Medical & Surgical Urology
Open Access
ISSN: 2168-9857
ISSN: 2168-9857
Case Report - (2022)Volume 11, Issue 2
Tuberous Sclerosis Complex (TSC) is a rare autosomal dominant disease characterized by the classical Vogt’s triad– epilepsy, mental retardation and sebaceous adenomas. TSC can have renal manifestations which include Angio Myo Lipomas (AML) and renal epithelial neoplasms. AML associated with TSC has the highest incidence between the second and third decade, and carries the risk of spontaneous retroperitoneal haemorrhage proportional to its size. Wunderlich syndrome is a rare condition characterized by acute onset of spontaneous, non-traumatic renal hemorrhage into the sub capsular and perirenal spaces, usually from a renal angiomyolipoma. Here we report a very rare case of bilateral giant AML in the setting of TSC with Wunderlich syndrome which necessitated surgery and discuss the management.
Tuberous Sclerosis Complex (TSC); Angio Myo Lipomas (AML); Intralesional arteriovenous fistula
31 years old female patient, presented to the outpatient department complaining of a gradually enlarging abdominal mass for the past 5 months associated with bloatedness and vague discomfort over her flanks bilaterally. Further history also revealed that she had learning disability as a child and suffered from generalized tonic-clonic seizures and is on regular antiepileptics (Figure 1).

Figure 1: Multiple papules with malar distribution suggestive of adenoma sebaceum.
Upon examination, she was pink and haemodynamically stable. Multiple papules were seen primarily distributed across the malar region on her face. Her abdomen was grossly distended with bilateral palpable kidneys extending from the infracostal region to the iliac fossa.
Abdominal CT revealed bilateral huge renal masses with multiple lobulated heterogenous enhancing renal lesions, distorting the normal kidney and pelvi-calyceal system. The right kidney measures 6.6 cm x 8.0 cm x 13.8 cm while the left kidney was significantly larger at 10.5 cm x 17.0 cm x 30.2 cm (Figures 2,3).
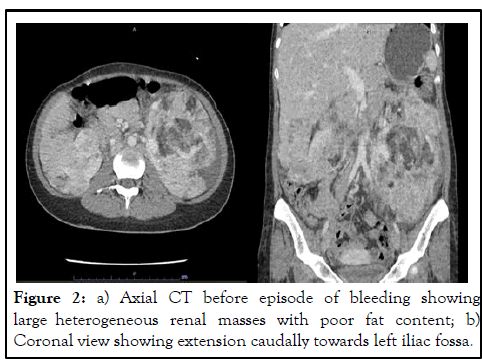
Figure 2: a) Axial CT before episode of bleeding showing large heterogeneous renal masses with poor fat content; b) Coronal view showing extension caudally towards left iliac fossa.
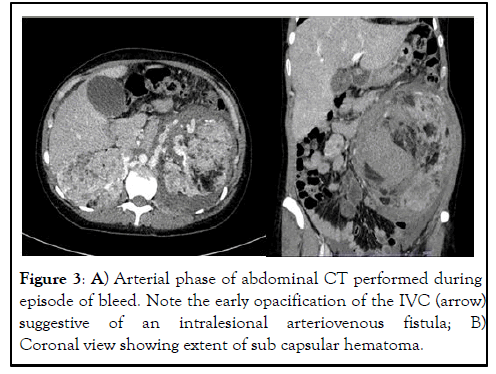
Figure 3: A) Arterial phase of abdominal CT performed during episode of bleed. Note the early opacification of the IVC (arrow) suggestive of an intralesional arteriovenous fistula; B) Coronal view showing extent of sub capsular hematoma.
She was planned for everolimus and was waiting for the government grant approval for such medication. However, she presented again in less than 3 months with the classical Lenk’s triad: worsening left flank pain, palpable flank masses and hypovolaemic shock. She was tachycardic with a heart rate of 112 bpm and hypotensive. She was fluid resuscitated and transfused with packed cells. Emergency abdominal CT showed new hyperdensities on the non-contrasted phase suggesting acute retroperitoneal haematoma surrounding the left kidney. There was also early opacification of the left renal vein suggestive of an arteriovenous fistula in the left kidney with few draining veins. Angioembolization was attempted but failed due to no active blushes on angiography.
Following this event, she was scheduled for a semi-emergency left open simple nephrectomy approached via a left subcostal incision. The resected left kidney weighed 2.5 kg and was 30 cm in size cranio-caudally. Postoperatively she recovered well and was discharged home after 5 days.
Histological studies of the left kidney showed well-demarcated, non-encapsulated tumour involving almost the entire kidney, displaying diphasic morphology composed of an admixture of mature adipocytes, thick-walled poorly organized blood vessels and neoplastic spindled and occasional epithelioid myoid cells. Immunohistochemistry of the tumour cells showed expression of melan-A and SMA, while HMB-45 is focally positive; and negative for cytokeratin, desmin and S 100, consistent with the diagnosis of a large AML of the left kidney (Figure 4).
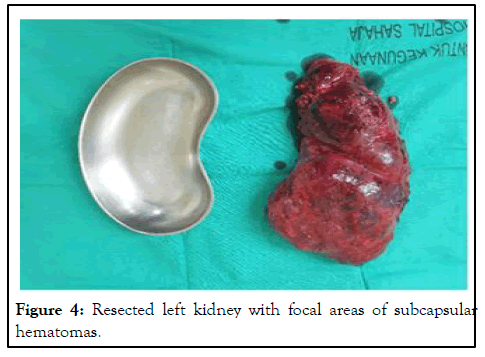
Figure 4: Resected left kidney with focal areas of subcapsular hematomas.
Tuberous Sclerosis Complex (TSC) is an autosomal dominant disease with a prevalence ranging from one in 6000 to one in 12,000. It is caused by mutations in either the TSC1 or TSC2 genes [1], which encode for the proteins hamartin and tuberin respectively. These proteins are tumour growth suppressors and they regulate cell proliferation and differentiation [2]. Hence, their mutations result in formation of various growths and hamartomas in various organs of the body, including renal Angio Myo Lipomas (AML) in up to 80% [3-5] of patients along with other manifestations. The classic triad consists of seizures, mental retardation and angiofibromas but this occurs in less than 40% of the patients with TSC. Unlike sporadic renal AML, TSC related AML tends to be larger, multiple and at a higher risk of bleeding [6]. The main goals of treating patients with renal AML are preserving renal function and minimizing the risk of haemorrhages.
In principle, AMLs should be treated in the setting of: (1) Large tumors; (2) Females of childbearing age, (3) Patients who may find follow-up or emergency care inaccessible and/or (4) Patients with persistent pain/acute bleeding. In our patient, the decision to perform nephrectomy was made because of a recent episode of life-threatening bleed. Otherwise, a diameter of >4 cm is frequently used as a cut-off, owing to the landmark study by Oesterling in 1986 [7]. Management options include surveillance, local ablation, angio-embolization, surgical resection or more recently, medical treatment with mTOR-inhibitors. Conservative treatment should be considered when the patient is asymptomatic with lesions smaller than 4 cm with no risks; following up with imaging every 1-3 years [8]. In the case of tumors >4 cm, 6 monthly follow-ups with ultrasonography is recommended. When active management of the lesion is considered, renal preservation should remain the primary endpoint whenever possible. Selective angio-embolization is the treatment of choice in cases with active haemorrhage, as surgical treatment often results in the loss of a kidney [9,10]. Post-embolization complications include infections, post-embolization syndromes and renal infarction [11,12]. In an elective setting, partial nephrectomy can be considered; with comparable outcomes in terms of complications with standard RCCs [13,14].
As for this patient, we wanted to start her on everolimus. However, everolimus is not readily available in our national formulary and requires special approval from the Ministry of Health before we could start patient on such treatment. Everolimus is an orally bioavailable mTOR inhibitor that induces cell cycle arrest, reduces cell proliferation and prompts angiogenesis regression. It has been shown to reduce the AML volume by 50% after 6 months of treatment [15,16] and is currently approved by the FDA for the treatment of AML in TSC. Unfortunately, this patient presented with significant bleeding requiring blood transfusion before she was started on Everolimus and necessitated the need for nephrectomy.
Within the recent literature, reports of bilateral giant AMLs are rare. In many cases, nephrectomy was almost inevitable [17-19]; but unilateral nephrectomies have been performed with a contralateral nephron-preserving approach [20]. Reported a case in which bilateral nephron-sparing surgery may be performed safely [21] while demonstrated that giant AMLs may be managed expectantly. The various clinical circumstances and modalities available highlight the need for an individualized approach beyond standard guidelines when managing AMLs in TSC.
Bilateral large AMLs in association with TSC are an extremely rare occurrence with few reports of this disease within the contemporary literature. Hence, treatment approaches need to be individualized according to the different clinical scenarios to best preserve the renal function without compromising patient’s safety.
[Croosref]
Citation: Tjun BCJ, Choo GEL, Nasuha NA (2022) Bilateral Giant Renal Angiomyolipoma in Tuberous Sclerosis Complex with Wunderlich Syndrome: A Case Report. Med Surg Urol. 11:285.
Received: 16-May-2022, Manuscript No. MSU-22-17512; Editor assigned: 18-May-2022, Pre QC No. MSU-22-17512(PQ); Reviewed: 01-Jun-2022, QC No. MSU-22-17512; Revised: 15-Jul-2022, Manuscript No. MSU-22-17512(R); Published: 22-Jul-2022 , DOI: DOI: 10.35248/2168-9857.22.11.285
Copyright: © 2022 Tjun BCJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.