Journal of Cell Science & Therapy
Open Access
ISSN: 2157-7013
ISSN: 2157-7013
Case Report - (2022)Volume 13, Issue 1
The foregut cysts are rare developmental anomalies, which can present a diagnostic and therapeutic challenge. A universal need for resection is debatable especially in asymptomatic cases. The objective of this study is to describe a case of a 26 years old healthy female with two different non communicating mediastinal congenital cyst (bronchogenic and esophageal) in a single mass mimicking a lung abscess with a protracted treatment course and to do up to date literature review to evaluate the decisive factors in the management of bronchogenic cyst.
Congenital foregut cyst; Mediastinal-intrapulmonary bronchogenic cyst; Lung abscess
Bronchogenic and esophageal duplication cysts are rare but clinically distinct and significant developmental anomalies. The respiratory system and esophagus have a common embryologic origin from the primitive foregut tube. Both Esophageal Duplication Cysts (EC) and Bronchogenic Cysts (BC) are congenital malformation due to abnormal budding off the foregut tube and are referred to as foregut cysts. Those that result in respiratory abnormalities are collectively termed as Bronchopulmonary Foregut Malformations (BPFM), which encompass BCs, pulmonary sequestrations, congenital cystic adenomatoid malformation (CCAM) and congenital lobar emphysema [1]. Among these, BCs and ECs together represent approximately half of mediastinal cysts found on imaging [2].
They can be indistinguishable by imaging and share similar diagnostic and therapeutic challenges, thus are often considered together [3-5]. Histologically a BC is lined by ciliated columnar epithelium and its walls contain cartilage plates or bronchial mucous glands, whereas an EC is lined by squamous epithelium and walls contain band of smooth muscle. The gestational timing of abnormal budding dictates the location of a BC, if it occurs during early gestation (before 7 week), the cyst tends to locate centrally along tracheobronchial tree (commonly middle and posterior mediastinum) whereas later budding leads to peripheral locations, including within lung parenchyma, and more often have patent bronchial communication [5,6]. Peripheral lesions (intrapulmonary cyst) with bronchial communication are more likely to present with infection, whereas centrally located lesion (mediastinal cyst) tend to manifest compressive symptoms and are more commonly seen in children. The optimal management or timing of bronchogenic cyst resection has historically been unclear, especially in an asymptomatic cyst. Most of the older series advocate for universal surgical resection to confirm diagnosis and prevention of complications. We present a case with both bronchogenic and esophageal duplication cysts in a single mass mimicking a lung abscess which did not improve with a protracted conservative treatment course and which eventually required surgical resection.
A healthy 26 year old female presented with a day of pleuritic chest pain and fever. Computed Tomography (CT) of chest revealed a well demarcated large cystic mass in the left hemi thorax with an air fluid level (Figure 1).
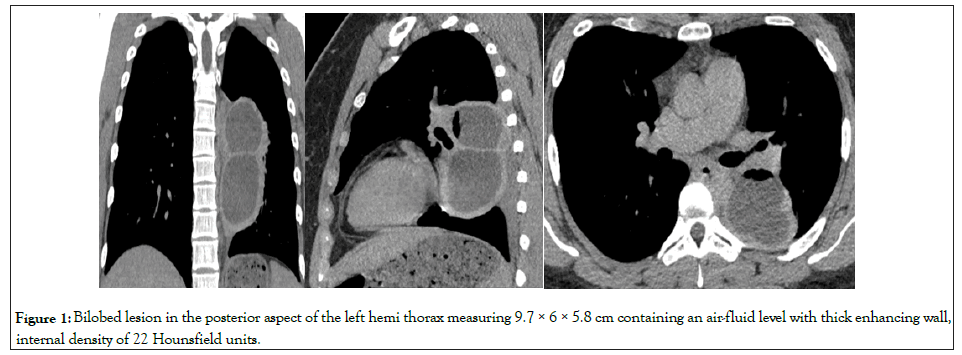
Figure 1: Bilobed lesion in the posterior aspect of the left hemi thorax measuring 9.7 × 6 × 5.8 cm containing an air-fluid level with thick enhancing wall, internal density of 22 Hounsfield units.
She had never had prior chest imaging and was adopted with no available family history. She denied tobacco, alcohol, or substance use, and denied loss of consciousness, vomiting, or aspiration. A working diagnosis of lung abscess was made. CT guided aspiration was performed with drainage of frank purulent material. Fluid cultures and cytology were negatives, Sputum grew mucoid pseudomonas aeruginosa and was treated with four weeks of intravenous cefepime and two weeks of levofloxacin and metronidazole. Pleuritic chest pain persisted despite regression of the lesion over a 10 month period as seen in the serial CTs (Figures 1-3).
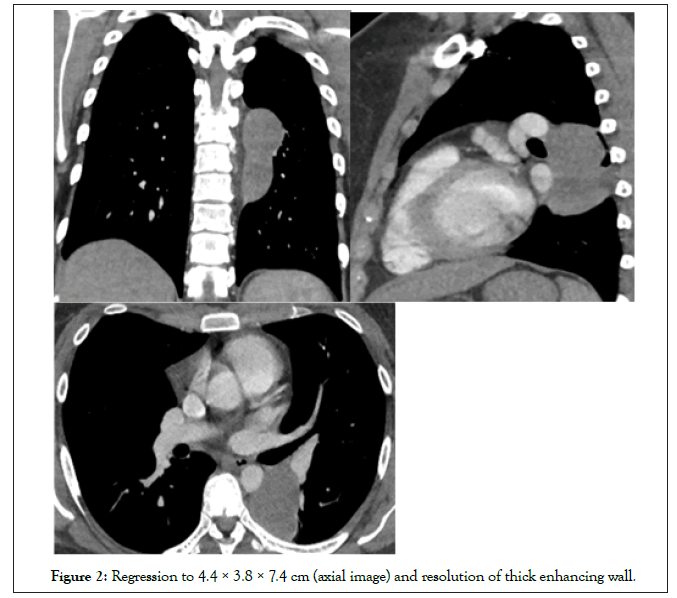
Figure 2: Regression to 4.4 × 3.8 × 7.4 cm (axial image) and resolution of thick enhancing wall.
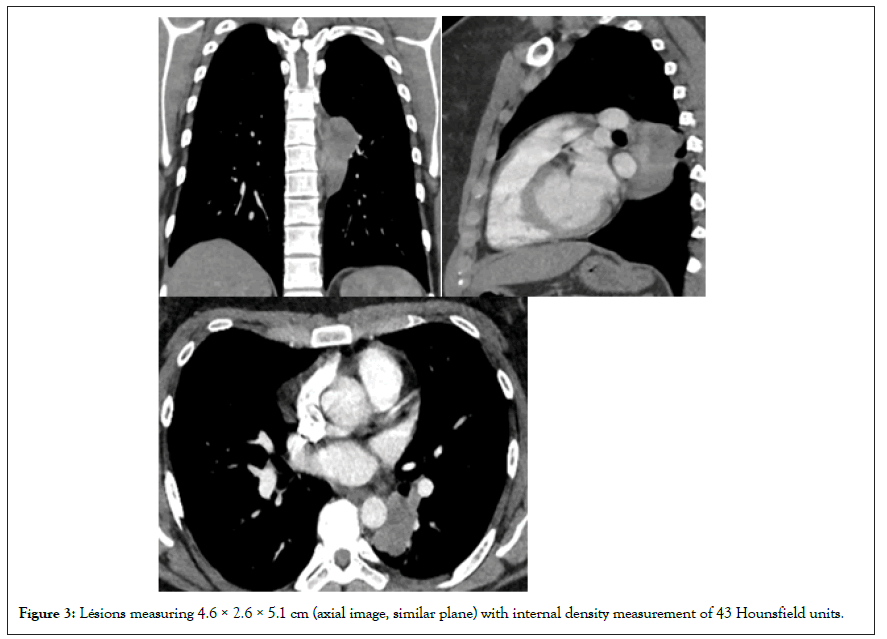
Figure 3: Lésions measuring 4.6 × 2.6 × 5.1 cm (axial image, similar plane) with internal density measurement of 43 Hounsfield units.
The density of the cystic mass, as measured on CT scan, progressively increased from 22 to 43 Hounsfield units over a 10 month period. At 10 months the patient underwent resection through a left video assisted thoracic surgical approach. Intraoperatively, a large inflammatory lesion seen densely adherent to the lung parenchyma with a clear connection point to the esophagus without intraluminal connection and was difficult to resect due to the adhesions. Pathology of the cystic mass showed squamouslined epithelium with thick bands of smooth muscle representing an esophageal duplication cyst (Figure 4A) with an additional no communicating area of ciliated columnar epithelium with cartilage plate representing a bronchogenic cyst (Figure 4B).
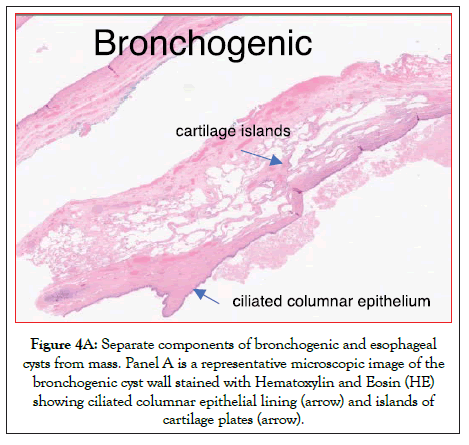
Figure 4A: Separate components of bronchogenic and esophageal cysts from mass. Panel A is a representative microscopic image of the bronchogenic cyst wall stained with Hematoxylin and Eosin (HE) showing ciliated columnar epithelial lining (arrow) and islands of cartilage plates (arrow).
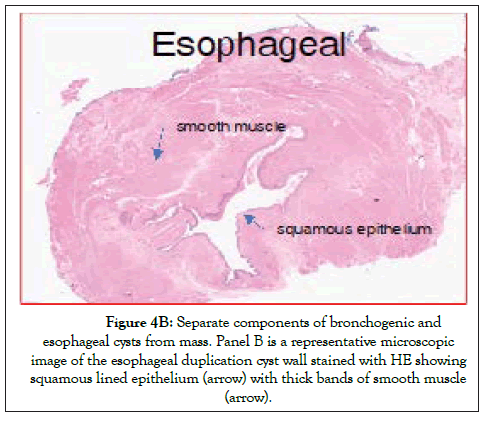
Figure 4B: Separate components of bronchogenic and esophageal cysts from mass. Panel B is a representative microscopic image of the esophageal duplication cyst wall stained with HE showing squamous lined epithelium (arrow) with thick bands of smooth muscle (arrow).
There were no complications in the postoperative period and was discharged home after surgery in a stable condition. At 6 month follow up visit, she was doing well and free of symptoms.
Table 1 included most of the larger series including highly cited studies on mediastinal bronchogenic cyst. It is evidently very clear that most of the series included both adult and pediatric subjects and are vague related to the location of the cyst and their relation with their symptoms and management. This differentiation is important as more symptomatic in pediatric subject and intrapulmonary bronchogenic cyst. Mediastinal bronchogenic cyst is a very heterogeneous disease with unclear natural history. Many cysts remain clinically silent and are discovered in older individuals [2-20].
| Study (year) | N (ped) | Age (Oldest) | BC locations | Symptomatic | CA | Intervention | Peri-opcomplication | |
|---|---|---|---|---|---|---|---|---|
| St-Georges, et al. 1991 [6] | 86 (0) | 36 (69) | 66-M 20-IP |
44/66 (67%)-M 18/20 (90%)-IP |
0 | Mostly thoracotomy | 44% | |
| Suen, et al. 1993 [10] |
42 (NR) | 34.8(62) | 37-M 5-IP |
50% | 1 (in 8 yrs old girl) | Mostly thoracotomy | NR | |
| Patel, et al. 1994 [4] |
18 (0) | 37.6(70) | 14-M 4-IP |
44% | 1 (C) |
Mostly thoracotomy | 27.3% | |
| Ribet, et al. 1995 [5] |
45 (24) | 39 (64) | ALL BC | 63% | 0 | Mostly thoracotomy | 13.4% | |
| Cuypers, et al. 1996 [13] | 20 | 35.6 (70) | 14-M 6-IP |
30% | 1 (SCA) |
Mostly thoracotomy | NR | |
| Aktog, et al. 1996 [14] | 31 (1) | 32 (69) | 11-M 20-IP |
80.6% | 0 | Mostly thoracotomy | 42% (reported as ‘operative difficulties”) | |
| Cioffi, et al. 1998 [3] |
27 (0) | 44 (67) | 15-M 1-IP 11-EC |
56-72% % | 0 | Mostly thoracotomy | NR | |
| McAdams, 2000 [9] | 68 (29) | 22 (72) | 58-M 7-IP 2- diaphragm 1-pleura |
58% | NR | NR | NR | |
| Takeda, et al. [2] 2003 |
95 (10) | 37 (74) | 47 (45%) ? EC-4 (4%) |
39% | 0 | Mostly thoracotomy, | NR | |
| Granato, et al. 2009 [15] |
30 | 45 (65) | 20-M 10-IP |
30% | 1 (LCAC) |
Mostly thoracotomy | 16% | |
| Giacomo, et al. 2009 [16] | 30 (0) | 39 (59) | NR | 37% | 0 | Mostly thoracosopy | NR | |
| Kirmani, et al. 2010 [8] | 683 | ALL BC (Mixed) |
74 asymptomatic initially-> 33/74(45%) symptomatic conversion. | 5 | 20% | |||
| Jung, et al. 2014 [17] | 113 (7) | 41.3 (78) | 11-IP | 23% | 0 | Mostly VATS | 9% | |
| Guo C, et al. 2016 [18] |
99 | 44.5 (79) | 52.5% | 0 | 65.6% VATS | 7.7%-VATS 17.6%-thoracotomy |
||
| Wang, et al. 2018 [19] |
119 (NR) |
45.4 (75) | 119- M | 26.9% | 0 | 99%-VATS | 9.1% | |
| Fievet, et al. 2020 [7] | 82 (32) | ? (77) | 64-M 18-IP |
44%-M 66.6%-IP | NR | 62.5%. | Symptomatic (48%) vs. Asymptomatic group (26%) |
|
| Ceylan, et al. 2021 [20] | 71 | 41 (78) | 45-M 26-IP |
* | 2 (MCA and C) |
22.5%-VATS | 7.2% | |
Note: N- Total number of cases (adult + children), Ped- Pediatrics age, Average age- mean or median (oldest age), NR- Not Reported, BC-Bronchogenic Cyst, M-Mediastinal bronchogenic cyst, IP- Intrapulmonary Bronchogenic cyst, Symptomatic-either initially or subsequent conversion (infection is the most common cause), CA-Cancer, SCA- Squamous Cell Carcinoma, LCAC- Large Cell Anaplastic Carcinoma, MCA- Mucoepidermoid Carcinoma, C- Carcinoid tumor, *- not reported separately for BC, 51.1% symptomatic (altogether among different cysts).
Table 1: Clinical characteristics arranged chronologically by year of publication.
In our review, oldest patient was 79, 18 when diagnosed. Furthermore most of the studies comprises of highly selective surgical case series over extended period of time. Although common indication for resection is for symptom management, all symptoms are not equal. Most common symptoms cough and dyspnea are very nonspecific and should be thoroughly worked up before consideration of surgery. Incidence of malignant transformation of the cyst is exceedingly rare. Kirmani, et al. [8]. Reviewed 23 studies from 1987-2009 with total of 683 adult subjects with bronchogenic cysts. Malignancy was reported in 5/683 (0.7%), out of which 3 subjects had intrapulmonary bronchogenic cyst, 1 subject, who was elderly with smoking history, had possible malignant degeneration with anaplastic neoplasm cell infiltrating the cyst wall, and 1 subject had unconfirmed malignancy. This study also found that 31/74 (42%) of those who were managed conservatively became symptomatic. This composite data, which includes both mediastinal and intrapulmonary bronchogenic cysts, is likely skewed by the inclusion of intrapulmonary cysts, which tend to be more symptomatic [5-12]. This is further reinforced by the fact that the underlying true prevalence of these cysts is unknown, and many may remain undiscovered. In regard to surgical approach,historically, open surgical approach was predominant, and this posed a challenge as the morbidity from procedure itself and the complications thereof raised questions about the benefit and utility of this approach was questionable for all comers. However, with the minimally invasive surgery, there is new emerging data to support early surgical resection via a minimally invasive approach such as the Video Assisted Thoracosopic Surgery (VATS) approach, which has fewer complications than the historical open surgical approach [13-22]. Therefore, current literature advocates early surgical excision with the use of the Video Assisted Thoracosopic Surgery (VATS) as the first line surgical option over open thoracotomy. Multiple surgical centers advocate for early surgical excision as this offers early diagnosis and relief of symptoms with minimal complication rates especially in centers with high volume of VATS procedures.
We conducted a search of the literature published in English language between 1990 and 2021 using Medline (PubMed). Database was searched using the keywords bronchogenic cyst and mediastinal, in which 221 articles found. We considered articles with larger series (n ≥ 18) including mostly adult subjects (age ≥ 19). References from articles reviewed for relevant additional studies to identify highly cited studies (citation ≥ 10). Each study was appraised by two reviewers (HS, ON) and included 17 articles for final analysis extracting prespecified clinical characteristics in the tabular form arranged chronologically by year of publication (Table 1).
There are only a few previous case reports describing coexistence of bronchogenic and esophageal cysts in the same individual. To our Knowledge, this is the first case to report de-novo infected dual cyst in adult. Our case highlights several important points in the management of the cystic lesions in the lung. First, it is prudent to include congenital cysts in differential diagnosis of the mediastinal mass and think beyond usual differential framework of infection, inflammation and neoplasm. Unfortunately the diagnosis is difficult without surgical resection, as characteristic imaging finding are missing in up to half of cases [4-6,8]. Computed tomography (CT) usually shows a well-circumscribed mass of soft tissue (20-40 HU) or water (0-20HU) attenuation. These lesions usually appear cystic but due to increase CT density of the cyst fluid can be misleading to differentiate from a solid tumor. Although seldomly used in the lung, there is a potential role for magnetic resonance imaging, which can better differentiate the cystic nature of these lesions [4,9]. In the study by McAdams, et al. [9], out of 20 patients, who had cyst with soft tissue density on CT, 9 of them had water density on MRI. However PET is usually less helpful. Second, there for aspiration of the cyst both for confirmation of the cystic nature epithelial cells on FNA) depending on its location. The idea of using bronchoscopy (by EBUS guided TBNA) for paratracheal and hilar cysts seems also intuitive, however its efficacy and safety resection [10]. Third, the optimal timing of cyst resection is not clear, especially in an asymptomatic cyst. Most of the older series advocate for universal surgical resection to confirm diagnosis and prevention of complications (infection and malignancy) [6,7,11,12]. However, there is minimal evidence to support this strategy. Unfortunately the overall surgical morbidity associated with resection of these lesions is not trivial, ranging from 20-27% in thoracotomy and 20% in VATS [4,7,11]. In our case, although there were no operative complications, VATS excision was difficult due to surrounding inflammation and density of the adhesions to adjacent structures. Similar findings were observed in most of the larger case series. A recent study by Fievet, et al. [7] showed no major differences in postoperative complications following surgical resection (mostly VATS) between symptomatic and asymptomatic subjects, but intraoperative complications were more common in the symptomatic group (20% vs. 4%, p=0.01).
BC and EC are well described, but rare clinical entities which can present as a diagnostic and therapeutic challenge, and early multidisciplinary discussion can be helpful. It is important to consider the location of the cyst, as intrapulmonary cyst tends to portend complicated clinical course more frequently than mediastinal cyst. Atypical presentations and lack of improvement in the management of other commoner pulmonary lesions despite appropriate therapy should raise concern for underlying congenital abnormalities. There is a lack of prospective data to support universal surgical resection, though symptomatic and infected cysts will continue to need surgical intervention, which have a significant risk of surgical morbidity.
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] (All Version) [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
Citation: Subba H, Nzewunwa OCN, Sears E, Hochheiser G (2022) Bronchogenic Cyst; Observation vs. Universal Surgical Resection: A Case and a Mini Review. J Cell Sci Therapy.13:336.
Received: 03-Jan-2022, Manuscript No. JCEST-21-14751; Editor assigned: 06-Jan-2022, Pre QC No. JCEST-21-14751 (PQ); Reviewed: 17-Jan-2022, QC No. JCEST-21-14751; Revised: 24-Jan-2022, Manuscript No. JCEST-21-14751 (R); Published: 31-Jan-2022 , DOI: 10.35248/2165-7556-21.13.336
Copyright: © 2022 Subba H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.