 ambulance assignments yearly [1]. Before the regulation on having RNs in the ambulances the EMTs were allowed to administer medicines such as salbutamol in case of respiratory distress, nitric oxide/ oxygen when patients suffered from pain, and intravenous adrenalin for patients with cardiac arrest. When it became mandatory to have RNs it led to several of the EMTs being dismissed, and the EMTs who continued to work in the ambulance services no longer had permission to administer any medications except for oxygen. The EMTs were not allowed to give any medications but they needed to introduce the RNs in to the work since most of the RNs did not have any experience (or training) in working in the ambulance service while the EMTs had the contextual knowledge. At present in Sweden the trend is towards a requirement for the presence of a specialist nurse, an RN with one year of additional training in emergency care (Pre-hospital Emergency Care Nurse) in every ambulance. The additional training is conducted at the university and the RN completes a master thesis as part of this education [11].
To explore how the ambulance service have developed since RNs became a part of the pre-hospital emergency care in the ambulance service an explorative descriptive design was used. Data collection was carried out by a focus group interview and through a review of medical guidelines used in the years 1999, 2006 and 2015 in the ambulance service. The medical guidelines were written by the medical directors in the ambulance service. A content analysis inspired by Hsieh and Shannon was conducted on the collected data [12]. The purpose of this design was to develop an understanding of how the ambulance services have developed since RNs became a part of the pre-hospital emergency care in 2005.
Focus group interview
Purposeful samples of retired EMTs were invited to participate in a focus group interview. A purposeful sampling aims to find “information- rich cases”, those who know and can express a lot about the issue being studied [13]. In this study, that meant persons with knowledge of the history and development of the ambulance service. Focus group interviews have advantages when gathering information on what people say when exploring experiences and practices [14]. Three male EMTs aged 65-70 years who started to work in the ambulance service during the 70s and retired in 2013 participated. The EMTs have served in urban, sub-urban and rural areas in the County of Stockholm, Sweden. The interview started with an overall conversation that occurred naturally and was not audio-recorded. When recording started, the participants received instructions and information about the aim of the study. The discussions during the interview were encouraged by open-ended questions such as: Can you describe how the work in the ambulance has changed over the years? The open-ended questions aimed to inspire the participants to speak and discuss freely. Probing questions such as: Can you describe? Can you explain? And can you give an example? Were used to clarify the communication in the group [13]. The interview lasted 100 minutes. The interview was transcribed verbatim.
Review of medical guidelines
Convenience samples of three editions of medical guidelines were included in the review. The included guidelines were from the years 1999, 2006 and 2015. The medical guidelines from 2015 are available on-line [15]; the others are paperback books that were available.
The data analysis of the interview was conducted inspired by qualitative content analysis described by Hsieh and Shannon [12]. The first part of the analysis consisted of listening and transcribing the interview. In the transcription of the interview, all three participants were identified to be participating in the discussions, and no single participant was identified as dominant compared to the other participants. The second part of the analysis consisted of reading all the transcribed material several times to obtain a sense of the whole. The next step, employing a deductive approach, consisted of identifying the descriptions of how the ambulance service had developed since the RNs became a part of the pre-hospital emergency care in the ambulance service. Meaning-units illuminating the purpose were then collected in an electronic spreadsheet. Next, coding of the descriptions was carried out. According to Hsieh and Shannon, the coding is a summary of and a reflection on the description [12]. After coding of the descriptions an electronic spreadsheet with all the codes was created and then further categorized into sub-categories. The sub-categories with similar content were then grouped together into a main-category (Table 1).
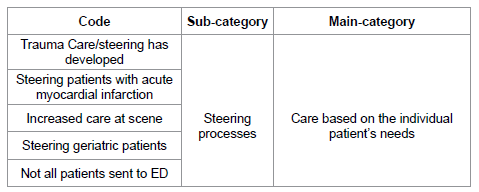
Table 1: Illustration of the process from coding to creation of sub-109 categories and a main-category.
All authors read the transcripts and evaluated the codes and subcategories several times in order to be true to the EMTs descriptions. In congruence with the exploratory aim of this study the sub-and maincategories represent general, rather than specific, descriptions of the EMTs experiences of RNs in the ambulance service. The analysis of the medical guidelines started with reading the text to obtain a sense of the whole. The next step consisted of searching for differences and similarities, aiming to identify the development of the care during the years 1999, 2006 and 2015. Quantitative variables and meaning-units describing differences and similarities in the guidelines were then collected into an electronic spreadsheet. Then coding of the descriptions was carried out in the same way as the group discussion analysis.
Finally, the findings from focus group interview and the guidelines were merged into one presentation of findings. The merging of findings was done in order to create a picture of how the ambulance service had developed since RNs became a part of the pre-hospital emergency care. This presentation of findings makes it possible to compare the qualitative results from the focus group interview with the quantitative data from the medical guidelines. This merging of data was inspired by Sandelowski et.al who describes the value of converting qualitative data into a quantitative form [16].
Ethical considerations
The study was designed to meet the ethical principles for research described by the International Council of Nurses, ensuring the anonymity, integrity and confidentiality of the participants. Before starting the focus group interview it was emphasized that participation was voluntary and the participants could withdraw from the study at any point without consequences. All participants signed a consent form before participating in the study.
From the focus group interview one main category was identified, describing how the ambulance services have developed after RNs became an element of the care: Care based on the individual patient needs (Table 2).
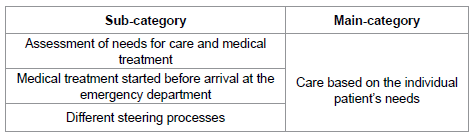
Table 2: Identified sub-and main categories.
The main category shows how the pre-hospital emergency care has developed since RNs started to work in the ambulance services. According to the interview the main areas of development concerned assessment, medical treatment, and steering to an optimal level of care, together creating conditions for care based on the individual patient needs. This is to some extent congruent with the content in the medical guidelines; an increase of medicines available in the ambulances, and an increase in medical conditions described (Table 3). Despite the increase of medical treatments and the RNs becoming an element of the prehospital emergency care, the nursing aspects almost disappeared in the 2006 and 2015 editions of the medical guidelines.
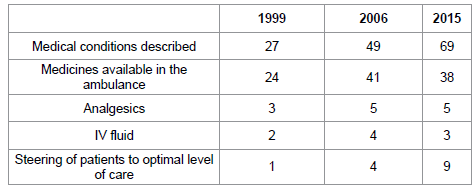
Table 3: Quantitative descriptions of the Medical Guidelines.
Assessment, medical treatment and goals of treatment are described in all editions of the medical guidelines, but there are differences. In the editions of 2006 and 2015 there are more descriptions of how to assess patients’ medical condition and there are flow charts illustrating treatment strategies, and different assessment tools such as the Glasgow Coma Score and Apgar Score are also described. The goals of treatment are described as expected measurements of patients’ vital sign i.e. saturation >95, blood pressure >90 mmHg. In the 1999 edition the descriptions of assessment is questions to be answered and the treatment is described as; start with one intervention - evaluate- if necessary do next intervention. The goals of treatment in 1999 edition are described as “do the best possible” and take care of the patient by using the the accelerator pedal in the ambulance.
According to the findings in the interview, the medical treatment and symptom relief started earlier with the RN in the ambulances and the patients were in better condition when delivered to next level of care, the emergency department (ED). For example, patients suffering a suspected hip fracture received greater pain relief before being moved to a stretcher at the scene and the patients received intravenous fluid before arrival at the ED after the RNs began to work in the ambulance service. However, the increase of care and treatment led to care staff spending a longer time at the scene according to the interview: “A longer time at scene is good for the patient, but not for the preparedness of the ambulance service”.
The steering processes have developed since the RNs started to work in the ambulance service. The steering processes of patients to an optimal level of care were described both by the EMTs and were found in all medical guidelines. But there has been a development over the years, from one steering process described in the 1999 edition to nine in the 2015 edition of the medical guidelines. Steering patients to the optimal level of care in the 2015 edition includes for example steering patients directly to geriatric awards, by-passing the ED by transporting patients to X-ray departments or different interventions such as the Percutan Coronary Intervention. According to the interview, the chain of trauma care has also developed through the distinguishing of different traumas and transporting the patients to the optimal hospital 174 instead of the nearest hospital where trauma surgeons were not always available. This finding on trauma steering from the interview is to some extent congruent with what the guidelines describe. Trauma steering is described in all medical guidelines, but there are differences concerning details in the trauma steering. For example, according to the guidelines (2006, 2015), severe injury trauma patients with injuries such as two or more femur diaphyseal fractures should be transported to a trauma level one hospital instead of the nearest emergency hospital (1999).
Although the EMTs described development of the ambulance service since RNs started to work, the EMTs also communicated a feeling of disappointment caused by the non-fulfilment of their expectations. Their expectations concerned the RNs independence “they still need to call the physician in the same way as we did… I thought they would be more independent when taking decisions on the patients’ care”.
Medical guidelines
The review of the medical guidelines showed additional changes that have taken place since the RNs became a part of the organization. A major change concerns out-of-hospital- cardiac-arrest: not initiating Cardio Pulmonary Resuscitation (CPR) and ending CPR without a physician at the scene. In the 2006 and 2015 editions there are clear descriptions of how and when the RNs may and may not start and end CPR without previous contact with a physician. In the 1999 edition the description is “Unsuccessful CPR may be interrupted after contact with a physician”. Another change in the medical guidelines over the years is the additional information on administrative routines and the ambulance personnel’s responsibilities as regards the care of the patient. The number of pages in the medical guidelines has increased from 110 in the 1999 edition to 257 pages in the 2015 edition, mainly because of the increase of descriptions of different medical conditions and administrative procedures. However, in the 1999 edition there were instructions not found in the 2006 and 2015 editions, about on-going studies, handling of air bags and nursing interventions.
There has been a development of the pre-hospital emergency care in the ambulance service since the RNs became a part of the organization. This finding is congruent with Williams’ discussion on how RNs complement the paramedics when improving the care delivered in the ambulance service in England and Suserud’s description about a new profession in the pre-hospital care [4,10]. However, it is not known if and how this development would have occurred without the RNs. But according to the national regulations in Sweden, there was no possibility of continuing to staff the ambulances with only EMTs after 2005. A study by Aiken et al. shows that higher academic education among RNs may reduce the mortality at hospitals [17]. An assumption could be that having RNs with a bachelor’s or master’s degree working in the ambulance service may improve care delivered in the ambulance service. But a study by Falk et al. showed no significant results in pre-hospital interventions or mortality in patients suffering from severe traumatic brain injury [8]. Nevertheless, the findings in this study show that the medical treatment and care based on the individual patient’s needs have developed over the years, and this may support an assumption that better care has been delivered in the ambulance service since RNs became a part of the organization. But still we do not know to what extent the RNs have an impact on the patient care, and further research is needed to explore how and if the RNs competence have an effect on patient outcomes in the ambulance service. The EMTs expressed a feeling of disappointment when the RNs started to work in the organization. This was caused by the non-fulfilment of their expectations concerning RNs independence. One explanation for this could be that regardless of whether there are EMTs or RNs working in the organization, it is still the medical advisor, the ambulance physician, who decides on the guidelines used in the ambulance service.
The findings showed that the nursing content decreased in the 2006 and 2015 editions of the medical guidelines. This is to some extent a paradox since the RNs main profession is nursing. The small amount of nursing content in the medical guidelines is congruent with the findings that were found in a study for curriculum to become a nurse pre-hospital emergency care in Sweden. The curriculum contained more medical than nursing skills/science [11]. The lack of nursing content in the guidelines may reflect the need of knowledge in medicine science since the physicians are not a part of the daily activities in the ambulance service in Sweden. Personnel working in the ambulance service need medical knowledge supported by guidelines. But the medical knowledge is not sufficient alone; there is a need for knowledge about nursing and caring relations in the ambulance service [18]. There is also a need of expressing the nursing aspects on care in the ambulance service. However, the nursing content decreasing in the 2006 and 2015 editions of the medical guidelines could also be explained by RNs have a higher baseline education than the EMTs and the content of guidelines could have changed to reflect this. There is not a need of simplistic description of different interventions. The expanding of medical guidelines may be evidence of increased standards of care after RNs become a part in the ambulance service.
Methodical considerations
There are some limitations in this study to be considered when interpreting the findings. According to the literature a focus groups interview should be conducted with 6-10 participants [13]. In this study only three participated since there are few EMTs who work until retirement in the ambulance service. The participants’ experiences may not be representative of the whole period during which the RNs started to work in the ambulance service in Sweden, but they reflect their perspective on this period, and the medical guidelines supported their experiences. Another way of exploring RNs role in the ambulance services could have been by interviewing EMTs still in the service as well as the RNs for a comparison of their perceptions. One factor that is both a limitation and strength of this study is the contextual awareness of the ambulance service by the authors. The daily practice made it possible to discuss the findings among elderly colleagues, but there is also a hazard in having contextual awareness when analyzing collected data [19]. However, this hazard was reduced by verifying the findings among clinical colleagues and by discussions among the authors. The convenient selection of medical guidelines may be a limitation, but the inclusion was made based on availability of the medical guidelines. If an edition from e.g. 2010 250 had been found, this may have clarified the development of the ambulance services to a greater extent.
Since the RNs became a part of the pre-hospital emergency care provided by the ambulance service there has been an increase in the possibilities to treat and alleviate suffering by using different medicines. There has also been a development of possibilities to steer patients to an optimal level of care instead of transporting all patients to the emergency department. This may indicate increased independence in decision-making among pre-hospital personnel after the RNs become a part of the ambulance service.
By showing the sparse descriptions on nursing and caring in the medical guidelines used in the ambulance service this study highlights the need for development of the guidelines. Medical knowledge is not sufficient alone; there is also a need for knowledge about nursing and caring relations in the ambulance service.
The authors would like to acknowledge the time, support and insights contributed by the retired EMTs and Karin Sedig, MD, ambulance physician, and wish to thank them for sharing their great knowledge of the ambulance organization.