Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Research Article - (2025)Volume 13, Issue 2
The number of deceased attributed to COVID-19 reflects the impact of the pandemic on global health. However, estimates differ considerably. For instance, in the Netherlands cause-of-death statistics reports almost 48,000 COVID-19 deaths in 2020-2022, accounting for about 11 percent of all deaths, while the Dutch registration of notifiable infectious diseases reports only 23,000 deaths due to COVID-19 in the same period. Such a (large) difference between estimates is also observed in other countries and requires an explanation.
COVID-19; Death; Coding; Perspective
The number of deceased attributed to COVID-19 reflects the impact of the pandemic on global health. However, estimates differ considerably. For instance, in the Netherlands cause-ofdeath statistics reports almost 48,000 COVID-19 deaths in 2020-2022, accounting for about 11 percent of all deaths, while the Dutch registration of notifiable infectious diseases reports only 23 000 deaths due to COVID-19 in the same period [1-2]. Such a (large) difference between estimates is also observed in other countries and requires an explanation.
The attribution of a death to COVID-19 is difficult and disputed [3-6]. Nowadays, a death certificate reports on average three causes of death [7]. Selection is inevitable for assigning the death of a person to a (one) cause for statistics. The instruction manual of the ICD-10 provides rules for such a selection in order to obtain international comparable data for health policy purpose [8]. According to these instructions, cause-of-death statistics are a tabulation of underlying causes of death, one per deceased, defined as the starting point of the causal sequence leading directly to death. This is called the General Principle (GP) of cause-of-death statistics as the selected underlying cause of death should explain all the other causes reported on a death certificate. The GP is not only part of the ICD-10, but has a long tradition covering different previous versions of the International Classification of Diseases (ICD) as well [9]. In April 2020, WHO issued a special instruction prescribing to attribute death to COVID-19 in every deceased with a natural cause of death and the disease being mentioned on part 1 of a death certificate [10]. This is a deviation from the GP. COVID-19 is considered to be caused by nothing else but itself. A causal sequence described by a certifier is neglected. This study investigates the impact of this WHO special instruction on cause-of-death statistics by comparing its application with that of the prevailing ICD-10 rules on the same data set (bridge coding study) in order to explain the different estimates of COVID-19 deaths.
Methods
A bridge coding study was performed, defined as a processing of the same set of death certificates by two different methods. Bridge coding studies were used for studying changes of classifications (e.g. ICD-9 versus ICD-10), the introduction of new coding methods (e.g. manual versus automated coding), or the introduction of new ICD-10 codes [11-12]. At its outbreak in 2019, COVID-19 was a new disease. It brought new ICD-10 codes and principles for selecting COVID-19 as underlying cause of death. The WHO special instruction issued in April 2020, prescribed to select COVID-19 as underlying cause of death for statistics when mentioned on part 1 of a death certificate in case of a natural cause of death: “The primary goal is to identify all deaths due to COVID-19. A death due to COVID-19 is defined for surveillance purposes as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma)”. And: “A death due to COVID-19 may not be attributed to another disease (e.g. cancer) and should be counted independently of preexisting conditions that are suspected of triggering a severe course of COVID-19”. This principle was incorporated in the Iris software for automated coding of death certificates by an update of September 2020, so that the WHO special instruction became part of the regular production of cause-of-death statistics in the Netherlands.
For this (bridge coding) study, all death certificates mentioning COVID-19 in 2020-2022 were recoded by the prevailing ICD-10 coding principles. The General Principle (GP) was applied when COVID-19 was reported on the lowest used line in part 1 of the death certificate, regardless any other causes mentioned on part 2 of the death certificate. When other causes of death were mentioned in part 2 of the death certificate-the position of contributory causes of death-the so-called Direct Sequel (DS) was applied. Disorders with a possible causal connectiondementia, diabetes mellitus, COPD, stroke or malignancies-were preferred as underlying cause of death despite their position on part 2 of the death certificate in the same way the ICD-10 instruction manual prescribed the DS for a pneumonia being a “clinical compatible illness” of COVID-19. The reason for applying a DS lies in the fact that although from a medical point of view the (only) cause of pneumonia is a micro-organism, a pneumonia becomes a cause of death by another disease without which the person would not have died from the pneumonia. The application of the DS rule was validated by calculating odd ratios of concomitant causes on death certificates with and without a mention of COVID-19.
Death certificates with COVID-19 on the lowest used line and no other causes mentioned require no selection. The outcome of the recoding cannot not differ from that of the routine coding process for this kind of death certificates. From a causal point of view, these records represent deaths in which COVID-19 was considered the one and only cause.
The outcome of the recoding was compared with the outcome of the routine coding process for producing cause-of-death statistics by the WHO special instruction for COVID-19 issued in April 2020. The Perfect Compatibility Percentage (PCP), i.e., the number of records that would have been coded in exactly the same way by the different coding principles, and the Comparability Ratio (CR), i.e., the ratio of the different outcomes of the different coding principles for estimates in statistics, calculated by cross tabulation, were used as measures for expressing the outcome of this bridge coding study. Shifts of underlying causes of death by the introduction of new ICD-10 codes and principles were described.
Study material
The material of this study comprised all death certificates mentioning COVID-19 as cause of death during the pandemic (2020-2022) in the Netherlands (n=51,288). In the Netherlands, for every deceased a death certificates was issued by the attending physician reporting a causal chain of morbid events leading to death (part 1 of the death certificate) or diseases contributing to death while not being part of the causal chain (part 2 of the death certificate). Death certificates were processed by Statistics Netherlands. All causes of death mentioned on a death certificate were coded and the underlying cause of death-the starting point of the causal sequence of morbid events that led to death-was selected. During the years 2020-2022, death certificates were automatically coded by Irissoftware for coding causes of death and selection of an underlying cause of death-version 5.6. All death certificates mentioning COVID-19 were reviewed manually by medical coders before being processed by Iris in order to ensure COVID-19 was coded according to the WHO special instruction as issued in April 2020. All other death certificates were coded by the rules and guidelines of the instruction manual (Volume 2) of the ICD-10 as incorporated in the software of Iris.
The sample comprised of 45.9% women and 54.1% men. The mean age of death was 83.8 years for women and 80.3 years for men. Of the deceased with COVID-19, 61% died in a nursing home, 30% in a hospital and 9% at home. Of all COVID-19 diagnoses reported, 93.6% were clinical or laboratory confirmed (ICD-10: U07.1) and 8.4% suspected (ICD-10: U07.2). Deceased with an external cause of death (suicide, accident, violence) were excluded from the sample as the WHO special instruction and the prevailing ICD-10 rules did not differ for assigning the underlying cause of death to this kind of records.
The Figure 1 shows the outcome of different coding principles applied to the same data set for each year of the pandemic. Of all death certificates mentioning COVID-19, the disease was designated as underlying cause of death for statistics by the WHO special instruction in 93.7% of the cases. In 76.2% of the cases the General Principle applied and in 49.1% of the cases COVID-19 was underlying cause of death when reported comorbidity was taken in to account by applying the DS as instructed in volume 2 of the ICD-10. COVID-19 was reported on the lowest used line of a death certificate without any other causes, i.e., as necessary and sufficient cause of death, in 33.0% of all cases mentioning the disease. The percentage of cases designated to COVID-19 as underlying cause of death decreased in the course of the pandemic due to an increase of COVID-19 reported as contributory cause on part 2 of a death certificate: From 4.7% in 2020 to 16.4% in 2022 (Figure 1).
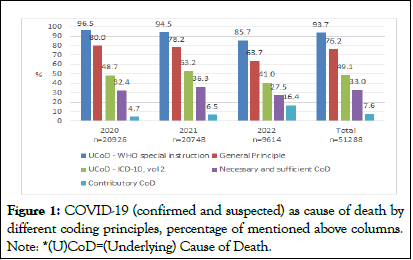
Figure 1: COVID-19 (confirmed and suspected) as cause of death by different coding principles, percentage of mentioned above columns. Note: *(U)CoD=(Underlying) Cause of Death.
Table 1 shows a crosstabulation of the number of cases with COVID-19 as underlying cause of death according to two different selection principles: The WHO special instruction for COVID-19 and the prevailing rules of the ICD-10 (volume 2) instruction manual. The Perfect Compatibility Percentage (PCP) of the two principles was 55.0%. Almost all cases considered underlying cause of death from a medical point of view were captured by the WHO special instruction too. However, too many cases were designated as underlying cause of death by the WHO special instruction. The Comparability Ratio (CR) was 1.23 with regard to the position of COVID-19 on a death certificate (General Principle) and 1.91 when the direct sequel (i.e., the causal connection between mainly neurodegenerative disorders, COPD and diabetes mellitus) was applied.
|
|
ICD-10, vol 2 rules |
||
|
|
Yes |
No |
Total |
WHO special instruction |
Yes |
25,062 |
22,980 |
48,042 |
|
No |
111 |
3,135 |
3,246 |
|
Total |
25,173 |
26,115 |
51,288 |
Table 1: COVID-19 as underlying cause of death (2020-2022).
Table 2 shows the co-occurrence of causes on death certificates mentioning COVID-19. There was a statistically significant association between COVID-19 and dementia, Parkinson’s disease, COPD, pneumonia (unspecified) and diabetes mellitus. The table 2 also shows the underlying cause of death when the regular ICD-10 coding principles would have been applied to death certificates mentioning COVID-19. In about 46% of the cases there would have been another underlying cause of death, mainly (neuro)degenerative diseases (dementia 38%, Parkinson’s disease 4%, old age 1%), COPD (11%), heart failure (5%), stroke (4%) and diabetes mellitus (3%).
| Cause of death | % on death certificates with COVID-19 | % on death certificates without COVID-19 | Odds ratio |
Upper limit | Lower limit | % UCoD according to vol. 2 ICD-10* |
| Dementia | 24.2 | 17 | 1.55 | 1.52 | 1.58 | 38.4 |
| Heart failure | 10.9 | 15.4 | 0.62 | 0.6 | 0.63 | 4.5 |
| Pneumonia | 20.5 | 7.9 | 2.76 | 2.7 | 2.83 | 1.7 |
| CVA (stroke) | 7.5 | 9.7 | 0.71 | 0.68 | 0.73 | 3.9 |
| COPD | 9.2 | 7.3 | 1.2 | 1.16 | 1.24 | 11.3 |
| Lung carcinoma | 1.8 | 7 | 0.21 | 0.2 | 0.23 | 1.2 |
| Diabetes mellitus | 9 | 7 | 1.22 | 1.19 | 1.27 | 2.7 |
| Hypertensive heart disease | 5.4 | 5.4 | 0.99 | 0.95 | 1.03 | 1 |
| Chr. ischemic heart disease | 3.7 | 4.3 | 0.81 | 0.77 | 0.88 | 1.8 |
| Myocardial infarction | 1.2 | 4 | 0.26 | 0.24 | 0.28 | 0.5 |
| Colon/rectum carcinoma | 0.7 | 3.4 | 0.18 | 0.17 | 0.2 | 0.4 |
| Old age | 1.5 | 3.8 | 0.36 | 0.34 | 0.39 | 1 |
| Mammacarcinoma | 0.8 | 2.6 | 0.28 | 0.25 | 0.31 | 0.4 |
| Prostate carcinoma | 1.1 | 2.6 | 0.38 | 0.35 | 0.41 | 0.4 |
| Pancreas carcinoma | 0.2 | 2 | 0.07 | 0.05 | 0.08 | 0.1 |
| Parkinson's disease | 2.6 | 2 | 1.29 | 1.21 | 1.36 | 4 |
| n | 51,288 | 461,776 | 24 733 | |||
| Note: *UCoD: Underlying Cause of Death | ||||||
Table 2: COVID-19 as part of conditions causing death.
This study is a bridge coding of death certificates mentioning COVID-19. The coding of death certificates by the WHO special instruction for COVID-19 was compared with the coding of death certificates by the prevailing rules of the ICD-10 (Volume 2) instruction manual. In 94% of the cases mentioning COVID-19, the disease was selected as underlying cause of death for statistics by the WHO special instruction. In 76% of the cases mentioning COVID-19, it was reported as the beginning of the causal chain leading to death, i.e., the general principle of the ICD-10 instruction manual applied. With the occurrence of co-morbidity taken in to account (DS applied), COVID-19 was underlying cause of death in 49% of the deceased cases. COVID-19 was reported as necessary and sufficient cause of death in 33% of the deceased cases. The perfect compatibility between the two principles was 55%. In case of discrepancy, the special WHO instruction led to a replacement of (mainly) neurodegenerative diseases and COPD by COVID-19 as underlying cause of death.
Up to date, no other (published) bridge coding studies on COVID-19 are encountered in medical literature. Grippo et al studied death certificates mentioning COVID-19 in 2020 and found it to be the underlying cause of death in 88% of cases. This finding is in line with the finding of this study for the year 2020 (80%). Grippo et al., reported comorbidities in 72% of the death certificates, with little variation by age and gender. A finding also in line with the outcome of this study (67%). The Italian study was conducted in the beginning of the pandemic (2020). This study covers the course of the pandemic showing a decrease of COVID-19 as underling cause of death and increase of COVID-19 as contributing cause of death.
This bridge coding study also shows in 49% of the cases COVID-19 remained the underlying cause of death when the role of contributory causes reported in part 2 of the death certificate is taken in to account. As there are no other bridge coding studies available yet, this estimate cannot be compared with other research. However, this percentage is in close alliance with the outcome of the Dutch mandatory registration of infectious diseases, reporting 23,000 COVID-19 deaths over the period of 2020-2022. The mandatory registration of infectious diseases reflects physician’s opinions on COVID-19 as the cause of death, while cause-of-death statistics identify every death in which COVID-19 played a role (underlying or contributory) in dying.
The different outcomes of these different coding principles can be explained by a different purpose of classification on the one hand and by a different idea of causality on the other. The WHO special instruction is motivated by surveillance. Deceased dying with COVID-19 are monitored to inform about the course of the pandemic. The regular ICD-10 rules for assigning an underlying cause of death are bases on medical causal considerations, i.e., the observation by a physician of a chain of events in time being connected by a pathophysiological mechanism. The start of such a causal chain leading to death can be the object of an intervention (therapy or prevention) preventing death.
The WHO special instruction of April 2020 serving surveillance is an exception to the ICD coding rules captured by a few pages as part of the ICD-6 to a complete volume of rules in the ICD-10 serving medical causality. Such an exception is not new. It is also used for selecting influenza as cause of death. However, the number of cases dying with influenza is even during an epidemic outbreak (about 0.3% of the deceased) much less than the number of COVID-19 deaths (11% of the deceased). So, the impact of the exception during the COVID-19 pandemic was large. The purpose of surveillance might be questioned as there are other registrations serving this purpose as well, for instance the mandatory registration of infectious diseases showing the same course of the pandemic or the registration of positive screening tests. The special WHO instruction also led to an ambiguous interpretation of cause-of-death statistics. In the years 2020-2022, the majority of causes (89%) operate as the start of a causal chain leading to death, while the most frequently occurring cause of death (11%), COVID-19, is selected when being mentioned on a death certificate regardless its role as cause of death.
As the name implies, cause-of-death statistics incorporate causal theory and classify the role of a disease in dying. This qualification requires a medical point of view as pathophysiological mechanisms form the causal connecting elements between diseases or disorders being reported on a death certificate. First of all, COVID-19 can be considered a necessary and sufficient cause of death when reported as the only cause on a death certificate or as start of the causal chain without additional co-morbidity. This appeared to be the case in 33% of the deceased cases. However, in 67% of the deceased cases there was a cooperation of COVID-19 with other diseases causing death. According to causal theory, COVID-19 is an Insufficient, but Necessary part of an Unnecessary but Sufficient (INUS) condition in these deceased cases. This means the patient would not have died at that particular moment in time without attracting the virus. However, comorbidity is required for dying. COVID-19 is a necessary part of a combination of diseases sufficient for causing death. As there is not a fixed combination of causes, each combination as such is a sufficient, but not a necessary cause of death. With regard to infectious diseases such as COVID-19, current cause-of-death statistics identify so called INUS conditions underlying death, but do not provide a full description of such a condition. For this death certificates reporting other causes beside COVID-19 have to be studied.
In studying COVID-19 as part of an INUS condition, there appeared to be a statistically significant association between COVID-19 and dementia, Parkinson’s disease, COPD, pneumonia and diabetes mellitus. Other studies confirm this role of co-morbidity in death. It is the immuno-senescence in case of neurodegenerative diseases and the change of ACE2 receptors in case of COPD or diabetes that causally connects them with COVID-19. It makes COVID-19 a part, not the start of a causal chain. It justifies the application of the DS. With these pathophysiological mechanisms, i.e., the GP and DS, taken in to account, the estimate of COVID-19 deaths would have been about half than currently reported by cause-of-death statistics.
Our study presents significant advancements in linguistics by exploring the imagery-topology hypothesis and its application to lexical semantic and grammatical structures. Addressing our research questions, we have elucidated the intricate relationships between lexical semantics, conceptual metaphors, and topology within linguistic frameworks. We demonstrated how spatial concepts and imagery-topology influence cognitive schemas in both lexical semantic and grammatical structures and identified culturally marked cognitive factors in various languages. The two innovative models developed–the grammar construction model and the Lexical semantic structure model–highlight the essential role of spatial concepts in cognitive development and their profound impact on linguistic comprehension. These models serve as effective tools in addressing challenges in universal linguistics, offering new perspectives for future research aimed at understanding the spatial cognitive underpinnings of language.
Strengths and limitations
Strong point of this study is its material. The role of COVID-19 as cause of death is studied by death certificates. Different perspectives were identified and their impact on cause-of-death statistics explained. This provides new information for the often heated debate about the number of COVID-19 deaths. Different estimates represent different views on COVID-19 as cause of death. With regard to age and sex, the sample of death certificates studied can be considered representative for COVID-19 deaths in high income countries. As there are no other bridge coding studies identified in literature yet, the findings in this study require replication to validate its outcome.
A limitation of this study is the proper completion of a death certificate. The certifier will have to determine whether a patient would have died if she had not had the particular disease or condition (counterfactual) or not. This is more difficult for a new disease like COVID-19 than for diseases with a known pathophysiological mechanism. Underreporting of causes on death certificates has to be considered.
Also, the mention of COVID-19 on a death certificate provided no information about the clinical severity of the disease. A positive test result or a fully developed clinical syndrome could not be distinguished, and in accordance with the WHO special instruction both were coded (ICD-10: U07.1) and selected as underlying cause in the same way. The fact that 91% of the deaths involved in this study are nursing home residents or hospitalized patients, supports the interpretation of COVID-19 on a death certificate as a developed clinical syndrome. However, this remains to be confirmed by other studies (e.g. a comparison of death certificates with clinical records).
According to Dutch Civil Law (Article 7: 458) no ethical approval is required for a secondary analysis on non-identifiable data of deceased persons.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Harteloh P (2025) COVID-19 Deaths: Different Estimates from Different Perspectives-A Bridge Coding Study. Infect Dis Preve Med. 13:408.
Received: 07-Jun-2024, Manuscript No. JADPR-24-31924; Editor assigned: 10-Jun-2024, Pre QC No. JADPR-24-31924 (PQ); Reviewed: 24-Jun-2024, QC No. JADPR-24-31924; Revised: 15-May-2025, Manuscript No. JADPR-24-31924 (R); Published: 22-May-2025 , DOI: 10.35841/2329-8731.25.13.408
Copyright: © 2025 Harteloh P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.