Journal of Cell Science & Therapy
Open Access
ISSN: 2157-7013
ISSN: 2157-7013
Mini Review - (2021)
Madelung’s Disease (MD) is a rare syndrome characterized by the presence of non-capsulated fatty deposits symmetrically located in the body. Various treatments have been proposed during years, but only surgical treatment seems to be the only disease modifying possibility. Surgical options are lipectomy, first treatment described, and liposuction. Due to the nature of the disease, both techniques are burdened by a high relapse rate, and there is no consensus about which is the best one. Moreover, when surgical excision is performed, un-aesthetical scars can occur, and patients can be not satisfied. Cervicofacial district is one of the most involved body areas by Madelung’s disease, for this reason, aesthetic approaches like Rhytidectomy can help surgeons to reach the best aesthetical result as possible.
Starting from a clinical case treated in our Department, we made a short review of the available literature to identify the more appropriate approach to reach the most satisfying result.
Rhytidectomy; Gynaecoid; Madelung’s disease; Surgical technique
Madelung’s Disease (MD), also known as Launois-Bensaude syndrome, is a rare metabolic syndrome characterized by the presence of fatty deposits like un-capsuled lipomas located symmetrically in the body [1]. Two variants have been identified, characterized on the location of the fat excess [2]. The causes of this pathology have not been precisely identified, but chronic use of alcohol is reported in the personal history of the 90% of patients suffering the MD. It is mostly described in male rather than female with a ratio of 15:1 to 30:1 and affects the middle age (30-70 years) [3]. To date it is still unclear why it is more prevalent in the European and Mediterranean population. MD seems to be associated to other pathological conditions, such as peripherical neuropathy, hepatic disorders (steatosis, alcoholic hepatitis or cirrhosis), arterial hypertension, dyslipidemia, diabetes [4]. MD diagnosis is clinical, whereas CT, MRI and US can be useful to study in the deep the extension and localization of adipose masses, other structures involvement and to optimize the surgical planning [1].
Effective and lasting strategies are still being sought for the treatment of this pathology. In fact, the incidence of relapses is very high, and represents the first cause of dissatisfaction for patients. Due to the absence of the knowledge of the exact pathophysiology, surgery is still considered the treatment of choice. Lipectomy and liposuction are the main techniques performed, especially in severe cases (e.g., severe aesthetic alterations, compression, or displacement of aero-digestive neck structures). However, due to the benign nature of lipomas and the proximity to other structures (vessels or nerves), the target is not radical [2]. In fact, surgery aims to improve the quality of life of patients.
In our work we consider the pathology affecting the middle and lower thirds of face and neck. Considering the recent interest about MD, we conduct a short review of the literature about the surgical approaches to this district. Finally, we present our surgical approach, characterized by liposuction and Rhytidectomy.
Methodology
We conducted a search of the literature published between January 1, 2000, to June 30, 2021, using MEDLINE (PubMed). The database was first searched using the key words “Madelung disease, surgical treatment and head and neck”, in which 413 articles were found. We considered only studies in English and those referring to humans and with abstract, thus reducing the count to 187 papers. The reference lists of all retrieved articles were scanned to identify additional relevant studies.
Only articles with abstract were considered (170 articles). After selection by title and abstract, 26 works were analysed. A quality score was calculated for each article using a check list from the American Society of Plastic Surgeons guideline for therapeutic studies [5]. Each study was appraised by at least two reviewers (MG and CNF), and rating decisions were based on the consensus of the reviewing authors.
In 1846 Sir Benjamin Brodie first described Madelung syndrome [6]. In 1888, Otto Madelung published the first series of 35 patients with “cervical lipomatosis”, and Launois and Bensaude characterized the disease in 1889 [7].
The disease presents an abnormal accumulation of noncapsulated lipomas distributed symmetrically. Lipomas generally involve only the neck and\or the region of parotid glands: “buffalo hump” and the “hamster-like appearance” are typical signs. In most cases, MD remains localized at this level, but sometime involves other regions of the body: upper or lower limbs, thorax, abdomen, or the external genitalia described two types of MD according to the anatomic distribution [8]. In MD type 1, the location is symmetrical and mainly distributed in the neck (Madelung’s collar or “horse collar”), shoulders, supraclavicular fossa, and proximal regions of the upper limbs, sometimes giving to the patient a “pseudo-athletic” appearance. Whereas patients with generalized fatty masses distribution are categorised as type 2. In these cases, the patients have an obese appearance. Donhauser et al. [9] classifies MD into 3 types. Type I: fat deposition involves only the neck (Madelung fatty neck), Type II: neck, shoulders, upper limbs and back are used to be involved (Pseudo-athletic type), Type III hips and pelvic region are involved (Gynaecoid type). Rarely these lipomas transform in malignant tumours [10].
Madelung’s disease treatment is challenging; several medical and surgical options have been proposed by years. Associated with alcohol abuse and various metabolic disorders, the first steps to decrease the progression of MD are the abstinence from alcohol and a balanced diet. Anyway, this strategy does not reduce the size of the fatty masses but can slow their enlargement [11].
Non-surgical treatments, such as ones based on phosphatidylcholine/deoxycholate, β2 agonist (as Salbutamol) or Heparin injected in lipomas have been studied by several groups [12,13]. Moreover, they could create adherences that could complicate any further surgical approaches [14], like liposuction. Non-surgical options should be considered just in slight and mild cases and should be proposed to patients who do not require surgery. Surgery remains the only possible treatment in advanced disease.
In head and neck district, surgery is considered the most effective treatment. Liposuction and lipectomy represent the best options in this field even though there is still a debate on what is the gold standard [2]. Surgery should be proposed to patients with aesthetic or psychological discomfort caused by MD, diminished cervical range of motion or significant aerodigestive tract compression.
According to most of the authors, open excision represents the first treatment considered [15,16]. Historically, open lipectomy is the first technique used. In fact, before the advent of liposuction, open surgical excision was the only form of treatment for aesthetic deformity or relief of laryngotracheal compression [15]. It lets to see better every close structure and its eventual pathological involvement, performing a safer surgery and avoiding iatrogenic injury. Lipectomy allows to remove huger amount of fat than liposuction, performing a more radical surgery and allows a better reduction of the redundant skin. Moreover, in case of masses located sub-platysmal, open surgery allows a direct approach to masses, resulting in a more radical treatment [16]. New scars -with possible pathological scarring-, higher rate of infection, hemorrhage or hematomas are like to be the lipectomy drawbacks [11]. A new approach to lipectomy was given by performing a cervicofacial lifting with the aim to obtain a greater mass reduction associated with scars well tolerated by patients.
Conversely, liposuction is not as invasive as lipectomy [17,18]. It is easier, faster and it can be performed under local anesthesia. It could be proposed to patients who could not undergo a general anesthesia. Due to the operative technique, important structures such as vessels or nerves could not be seen directly, and it is not suitable for nonprimary excisions of fibrotic adipose tissue [19]. For this reason, many authors consider safe the use of this procedure only for suprafascial masses and in the case of the neck, they recommend remaining above the sternocleidomastoid muscles [20]. Another advantage is the reduction of operative and, mostly, post-operative bleeding. Moreover, it allows the benefit of surgical debulking without long skin incisions, scarring and prolonged recovery period. Liposuction maintains intact most of the subcutaneous neurovascular plexus reducing the risk of post-operative oedema, hematoma, or nerve injury [21]. However, for some authors, liposuction is not the first choice because considered too conservative and not radical enough [22]. In particular, the submental area is the most difficult to correct by lipoaspration alone.
As already said, MD can relapse. Recurrence can be caused by an incomplete surgical excision, as sustained by authors who support lipectomy [10], but also by the pathology itself. Pinto, et al. [4] found a tendency towards a higher relapse rate using liposuction techniques when compared to lipectomy (20% vs 14.1%).
Generally, both methods are performed to be palliative and to lower functional and aesthetical complication rate. The excision of nonencapsulated masses can be incomplete both with lipectomy and with liposuction approaches because of the difficulty distinction of the mass limits. In this context, liposuction gives the possibility to repeat the treatment without adding new scars [20].
But how does the facelift fit into the context of the MD surgical treatment? In literature, this approach is not widely described for cases of MD affecting the cervicofacial area [4,10,23,24].
The placement of incisions for surgical treatment of Madelung’s disease is a controversial, but it is a crucial issue. For example, Wong, et al. [16] recommend mid-neck transversal incision, but other authors [4,24] consider it as a disfigurement. Classic aesthetic incision placement is used in primarily non-aesthetic fields. A trade-off between adequate vision, decent access to fat masses, minimal invasiveness and invisible postoperative scarring is necessary for Hundeshagen, et al. [10]. Facelift approaches have been described for operations such as parotidectomy [25], or for open reconstruction of condylar fractures of the mandible [26]. In MD this surgical technique guarantees a good access to fat masses, acceptable scars, and skin reduction. As in aesthetically motivated facelifts, trimming of excess skin and reshaping of natural neck contours and the cervicomental angle can be readily achieved and customized for each individual patient. According to Pinella, et al. [24] wide skin undermining facilitates the fat resection, which is best done with a scalpel rather than by liposuction.
Rhytidectomy can be considered as an evolution of the lipectomy approach but can also be associated with liposuction; this second approach is not completely defined [15], in fact, there is still a debate on when the excess skin removal should be performed: in the same session of the liposuction rather than few weeks later. Liposuction reduces fat volume and renders the dissection and consecutive skin resection easier. This, however, may be associated with a non-negligible risk of skin necrosis or poor healing that can move surgeons to perform the procedure in two stages [19].
As already said, the submental area is the most difficult zone to correct. Facelift approach can help us to reach our target. In particular, we agree with Candia, et al. [15], considering that the Rhytidectomy approach, with a short submental scar (2.5 cm), provides adequate access to superficial fat and obviates the need for anterior “chin strap” incisions. These incisions can be cosmetically disfiguring and can interfere with the skin redraping necessary for a satisfactory cervicomental angle, as demonstrated by Upjál, et al. [27].
We present the case of a 74-years-old woman who was referred to our Plastic Surgery department due to an evident enlargement of the anterior neck. Patient reported that this mass was present since in 2016 and progressively increased its volume in the last two years.
Patient’s anamnesis revealed a >10-year history of alcohol consumption (equivalent to 100 g/day), complicated by a demyelinating sensory-motor polyneuropathy, since 2007, that requires a treatment with gabapentin 900 mg/day. Moreover, she has history of episodes (five in total) of epilepsy from 2002 to 2007 and chronic vascular encephalopathy with a stenosis of carotids of 25%.
At clinical evaluation (Figure 1), a 10 × 8 cm soft, circular, subcutaneous mass was noted in the anterior surface of the neck; it was not fixed to the overlying skin or deep structures. Two other masses (10 × 5 cm), with the same characteristics of the one described above, were present at supraclavicular level.

Figure 1: Pre-operative photos.
Laboratory test was unrevealing even if the lipid profile reported a nonspecific increase of LDH value (397 mU/ml).
Radiological examinations were performed. CT showed a nonencapsulated fat mass, with soft tissue density mainly deposited in the anterior over-platysmal subcutaneous tissue of the neck. MRI exam confirmed the presence of that superficial nonencapsulated mass. No involvement of deep noble aerial, vascular or digestive structures was highlighted.
Considering the poor sub-platysmal location of the mass, liposuction for mass removal and cervicofacial lifting for skin excess were programmed.
Surgical technique: After preoperative planning, the lower third of the face, the anterolateral cervical region and supraclavicular regions were infiltrated with tumescent solution described by Klein [28] and liposuction of the supra-platysma region was made. A little submental incision was made to allow a submental fatty mass lipectomy, as described by Di Candia et al. obtained a good result in terms of fat removal; we proceeded with the removal of skin excess through Rhytidectomy. We considered the possibility of performing a lower third and neck lifting in reason of the residual skin excess and the possibility to produce more aesthetic scars. Despite the conflicting opinions in literature [19], we considered possible to perform the Rhytidectomy at the same time of liposuction because it was not too aggressive to risk a vascular compromise of the tissues. According to the article published by Sadati, et al. [29], a Triple- C SMAS plication was performed to obtain a face and neck-lift, before removing excess skin. Two suction drains were placed and removed after 48 hours and then sutures have been put. Finally, a liposuction of the two supraclavicular masses was carried out until their complete removal and restoration of the ideal profile were obtained. Patient wore a facial brace for the following month.
No surgical intraoperative or postoperative complications have been occurred and no signs of recurrence have been developed after 18 months. Globally, patient was very satisfied from result (Figure 2).
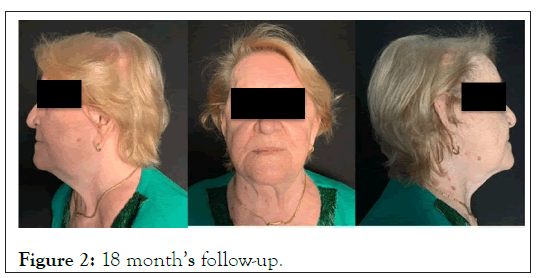
Figure 2: 18 monthâ??s follow-up.
MD represents a rare, indolent and slow-growing disease, but remains an aesthetically very difficult condition to bear. In our experience, liposuction played a primary role in the treatment, leading to optimal mass reduction and fewer risks of complications. Face and neck-lift served both add an aesthetic completion of the MD surgery (removal of the residual skin excess with almost invisible scars) and to favor the lipectomy of the residual masses in areas where liposuction was not sufficient.
MD remains a rare disease, and for this reason data are scarce. With our experience, we strongly believe that this pathology needs a combined surgical approach to reach the best quality in terms of excision of masses, respect of structures and overlying skin and aesthetical result. However, it is necessary, both for us and globally, to treat more cases of MD in order to find a welldefined approach and to get an idea of pros and cons of the various surgical techniques.
Citation: Citation: Miotti G, Negrini FC, Pisano G, Zanin C, Parodi PC (2021) Cervicofacial Lifting for Madelungâ??s Disease: Short Review and Our Surgical Approach. J Cell Sci Therapy. S6: 317.
Received: 17-Sep-2021 Accepted: 01-Oct-2021 Published: 08-Oct-2021 , DOI: 10.35248/2157-7013.21.s6.317
Copyright: © 2021 Miotti G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.