Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Research Article - (2022)Volume 11, Issue 3
Torsion of the Spermatic Cord (TCS) is a serious surgical emergency. It corresponds to a rotation on a vertical axis of the testicle resulting in the formation of coil turns at the level of the spermatic cord causing the cessation of blood flow or even testicular ischemia. This pathology is responsible for rapid testicular necrosis resulting in the loss of functions of the ipsilateral gland with the possibility of subsequent impairment of fertility. It is therefore a real emergency.
Torsion of the spermatic cord; Ischemia; Ipsilateral gland
Many TCS are still operated on very late, due to the negligence of the patients, especially adolescents or their parents, or sometimes due to ignorance of the diagnosis, especially in adults. Such an event may result in a low rate of testicular salvage. Our retrospective study was carried out in order to verify the apparently increasing incidence in our institution, to determine the risk factors and to evaluate the diagnostic, therapeutic and prognostic aspects of TCS in adolescents and young adults in the urology department of the CHU IBN ROCHD of Casablanca [1,2].
This work is a descriptive retrospective study of a series of 91 cases of torsion of the spermatic cord confirmed surgically and taken care of in the urology department of the CHU IBN ROCHD of Casablanca, over a period which extends from June 2015 to the month of June 2019.
All the cases retained for the study had torsion of the spermatic cord and were all operated.
• The first step was to draw up an exploitation sheet for the clinical records.
• The second step consisted in collecting the data relating to each file on the Clinical record.
• The third step concerned the analysis of the data of the series considered.
Inclusion criteria
The cases included in this study were adolescent patients aged 14 to 19 years (according to the WHO an adolescent is between 10 and 19 years old); given that the service only supports patients over the age of 14; and young adults (20-40 years old) with TCS, hospitalized and operated on at the urology department of the IBN ROCHD University Hospital Center (CHU) in Casablanca.
Exclusion criteria
• Teenagers under the age of 14.
• Adults over 40 years old.
Were studied 91 files of torsion of the spermatic cord?
During the period studied, a total of 1640 surgical emergencies were treated in our department, 91 were for TCS, i.e. a prevalence of 6%and an average incidence of 23 cases per year.
•The average age of our series was 17 years (the extremes: 14 years and 37 years) The distribution according to age (figure1).
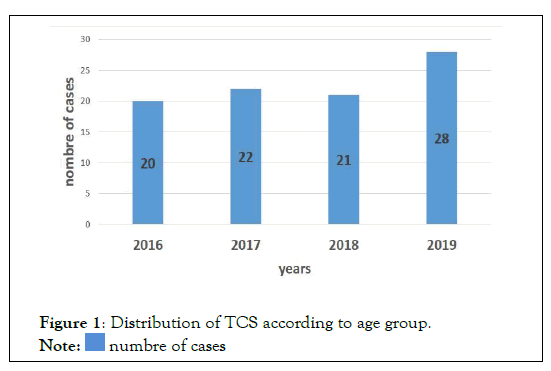
Figure 1: Distribution of TCS according to age group.

Antecedents
•Similar episode resolved spontaneously (subtortion):10 Cases (11%) including 3 cases reporting several similar episodes.
•Scholarship trauma:1 Case.
•Bilateral scrotal trauma occurring 2 years before TCS in an 18-year-old adolescent.
•Cryptorchidism:1 Case.
•In a 27-year-old patient, operated on at the age of 5 for left cryptorchidism, TCS occurred on the left side.
•Surgical treatment of an inguinal hernia:2 cases.
•In 2 adolescents aged 14 years operated respectively at the age of 4 years and 6 years; torsion occurred on the opposite side of the hernia repair in both cases.
Comorbidities
•Trisomy 21: 1 Case.
Socio-professional activities
•In 10 cases (11%), we identified occupations requiring intense physical effort (Figure 2).
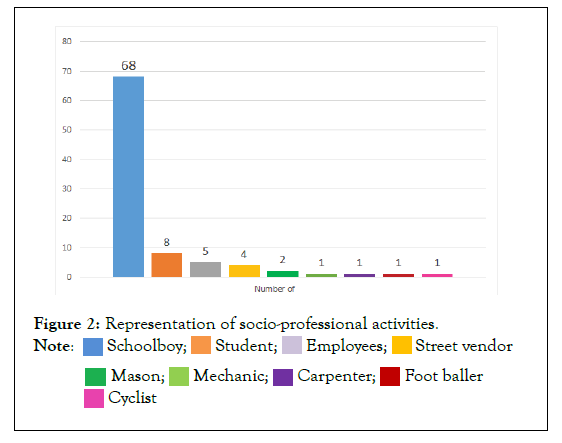
Figure 2: Representation of socio-professional activities.
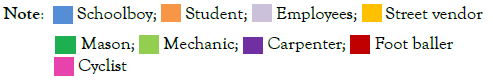
The seasonal distribution
More than 60%of the patients in our series were operated on fall and in winter (Figure 3).
Figure 3: Seasonal distribution of the TCS (%).

Circumstances of occurrence of TCS
•At rest: 54 Cases.
•During sleep: 29 Cases.
•Scholarship trauma: 4 Cases.
•Intense physical exertion: 2 cases (a footballer, a cyclist).
•Exposure to cold : 2 cases (cold bath).
Thus, a sudden tensioning of the fibers of the cremaster by a triggering factor is found in 8 cases (9%).
The affected side
The TCS was on the side left in 58% versus 42% from the side straight.
Clinical study
The diagnostic delay: Sixty-four cases had a delay of more than 6 hours (Figure 4).
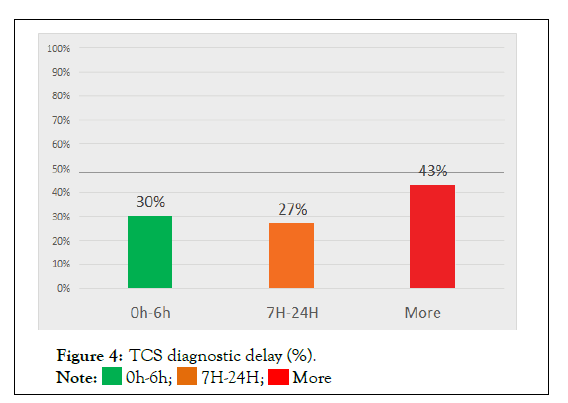
Figure 4: TCS diagnostic delay (%).
This delay was due to:
•The understatement the severity of the symptomatology or the neglect of the parents or the patient (59%).
•Ignorance diagnosis in cases consulting first in other health establishments (peripheral hospital, health center, private practice) (28%).
•Self-medication by pharmaceutical analgesics, ice pack or herbal massages (11%).
•A delay in support in the case of a prisoner.
Clinical signs
• The clinical signs are dominated by spontaneous scrotal pain in 88 cases (97%) (Table 1).
| Clinical signs | Number of cases | Percentage (%) |
|---|---|---|
| Spontaneous scrotal pain | 88 | 97 |
| Nausea and vomiting | 22 | 24 |
| Inguinal pain | 10** | 11 |
| Lower back pain | 3 | 3 |
| Very annoying scrotal pain when walking | 3 | 3 |
| Fever | 4* | 4 |
Note: * Temperature between 38°c and 38.4°c;** Left TCS on cryptorchid testicle in one case.
Table 1: The clinical signs of TCS.
• The intensity of scrotal pain on admission according to the visual analogue scale varied according to the time to diagnosis. The longer the delay, the less pain (Table 2).
| Diagnostic delay | No scrotal pain | Moderate scrotal pain | Intense scrotal pain |
|---|---|---|---|
| <6 hours | 1 | 17 | 9 |
| Between 6 a.m. and 24 a.m. | 1 | 20 | 4 |
| >24 hours | 27 | 12 | - |
Table 2: Intensity of scrotal pain according to the visual analogue scale according to the diagnostic delay.
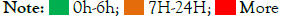
Clinical examination
The clinical signs of orientation towards a TCS are not systematic. The ascended testicle was the most found in 40 cases (44%). On the other hand, the abolished cremasteric reflex was sought only in 5 cases (5%) (Figure 5).
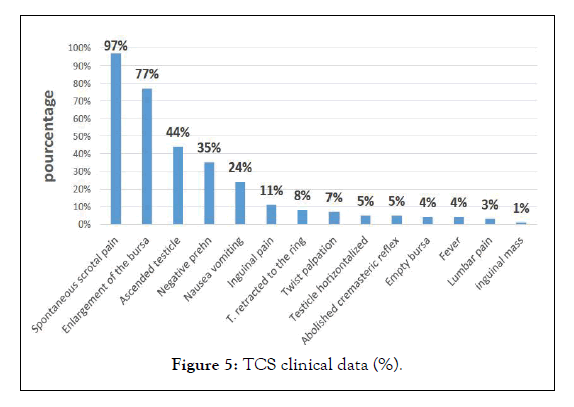
Figure 5: TCS clinical data (%).
Para clinical study
Scrotal ultrasound
Indications: Scrotal ultrasound was indicated in case of diagnostic doubt or TCS seen late.
Thereby, 28 patients underwent scrotal ultrasound either 31% cases (Tables 3 and 4).
| Diagnostic delay | Number of cases | Percentage % |
|---|---|---|
| <6 hours | Feb-27 | 7 |
| Between 7 hours and 24 hours | Aug-25 | 32 |
| >24 hours | 18/39 | 46 |
Table 3: Scrotal ultrasound in case of TCS according to diagnostic delay.
| Scrotal ultrasound | Number of cases | Percentage (%) |
|---|---|---|
| TCS direct sign | ||
| CS spire tower | 24 | 86 |
| Indirect sign of the TCS | ||
| Heterogeneous echostructure | 22 | 79 |
| Increase in testicular size | 23 | 83 |
| Hydrocele | 28 | 100 |
| Thickening of the scrotal envelopes | 8 | 29 |
Table 4: Data from scrotal ultrasound in case of TCS.
Results: Scrotal ultrasound made it possible to visualize number of twists (TS) in 24 patients (86%) (The extremes ½ to 2 Twists) (Figure 6).
Figure 6:Scrotal ultrasound showing two Twists of the left SC (snail shell image). (14h delay) (Photo Department photo).
The other signs are related to the delayed diagnosis.
Inguinal ultrasound: It found in a 1 case a twisted left testicle crypt orchid of inguinal seat with a turn of the spire and hydrocele of low abundance with a delay of 3 hours.
In another case, it found a crypt orchid right testicle of reduced size (29*12 mm) at the level of the middle orifice of the inguinal canal contralateral to the left TCS (Table 5).
| The ultrasound sign | Diagnostic delay | ||
|---|---|---|---|
| 0 h-6 h | 7 h-24 h | More than 24 hours | |
| CS spire tower | 2 | 6 | 17 |
| Heterogeneous echostructure | - | 4 | 18 |
| Increase in Testicular Size | 2 | 4 | 17 |
| Hydrocele | 3 | 8 | 18 |
| Thickening of the scrotal envelopes | - | 2 | 6 |
Table 5: Correlation between ultrasound data and TCS diagnostic time(cases).
Color doppler: Ultrasound was coupled with Doppler in 25 cases out of 29(86%). The latter was indicated to look for a perfusion anomaly. Testicular perfusion as a function of diagnostic delay (Figure 7).
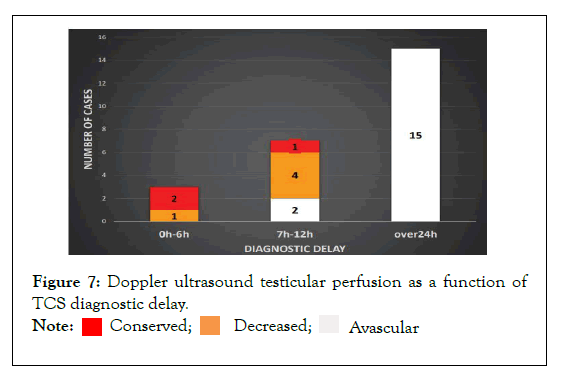
Figure 7:Doppler ultrasound testicular perfusion as a function of TCS diagnostic delay.
The treatment
Surgical exploration time: Sixty-two patients were sent directly to the operating room (68%). Thus, the time between admission and surgical exploration does not exceed a maximum of 30 minutes.
The other patients were sent to the operating room after performing an ultrasound in front of a doubtful clinical picture of TCS. In this case, the time between admission and surgical exploration varies between 40 minutes and one hour.
The surgical approach
• Scrotal incision transverse in 83 cases (91%); unilateral in 56 cases and bilateral in 27 cases for contralateral orchidopexy at the same time.
• Longitudinal incision median raphe in 7 cases (8%) for contralateral orchidopexy at the same time.
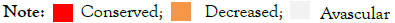
• A case was approached via the inguinal route for TCS on the crypt orchid testicle (Figure 8).
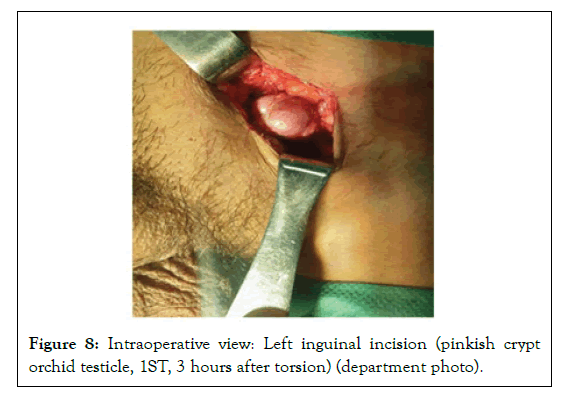
Figure 8:Intraoperative view: Left inguinal incision (pinkish crypt orchid testicle, 1ST, 3 hours after torsion) (department photo).
• A contralateral inguinal incision for contralateral cryptorchidism was performed in 3 cases at the same time.
Surgical exploration: The TCS was at the scrotal level in 90 cases and at the inguinal level on the testicle in left inguinal cryptorchidism in one case. The SC twists were found at 79 patients (87%). The extremes are ½ and 4 Twists. Correlation between the number of Twists of the Doppler spiral and surgical exploration according to the Delay between surgical exploration and treatment (Table 6).
| No. | Ultrasound(TS) | Surgical exploration(TS) | Surgical act |
|---|---|---|---|
| 1 | 0 | 2 | Orchidopexy |
| 2 | 1 | 1 | Orchidopexy |
| 3 | 1 | 0 (TCS stigmata) | Orchidopexy |
| Delay 6 hours | |||
| 4 | 1/2 | 1/2 | Orchidopexy |
| 5 | 1 | 1 | Orchiectomy |
| 6 | 1 | 1 | Orchiectomy |
| 7 | 1 | 0 (TCS stigmata) | Orchidopexy |
| 8 | 1 | 3 | Orchidopexy |
| 9 | 0 | 1 | Orchidopexy |
| 10 | 1 | 1 | Orchiectomy |
| 11 | 0 | 2 | Orchidopexy |
| 12 | 1 | 3 | Orchiectomy |
| 13 | 2 | 2 | Orchiectomy |
| 14 | 1 | 2 | Orchiectomy |
| 15 | 1 | 2 | Orchiectomy |
| 16 | 1 | 2 | Orchiectomy |
| 17 | 0 | 1 | Orchiectomy |
| 18 | 1 | 2 | Orchiectomy |
| 19 | 1 | 1 | Orchiectomy |
| 20 | 1 | 1 | Orchiectomy |
| 21 | 1 | 2 | Orchiectomy |
| 22 | 1 | 0 (TCS stigmata) | Orchiectomy |
| 23 | 1 | 1 | Orchiectomy |
| 24 | 1 | 3 | Orchiectomy |
| 25 | 1 | 1 | Orchiectomy |
| 26 | 1 | 2 | Orchiectomy |
| 27 | 1 | 1 | Orchiectomy |
| 28 | 1 | 1 | Orchiectomy |
| 29 | 1 | 1 | Orchiectomy |
Note:  False negatives.
False negatives.
Table 6: Comparison between the results of the Doppler ultrasound and the surgical exploration concerning the number of TS of the TCS.
Appearance of the testicle: Pinkish staining designates a viable testicle while blackish staining designates a non-viable necrotic testicle. The testicles with a purplish or bluish color are placed in a compress soaked in warm serum to obtain vasodilation and the Recoloration is observed. If the testicle regains its pinkish color it is viable, otherwise the testicle is non-viable. A Hydrocele associated was found in 79 cases (87%) (Figures 9 and 10).
Figure 9: Testicular staining on surgical exploration (%)
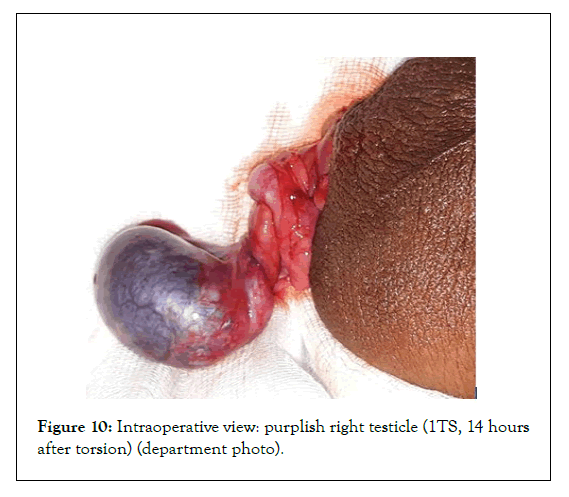
Figure 10:Intraoperative view: purplish right testicle (1TS, 14 hours after torsion) (department photo).
Surgical procedure and indications
Orchidopexy: The testicles were fixed with 3 stitches using a 4/0 non-absorbable suture at the level of the median face, lateral face and at the lower pole. All cases with a surgical exploration time of less than 6 hours benefited from orchidopexy.
The case presenting a TCS on cryptorchidism had on exploration a pinkish testicle with 1 SC twist. He underwent lowering with orchidopexy and contralateral orchidopexy (Figure 11).
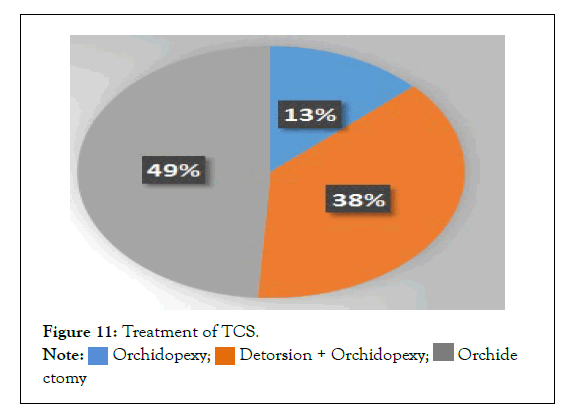
Figure 11: Treatment of TCS.
Contralateral side: All cases benefited from contralateral orchidopexy. It was performed at the same time of surgery in 34 cases (including 27 cases by transverse scrotal incision and 7 cases by longitudinal incision of the median raphe) and deferred in the remaining cases for risk of infection. Cases with contralateral crypt orchid testicles underwent lowering and orchidopexy.
Orchiectomy
It was performed after mass ligation of the spermatic cord above the seat of the TCS.
• Necrotic or non-viable twisted testicles after revitalization measures underwent orchiectomy in 45 cases.
• Ninety seven percent of cases with a surgical exploration time of more than 24 hours benefited from an orchiectomy.
The 45 cases benefiting from orchiectomy had a number of SC twists ranging from 0 to 3 Twists and a delay greater than 6 hours.
• The preservation rate according to the time of surgical exploration (Figure 12).
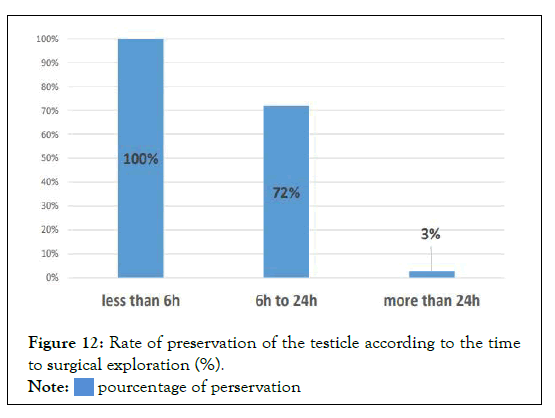
Figure 12:Rate of preservation of the testicle according to the time to surgical exploration (%).

• Correlation between the number of SC twists and the Delay to surgical exploration (Table 7).
| Surgical exploration time (hours) | ||||||
|---|---|---|---|---|---|---|
| TS | 0 H-6 H | 7 H-24 H | +24 H | |||
| O.pexy | O.ectomy | O.pexy | O.ectomy | O.pexy | O.ectomy | |
| 0 | 5 | - | 6 | - | - | 1 |
| ½ | 1 | - | 1 | - | - | - |
| 1 | 8 | - | 7 | 5 | 1* | 19 |
| 2 | 12 | - | 2 | 2 | - | 14 |
| 3 | 1 | - | 1 | - | - | 4 |
| 4 | - | - | 1 | - | - | - |
| Total | 27 | - | 18 | 7 | 1 | 38 |
| 91 | ||||||
Table 7: Correlation between surgical exploration time, the number of SC twist and the surgical Act.
This is a 14-year-old adolescent admitted with a left TCS after a delay of 25 hours. On clinical examination: large inflammatory left purse with a temperature of 38.4°. An anti-inflammatory treatment was prescribed on day 1 without improvement. On scrotal ultrasound: heterogeneous left testicle increased in size, as well as the epididymis head. On Doppler: absence of intra testicular vascularization, with peripheral vascularization. On surgical exploration: one SC twist with pink testicle. In front of the appearance of the testicle, a detorsion, a left orchidopexy and a contralateral orchidopexy were performed. With a good clinical and radiological evolution.
The seriousness of the torsion of the spermatic cord makes it the first etiology to be evoked when faced with a clinical picture of "large painful acute purse". Its urgent and surgical management is the only guarantee of a favorable prognosis. However, this remains uncertain for the torpidity of the testicle concerned and for the fertility of the individual due to the anomalies observed on the contralateral testicle [3]. Emergency surgical exploration must therefore imperatively remain the rule regardless of the patient's age, after having warned the patient and the parents of the risk of testicular necrosis, which may justify an orchiectomy during the operation. In this case, taking an intraoperative photograph may also be justified to facilitate communication with the family after the operation. The operation must be performed urgently because there is a direct correlation between the functional impact and the duration of ischemia [4]. The left side is most often affected according to the study by MCCOMBE and SCOBIE [5], the Israeli team of BEN-CHAIM [6], blame the length of the cord on the left which is usually longer and therefore more likely to bend. Other authors claim the opposite with predominance in favor of the right side [7]. In our study, we did not find a significant difference between the two sides. Make responsible the length of the cord on the left which is usually longer and therefore more susceptible to twisting. Other authors claim the opposite with predominance in favor of the right side [8]. In our study, we did not find a significant difference between the two sides. Make responsible the length of the cord on the left which is usually longer and therefore more susceptible to twisting. Other authors claim the opposite with predominance in favor of the right side [8]. In our study, we did not find a significant difference between the two sides.
For surgical simplicity we systematically choose a scrotal route through a single incision on the affected scrotum, 12 cases were operated on were operated on by incision on the median raphe, an orchidopexy is systematically performed in the months following the intervention or in the same operative time. It is true that there is a risk in the face of the tumorous testicle. In a series, they had to deplore only one incident. It was an intratumoral hemorrhage manifesting in the form of violent scrotal pain. As soon as the observation was made, they converted the intervention by approaching the vessels to inguinal and performed the orchiectomy. With a follow-up of three years, the patient is currently in complete remission. In our study, all testicles were sent to the pathologist, Depending on whether the torsion occurs below or above the line of reflection of the vaginalis, the torsion is said to be intraor supravaginal. Intravaginal torsion of the spermatic cord is the form most frequently encountered outside the neonatal period [9]; in our study we found a single case of extravaginally torsion in an adolescent with Down syndrome. For DURAND L and PERRIN P [10]. there are 2 types of anatomical anomaly that help to understand the occurrence of TCS in adolescents: - tilting of the testicle facilitating the bringing together of the 3 points which fix it normally - the existence of an inter-epididymis-testicular mesa with disintegration. Epididymis and testis. The right or left hemi-scrotal pain perceived in the cord, the epididymis and the testicle in pain inaugurates the clinical picture of this emergency. This is paroxysmal pain, the type of which is not indicated but most often radiates to the inguinal region. It is associated with scrotal swelling in 79% of cases [11]. Other clinical signs are often encountered such as nausea and vomiting, negative Prehn's sign, horizontal elevation of the testicle, an abolished cremasteric reflex, or nonspecific signs such as fever or symptoms of lower urinary tract, some patients report a history recent scrotal trauma or intense physical activity before the onset of torsion symptoms [12- 17] our study is in agreement with the literature. Of the risk factors identified in the literature, we note: the genetic theory, cases of family torsion are described [18] the torsion of the spermatic cord is most often spontaneous and nocturnal. Some triggering factors are described: sexual intercourse, masturbation, scrotal trauma, sudden movement, cycling [19]. An orchiectomy is performed in the absence of recordation after a minimum of 10 minutes of observation and after failure of the revitalization maneuvers. An anatomopathological examination is always carried out. Testicular torsion in adult’s leads to more orchiectomy than in children and this is due to a large number of turns of the whorl in adults [2]. The testicular salvage rate in the literature is between 90 to 100%, if the exploration is done before 6 a.m., the rate decreases to 50% after more than 12 p.m., then less than 10% after 24 p.m. Orchiectomy rates vary between 39 and 71% in most series [20-22]. Thanks to the use of high-resolution probes, testicular and spermatic cord ultrasound associated with a Doppler testicular vascularization study becomes an efficient examination. In the initial period, the testicular echo structure is not changed, and then the testicle gradually becomes hypoechoic due to testicular edema. After 24 hours, the testicular echo structure is heterogeneous due to the appearance of patches of necrosis [23]. According to various works, the study of testicular perfusion with Doppler has a sensitivity of 76% to 100%. In addition to the study of testicular perfusion, examination of the cord is essential. We look for the twist at the level of the cord (Whirlpool sign). This sign has a sensitivity of 97.3% and a specificity of 99% [24].
Spermatic cord torsion is a surgical emergency, a race against time for the surgeon to try to restore testicular vascularization, avoid damage to the contralateral testicle, preserve fertility and avoid physiological, psychological and social sequels. TCS can occur at any age. In adults, TCS represent approximately 20% of cases. Thus, the TCS must be evoked in front of any large acute bursa whatever the age. The diagnosis is essentially clinical. If the diagnosis is little likely, echo-Doppler occupies a place of choice in helping to make the diagnosis. The most important factor determining testicular preservation is the delay between onset of torsion and surgical management. Rapid suspicion of this diagnosis and emergency surgical management can limit the risk of orchiectomy and secondary testicular atrophy. The orchiectomy rate remains high (49%); this figure is related directly with the delay of surgical exploration which remains late in our context. Improving the surgical exploration time requires raising awareness among the general population, continuing medical education and facilitating access to health facilities.
[CrossRef]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
[CrossRef] [Google Scholar] [Pub med]
Citation: Chakir Y, Berni Y, Moataz A, Dakir M, Debbagh A , Aboutaieb R (2022) Clinical and Therapeutic Study of Torsion of the Spermatic Cord: 91 Cases. Andrology. 11:260.
Received: 18-May-2022, Manuscript No. ANO-22-17538; Editor assigned: 23-May-2022, Pre QC No. ANO-22-17538(PQ); Reviewed: 06-Jun-2022, QC No. ANO-22-17538; Revised: 16-Jun-2022, Manuscript No. ANO-22-17538(R); Accepted: 23-Jun-2022 Published: 23-Jun-2022 , DOI: 10.35248/2167-0250.22.11.260
Copyright: © 2022 Chakir Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO