Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Short Communication - (2023)Volume 11, Issue 3
Coronaviruses were initially discovered in 1964 by June Almeida in Glasgow. In order to comprehend how a disease manifests we have to understand the anatomy, physiology, and pharmacology of the body as well as the modus operandi of the pathogen. COVID targets the ACE-2 receptor of the body and like other similar viruses e.g. Middle East Respiratory Syndrome virus (MERS). COVID-19 is a biphasic condition if left unchecked results in embolism. The first step is a viremic phase which lasts 7 days-10 days where a four-phase approach can bring the viral load down. The second step is a host mediated reaction with a cytokine storm and thrombosis which requires medications from the first step along with high dosage steroids and additional medications to stop the cytokine storm and thrombosis. COVID has killed over a million people in the US, the fauci approach of stay at home for 2 weeks and return to your physician if there is a problem loses the valuable opportunity of stopping the progression of this condition in the viremic phase. We have to stop living in fear, be bold and move forward.
COVID-19; ACE-2 receptor; Viremic phase; Thrombosis; MERS virus
In order to comprehend how a disease manifests we have to understand the anatomy, physiology, and pharmacology of the body as well as the modus operandi of the pathogen. COVID targets the ACE-2 receptor of the body and like other similar viruses e.g., Middle East respiratory syndrome virus encroaches on the pulmonary CD4 cells resulting in secondary atypical infections [1].
ACE-2 receptors are ubiquitous in the epithelia of the body. ACE enzymes activate bradykinin resulting in increased cellular permeability. The net result of activation is a collection of fluid which is mopped up by secretion of hyaluronic acid notably in the lungs giving the appearance of ground glass on X ray and CT scans (Figure 1).
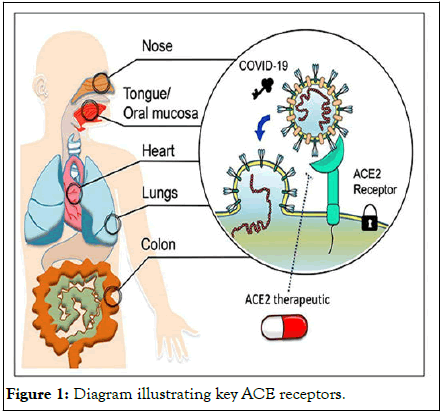
Figure 1: Diagram illustrating key ACE receptors.
As the ACE-2 pathways are activated the patient feels acutely short of breath with fluid accumulation in the alveoli, and in the pulmonary vessels this activation of ACE-2 receptors leads to a pulmonary embolism if left unchecked. In the gastrointestinal system the activation causes secretions of fluids with resultant diarrhea. Activation in the olfactory neuroepithelium results in loss of smell and COVID transverses into the basal cisterns causing inflammation with sequential headaches [2-4]. The resultant increase in pressure in the basal cisterns results in elevated intracranial pressure with subsequent release via the internal auditory canal causing enhancement of the mastoid segment of the facial nerve and mastoiditis [5,6]. ACE-2 inhibitors, ARB blockers and Ibuprofen up regulate ACE-2 expression. AVOID Ibuprofen for fever.
The body also has a novel cytokine signaling pathway activated by the JAK2 pathway that can be blocked by JAK2 inhibitors e.g., famotidine, apoquel and baricitinib limiting the progression pathway set up by ACE-2 receptor activation (Figure 2) [7,8].
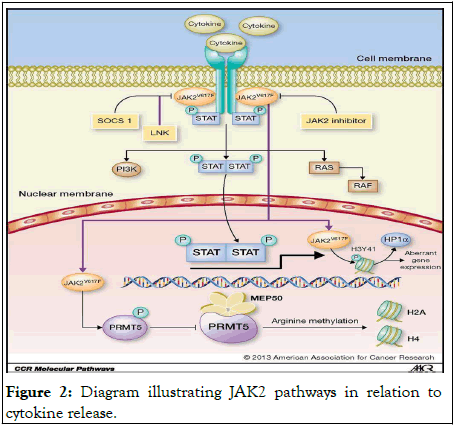
Figure 2: Diagram illustrating JAK2 pathways in relation to cytokine release.
COVID-19
Coronaviruses were initially discovered in 1964 by June Almeida in Glasgow. They are common commensals found in the back of the nose and throat. They have a hallmark crown type accessories externally which harbors the spike protein to attach to the ACE receptor. Internally it is an RNA virus with 16 gene fragments of HIV1, HIV2 and SIV9. COVID-19 is 1000 times more powerful in attaching to the spike protein compared to Almeida coronaviruses (Figure 3) [9].

Figure 3: Cross section through COVID-19 virus.
COVID-19 sits on facial hair and ventilation systems, studies from Bergamo and Harvard confirm it sits on particulate matter in the air, hence higher incidences of COVID in more polluted atmospheres [10,11].
Bronchoalveolar lavages of COVID-19 patients show elevated levels of hyaluronic acid due to up-regulation of hyaluronan synthases and down regulation of hyaluronidase [12].
Combined with increased lung hyperpermeability from bradykinin release hyaluronic acid mops up fluid. Hyaluronic acid inhibits gas exchange, damages alveoli in inappropriate ventilator settings. (US have the highest mortality rate) (Figure 4).
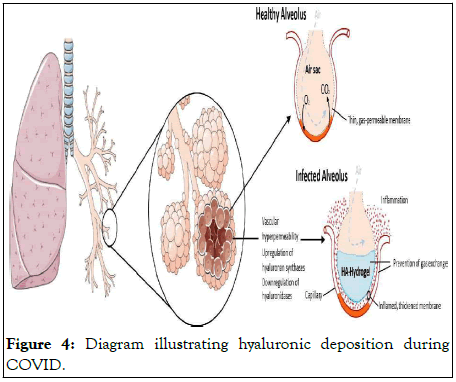
Figure 4: Diagram illustrating hyaluronic deposition during COVID.
COVID-19 treatment
COVID-19 is a biphasic condition if left unchecked results in embolism. The first step is a viremic phase which lasts 7 days-10 days where a four-phase approach can bring the viral load down.
The second step is a host mediated reaction with a cytokine storm and thrombosis which requires medications from the first step along with high dosage steroids and additional medications to stop the cytokine storm and thrombosis. Sadly, studies have been done using antivirals without adequately dosed steroids in the second step of this condition reflecting a poor understanding of the disease (Figure 5).
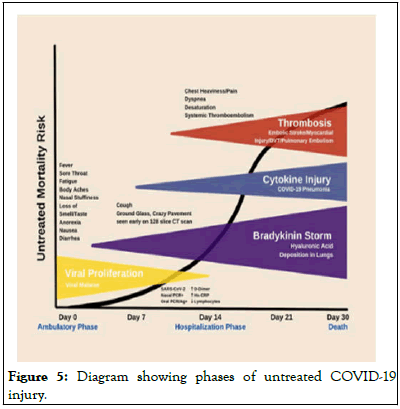
Figure 5: Diagram showing phases of untreated COVID-19 injury.
The above diagram summarizes COVID-19 injury with clinical signs and phase of the disease.
Step 1 phase zero treatment
The objective is to decrease viral load and prevent adherence of the spike protein to the ACE-2 receptor (Figure 6).
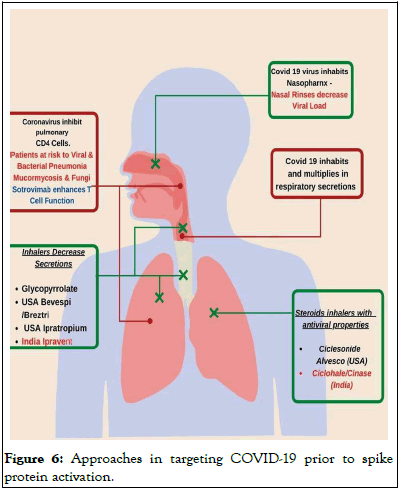
Figure 6: Approaches in targeting COVID-19 prior to spike protein activation.
This can be done by nasal rinses targeting the back of the nose/throat area with normal saline. It is simple and most effective as COVID sits at the back of the nose/throat.
Additionally, inhalers dry up the respiratory secretions such as bevespi or ipratropium bromide. Other inhalers with antiviral and steroid properties such as Alvesco and Pulmicort should be used with a drying inhaler.
Step 1 phase 1 treatment
The objective here is to prevent Spike protein adhering to the ACE-2 receptors and stop the bradykinin storm. Monoclonal antibodies prevent adherence but can take 2 to 6 days for the viral load to come to zero. Hence it is important to watch out for thromboembolic phenomenon. Benadryl allergy or Zyrtec will shut down the bradykinin storm (Figure 7).
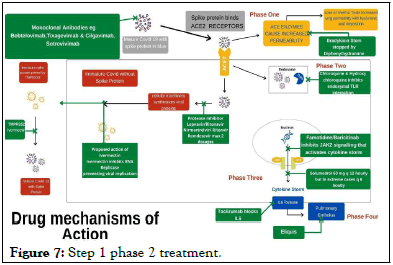
Figure 7: Step 1 phase 2 treatment.
This acknowledges that the spike protein of COVID-19 has adhered to the ACE-2 receptor and the drugs target viral multiplication. These include hydroxychloroquine which containerizes COVID-19. Protease inhibitors such aslopinavir/ritonavir.
Nirmatrelvir/ritonavir and remdesivir which target viral replication. Additionally, ivermectin can also be used as it inhibits RNA replicase and is a TMPRSS2 inhibitor preventing the attachment of the mature spike protein.
I normally use both a protease inhibitor and HCQ together to expedite viral load reduction. Those who do have reliable sources of ivermectin I encourage the addition of 12 mg of ivermectin daily. Higher dosing can cause dizziness, tachycardia, uveitis, and keratitis resulting in diminished visual acuity. It is important to realize that COVID is a highly inflammatory condition and daily 325 mg aspirin reduces the risk of vascular occlusive disease.
Step 1 phase 3 treatment
The objective here is to stop the cytokine storm using JAK 2 inhibitors that cytokine release like famotidine, apoquel and baricitinib. Famotidine at 80 mg per day shuts down the cytokine storm.
Step 2 treatment (phase 4)
This presents after 10 days or has had subtherapeutic earlier treatment. The objective is to decrease inflammation by using high dose steroids e.g., prednisones 60 mg bid and treat any thrombo-embolic diseases with Eliquis. Very often people need oxygen supplementation. Cura signa has developed an oxygen concentrator capable of delivering 10 L of continuous oxygen in a non-hospital setting, significantly more than the standard 6 L of continuous flow that is adhered to. Interleukin 7 blockers e.g., tocilizumab is used at this stage to quell the cytokine storm.
Additionally, as we precede outwards the risk of atypical bacterial infections and atypical viruses increase mandating clarithromycin/levofloxacin or valacyclovir.
Clinically it is difficult to break down the individual phases hence I treat giving a 10 days regimen of all the drugs listed from the time I first see the patient.
Patient 1
44 male presents after Xmas family gathering. PMHX: Type 1 diabetes × 39 yrs., BMI 36, sleep apnea, ARDS 2004 with:
• Intermittent dry cough × 7 days
• Sore throat × 3 days
• Diarrhoea 1-2 days
• Constant headache × 5 days
• New onset shortness of breath pulse oximetry 95% with fever
× 1 day no chills
• Loss of taste and smell × 5 days
• COVID PCR positive
Started on kaltura (lopinavir/ritonavir), hydroxychloroquine, aspirin, clarithromycin, benadryl, clarithromycin, medrol dose pack (Figure 8).
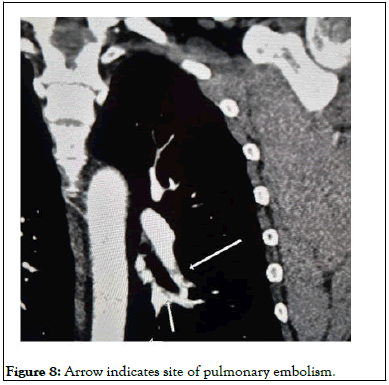
Figure 8: Arrow indicates site of pulmonary embolism.
• Patient referred to monoclonal antibody center, He received
bamlanivimab (the then current monoclonal antibody)
infusion on day 9
• The infusion staff told him everything OK and they will call
him in a week
• Patient did not follow up as requested for daily checks
• Patient returns on day 14 short of breath on walking up I
flight stairs
CT angiogram chest:
• Additionally, CT scan showed multiple ground glass opacities
in both lungs compatible COVID Pneumonitis.
• Patient refuses hospitalization, as sister placed on ventilator in
ICU
Patient started on:
• Eliquis 10 mg bid for pulmonary embolism famotidine 40 Mg
qd. started
• IV solumedrol 60 mg bid × 5 d and prednisone taper.
• IV ceftriaxone 2 gm qd x 5 days followed by oral
clarithromycin 500 mg bid. Incentive spirometry
• 10 days after monoclonal antibody infusion, the patient
develops fever and chills. Started on valtrex 1 gm tid × 7 days.
Chills resolved after 24 hours
• Patient returned to work 3 weeks after initial COVID
infection. His sister returns home 4 weeks after the initial
COVID infection with supplemental oxygen.
Patient 2
• A 67-year-old 115 lb. female horse dressage trainer presents 12
days after a positive COVID test. PMHx significant for asthma
• She had seen a MD who had prescribed her amoxicillin-clavulanate
875 mg-125 mg and prednisone 60 mg qd for 10
days.
• She was acutely short of breath and still COVID positive.
Started on:
• Aspirin 325 mg.
• Lopinavir/Ritonavir 200-50 two tabs bid #40.
• HCQ 200 mg 2 tabs bid #40.
• Prednisone 60 mg bid.
• Clarithromycin 500 mg bid.
• Famotidine 40 g bid.
• Benadryl 25 mg am and cetirizine 10 mg qhs.
• Breztri and Alevesco 2 puffs twice daily.
• CT angiogram of the chest ordered.
• CT angio chest confirms the right lower lobe pulmonary
embolus.
• Globular ground glass appearance in both lung fields
consistent with COVID 19 and scarring of both lung bases.
• Started patient on Eliquis 10 mg bid x week
• Started patient on IV Ceftriaxone 2 gm and solumedrol 60
mg bid x 5 days
• On day 18 of COVID patients get yeast infection and senses
onset of oral Herpes.
• Patient started on valacyclovir 1 gm tid x week and given
fluconazole 150 mg qd.
• Oxygen saturation restored to 95% and at home oxygen at 2 L
started. On day 20 of COVID oxygen saturation 97 %.
• On day 21 of COVID solumedrol dropped to 60 mg qd.
• On day 22 of COVID oxygen saturation 98% on 2 L oxygen
started on incentive spirometry and clarithromycin 500 mg
bid.
• Over the next 6 weeks steroids decreased and oxygen stopped.
Patient 3
A 59-year-old male patient who recently received a heart transplant on immunosuppressive medications with a past medical history of insulin dependent diabetes, sleep apnea gets sore throat, fever and chills from his children who tested positive for COVID. He tests positive for COVID, The patient was directed to the transplant unit who admitted him and gave him four dosages of remedy, closely monitoring his renal function. He was discharged 5 days later with a bronchitic cough, producing green phlegm with low grade fever and chills. Patient was started immediately on lopinavir/ritonavir. HCQ, clarithromycin, benadryl and pulmicort inhaler, within 10 days chest is clear with no symptoms.
COVID has killed over a million people in the US, the Fauci approach of stay at home for 2 weeks and return to your physician if there is a problem loses the valuable opportunity of stopping the progression of this condition in the viremic phase. The net result is we have established physicians who do not comprehend that COVID is a two-step disease. The initial step is viremic then the dangerous host reaction which can be stopped by high dose steroids. We have to look in the mirror and understand our willful ignorance is the cause of the million dead in the USA today. We have to stop living in fear, be bold and move forward.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mangat H (2023) COVID-19 and its Different Phases of Treatments. J Infect Dis Preve Med. 11:301.
Received: 19-Jan-2023, Manuscript No. JADPR-23-23603; Editor assigned: 20-Jan-2023, Pre QC No. JADPR-23-23603 (PQ); Reviewed: 03-Feb-2023, QC No. JADPR-23-23603; Revised: 25-Apr-2023, Manuscript No. JADPR-23-23603 (R); Published: 02-May-2023 , DOI: 10.35248/2329-8731.23.11.301
Copyright: © 2023 Mangat H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.