Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Research Article - (2020)Volume 9, Issue 2
Introduction: Many men live with chronic prostate diseases, such as Benign Prostatic Hyperplasia (BPH) and Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS). Medications widely prescribed for BPH and CP/ CPPS can cause sexual dysfunction and depression, which may increase patient visits to hospitals. The purpose of this study is to determine whether Thermobalancing Therapy (TT) and Dr. Allen’s Therapeutic Device (DATD) can be used as the first-line treatment preventing the development of new health disorders often resulting from taking medications for BPH and CP/CPPS.
Methods: This is a retrospective analysis of 2 observational clinical trials on thermobalancing therapy and DATD. Cohorts of 124 men with BPH and 45 men with CP/CPPS were treated with DATD and compared to the control groups without DATD. The dynamics of pain, urinary symptoms, Quality of Life (QoL), and Prostate Volume (PV) were assessed before and after treatment.
Results: In men with Benign Prostatic Hyperplasia (BPH), Dr. Allen’s Therapeutic Device (DATD) reduced PV from 45 ml to 31 ml (P<0.001) and decreased urinary symptoms from 14.3 to 4.9 (P<0.001). DATD reduced pain score from 10.3 to 3.5 (P<0.001) in men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS). QoL was improved in both treatment groups. In the control groups, no positive changes were observed.
Conclusions: The use of Thermobalancing therapy as a monotherapy reduces the abnormal prostate size and provides chronic pelvic pain relief in men with BPH and CP/CPPS, improving their QoL. This at-home treatment with DATD reduces the need for long-term courses of BPH and CP/CPPS medications preventing retrograde ejaculation, sexual dysfunction, depression, and other health disorders. The wider use of DATD in healthcare systems will decrease male visits to hospitals, diminishing the risks of contracting a viral infection and transmitting it to others during a coronavirus outbreak or another pandemic.
Benign prostatic hyperplasia; Chronic prostatitis; Thermobalancing therapy; Chronic pelvic pain; Dr. Allen’s device; Medications; Side effects; Alpha-blockers; 5α-reductase inhibitors
TT: Thermobalancing Therapy; DATD: Therapeutic Dr. Allen ’s Device; BPH: Benign Prostatic Hyperplasia; CP/CPPS: Chronic Prostatitis/Chronic Pelvic Pain Syndrome; QoL: Quality of Life; PV: Prostate Volume; LUTS: Lower Urinary Tract Symptoms; I-PPS: International Prostate Symptom Scale; NIH-CPSI: National Institutes of Health Chronic Prostatitis Symptom Index; UrS: Urinary Symptoms; 5-ARIs: 5α-Reductase Inhibitors
Chronic diseases adversely affect the Quality of Life (QoL) of millions of people [1]. The symptoms of a chronic health condition gradually worsen, compelling people to start taking medicines, and the number of medications they take increases over time. By the age of 75, up to 50% of patients are exposed to at least five drugs [2]. The analysis of prescribing patterns has revealed that many patients are on medications with the potential for adverse interaction [3]. The COVID-19 pandemic highlights the importance of medication optimization and deprescribing potentially inappropriate medications, especially in older adults [4].
Many men suffer from Benign Prostatic Hyperplasia (BPH), and Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) places a heavy burden on the health of patients [5]. Management of patients with these chronic prostatic diseases is frequently guided by pharmacological interventions with various medications, mainly including alpha-blockers and 5-alpha reductase inhibitors [6,7]. The use of these drugs can develop serious side events and, therefore they should be administered carefully, especially during a COVID-19 pandemic [8,9].
BPH treatment currently includes medication and surgery [10]. As there is no appropriate therapy for Lower Urinary Tract Symptoms (LUTS) caused by BPH, urologists typically prescribe various combinations of pharmacological treatments [11]. Selfcontrol strategies can be implemented initially, but the debate continues that they can delay drug or surgical therapy, which can lead to negative consequences, especially for men with worsening symptoms [12]. At the same time, medications and surgeries can lead to serious side effects, as a study by Giatti points to the development of severe sexual dysfunction and depression after taking BPH drugs [13].
The treatment guidelines for CP/CPPS recommend the use of the “Five A’s” of CP/CPPS therapy: avoid dietary or physical activities (e.g., bike riding), take long-term courses of antibiotic therapy, alpha-blockers, anti-inflammatories, and 5-alpha reductase inhibitors [14]. However, it is important to remember that all these medications are responsible for severe adverse events, including fatigue, sexual dysfunction, and depression. Discussing post-finasteride syndrome, for example, Dr. Traish says: The medical community must not turn a blind eye to this rare but debilitating condition, especially when it concerns young men [15].
For over 10 years, Thermobalancing Therapy (TT) and Dr. Allen’s Therapeutic Device (DATD) have been successfully used as the at-home treatment for prostate enlargement and chronic pelvic pain [16-18]. The uniqueness of this treatment method for chronic diseases and the innovative design of the wearable therapeutic device, that utilizes the body ’ s own energy, is confirmed with a U.S. patent granted for DATD and TT as "Therapeutic device and method" [19]. The purpose of this study is to assess the pathway of decreasing the instances of sexual dysfunction and depression in men with the use of this Thermobalancing treatment in the management strategies for BPH and CP/CPPS, instead of long-term courses of medications, and to discuss its particular importance during a pandemic.
Study protocol
Two clinical trials were conducted at the Department of Urology at the Yerevan State Medical University. The Ethics Committee approved these clinical studies with TT and DATD (approval No. 1-18.09.2014) and they were registered at the World Health Organisation via the German Clinical Trials Register. DATD has been registered with the Medicines and Healthcare Products Regulatory Agency in the United Kingdom since 2010 as a Class 1 medical device.
Dr. Allen’s Therapeutic Device (DATD)
DATD uses a belt to apply a thermoelement (comprising of a solid mixture of waxes) topically in the projection of the affected organ. This thermoelement is specially designed to accumulate the naturally emitted body heat and to turn into a source of energy itself. Designed as a soft belt, DATD applies the thermoelement to the skin tightly, thereby overcoming the skin barrier and spreading the controlled amount of heat towards the affected prostate gland. The DATD is comfortable to wear on the body. For prostate treatment, the thermoelement is applied to the coccyx area (Figure 1).

Figure 1: DATD for prostate treatment is worn on the body with its thermoelement covering the coccyx area.
Study design
The first clinical trial involved 124 men with BPH who used DATD during a 6-month period. The clinical symptoms and parameters before and after the therapy were examined. The obtained data were compared with the data received from 124 men with BPH who were in watchful waiting. The second clinical trial involved 45 men with CP/CPPS who used DATD during a 6-month period and their clinical data before and after the therapy were examined. The obtained data were compared with the data received from 45 men with CP/CPPS who did not receive TT with DATD. Patients with BPH were assessed using the International Prostate Symptom Score-Quality of Life (IPSS). In men with CP/CPPS, the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) score was utilized. In both clinical studies, Prostate Volume (PV) ml was investigated. The parameters were compared between the groups accordingly.
Participants
During an approximately 3-year period, 45 males (age<55 years) with CP/CPPS (NIH category III) and 124 men with LUTS due to BPH with PV<60 ml were receiving a 6-month at-home treatment with Dr. Allen’s Device and were regularly observed by urologists.
Evaluations
Baseline evaluations were a full physical examination, medical history, digital rectal examination, serum biochemistry, measurement of prostate-specific antigen and electrolytes, urinalysis, and renal function tests. Written informed consent was obtained from all patients before the study. Evaluations were made at baseline and 6 months after treatment. Dynamics of the symptoms and indicators in each group were assessed at the beginning and the end of treatment using NIH-CPSI and IPSS scores. Ultrasound was used to determine the volume of the prostate gland. Evaluation shows that the baseline characteristics of the men were identical in the treatment and control groups in the CP/CPPS and BPH clinical trials (Table 1).
| Baseline characteristics in average of 45 men with chronic prostatitis in the control group and study group measured by NIH-CPSI | ||||||
| Control group | Treatment group | |||||
| Patients No. | Age, years | Pain score | Quality of life | Age, years | Pain score | Quality of life |
| 45/45 | 41.5 | 10.49 | 3.11 | 42.4 | 10.38 | 3.31 |
| Baseline characteristics in average of 124 men with prostate enlargement in the control group and study group measured by I-PPS | ||||||
| Control group | Treatment group | |||||
| Patients No | Age, years | Urinary symptoms | Quality of life | Age, years | Urinary symptoms | Quality of life |
| 124/124 | 65.6 | 13.45 | 3.43 | 65.9 | 14.33 | 3.91 |
Table1: According to the data presented in the table, the baseline characteristics of patients with CP/CPPS and BPH in the treatment group and in the control group were identical.
Statistical analyses
The Wilcoxon signed-rank test was used. P<0.05 was considered significant. Statistical analyses were conducted using SPSS v22 (IBM, Armonk, NY, USA).
In the BPH treatment group, PV decreased from 45.1 ml to 31.8 ml (P<0.001) and UrS score decreased from 14.3 to 4.9 (P<0.001). In the BPH control group, changes were insignificant or even worse. These results suggest that DATD reduces PV and UrS significantly (Figure 2).
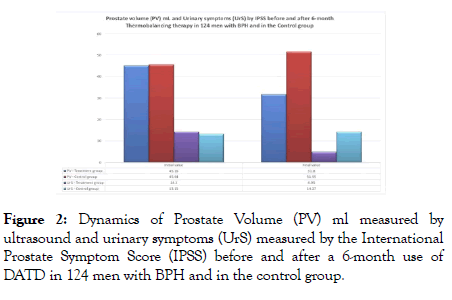
Figure 2: Dynamics of Prostate Volume (PV) ml measured by ultrasound and urinary symptoms (UrS) measured by the International Prostate Symptom Score (IPSS) before and after a 6-month use of DATD in 124 men with BPH and in the control group.
In the CP/CPPS treatment group, there was a significant decrease of PV ml from 31.7 to 27.07 (P<0.001) and the use of DATD reduced pain score from 10.3 to 3.5 (P<0.001). In the CP/CPPS control group, changes were insignificant. The results confirm that TT with DATD decreases PV and pain in men with CP/CPPS (Figure 3).
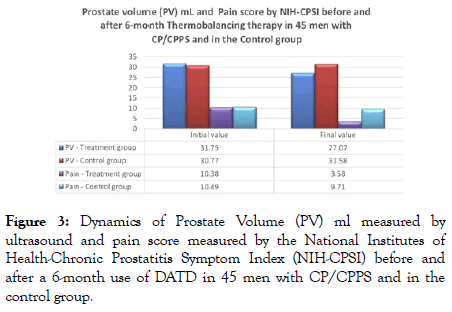
Figure 3: Dynamics of Prostate Volume (PV) ml measured by ultrasound and pain score measured by the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) before and after a 6-month use of DATD in 45 men with CP/CPPS and in the control group.
Side effects
No side effects associated with the use of DATD were observed during both clinical trials.
BPH treatment with TT and DATD reduces the size of the enlarged prostate and, consequently, relieves urinary symptoms (LUTS). TT with DATD reduces the volume of the inflamed prostate and, subsequently, patients with CP/CPPS experience pelvic pain relief. The successful treatment outcomes of these common chronic prostatic diseases suggest the necessity for the use of DATD as the main first-line management tool for men with BPH and CP/CPPS.
At present, however, patients with these common prostatic diseases are typically treated with various unsafe long-term medications with poor effectiveness. Multimorbidity and polypharmacy are common, increasing the risk of adverse events; in older people, it is as high as 78% [20]. Increasing multimorbidity and polypharmacy are associated with a higher risk of developing COVID-19 [21]. Inappropriate prescribing can be a reason for polypharmacy [22], for instance, the overall prevalence of potentially inappropriate prescribing in a retrospective cohort study of 931 people was 42% [23]. At the same time, TT with DATD is an effective treatment modality for the management of BPH and CP/CPPS that can be used at home, reducing the number of patient hospital visits and contact with healthcare providers, minimising the risk of infection and virus transmission during a pandemic [24].
Prevalence of BPH and its drug therapy
A large study involving 8,627 men aged 48-79 years showed that there were 75.3% of men who reported mild form, 22.0% who reported moderate, and 2.7% who reported severe LUTS due to BPH. The prevalence of symptoms increased with age. According to this study more than 97% of men with LUTS can handle the symptoms themselves without taking risky medications and undergoing surgeries [25].
At present, pharmacological therapy is recommended for BPH with a range of drugs, including α1-blockers, 5α-reductase inhibitors (5-ARIs), and combination therapy. These drugs exert their effects via various mechanisms and α1-blockers are associated with adverse reactions, postural hypotension, dizziness, asthenia, abnormal ejaculation, and intraoperative floppy iris syndrome, while 5-ARIs decrease libido, gynecomastia, erectile dysfunction and sexual side effects [26].
Gul and Kaplan suggest that patients with BPH should have a personalized approach to treatment, including patient selection for medical or surgical management that can prevent the failure of medical therapy [27]. This is, therefore, imperative to advise patients with BPH to achieve safe and effective urinary symptoms relief with Thermobalancing therapy in what is called watchful waiting [28]. The use of Dr. Allen’s Device as a selfmanagement tool can help millions of men to safely improve their quality of life and wellbeing [29].
Prevalence of CP/CPPS and its drug therapy
In a large healthy population, the CP/CPPS symptoms affect QoL more detrimentally than even pain [30]. Evidence shows that the overall prevalence of sexual dysfunction among men with CP/CPPS is 62% [31].
A recent Cochrane Systemic review examined the available clinical data on the efficacy of pharmacological interventions for treating CP/CPPS and confirmed that some treatments may confer, at best, only a small and perhaps clinically insignificant benefit for patients. Most common pharmacological agents for CP/CPPS are antibiotics, which may result in sexual dysfunction and reduce QoL, while α-blockers may cause sexual dysfunction, anxiety and depression [32]. Another comprehensive review shows that 5-ARIs have been associated with sexual dysfunction and infertility, as several recent studies have reported adverse sexual and spermatogenic events in young men using 5-ARIs, such as erectile dysfunction, decreased ejaculate volume, decreased libido and infertility [33].
The growing body of evidence showing that medications are mostly ineffective and can exacerbate CP/CPPS by adding side effects suggests that researchers should change their tactics from prescribing pills that do not treat the prostate gland to the use of TT with DATD which improve blood circulation in the inflamed prostate, resulting in notable pain relief and significant improvement in QoL without side effects [34]. Therefore, it is essential to use DATD in personalised care of patients with CP/ CPPS, as TT with DATD allowed to effectively treat this disease at home in 93.4% of men, including a full recovery in 42% of cases [35].
Management strategy for chronic prostatic diseases during a pandemic
The high incidence of these chronic prostate diseases requires a significant response from healthcare services. The use of potentially inappropriate medications is not a rare event, particularly in elderly patients [36]. As medication can cause serious side effects, clinical consideration for BPH drugs is difficult [37]. Although there are many medical options for treating BPH and CP/CPPS, their safety and efficacy are still under assessment [38,39].
A new understanding of the cause of BPH and CP/CPPS that stems from the changes at the vascular level opens a new era in the treatment of these common diseases, which are currently hard to treat. The pathological activity of capillaries results in the development of focal hypothermia inside the affected prostate tissue, thus becoming a continuous trigger developing spontaneous expansion of capillaries and, as a result, swelling and pressure leading, in the long term, to the prostate enlargement [40,41].
It was demonstrated that BPH and CP/CPPS are associated with abnormal blood flow and pressure in the prostate gland. The data obtained by some researchers suggested that prostatic blood flow could be therapeutic targets for BPH/LUTS and CP/CPPS [42-44]. As both these chronic diseases have the same root, their treatment method should be focused on the improvement of blood circulation, which can be achieved with TT and DATD [45,46].
During a pandemic, more health problems arise and should be considered when treating men with chronic prostate diseases. The COVID-19 pandemic showed an unfavourable forecast for aging men, suggesting that 5-alpha reductase inhibitors, which are commonly used to treat BPH, may be one of the factors contributing to the worsening prognosis in men [47]. It is crucial to take comprehensive preventive measures for patients with BPH and CP/CPPS to control COVID-19 transmission via the hospital route. For instance, between March 18, 2020 and April 5, 2020, out of 18 BPH patients who were admitted and treated at a hospital, 10 men (55.5%) became infected with the virus, 2 of them transferred to the intensive care unit and one man died [48].
The use of Dr. Allen's Device as a monotherapy for BPH and CP/CPPS significantly reduces the need for other medical interventions [49]. The at-home treatment with Dr. Allen ’ s Device reduces the number of hospital visits and reduces patient contact with healthcare providers, minimising the risk of virus transmission during a pandemic. It is, therefore, a safe option and can be used by various health care professionals for the management of BPH and CP/CPPS [50].
Limitation
2 observational clinical trials are presented in this study. It might be suggested at a "placebo" or "sham" group as control could have provided more statistical rigor with respect to results. However, most patients with CP/CPPS and BPH have psychological problems including depression and anxiety [51,52]. A 6-month period may be considered an appropriate time for taking placebo tablets but not for using something attached to the body. Therefore, suggesting that patients should wear a "placebo-belt" for 6 months that does not alleviate their symptoms would be very difficult and highly impractical. Typically, patients included in the study experienced notable symptomatic relief several days or weeks after wearing DATD and continued using the device at home as needed
Medications commonly used for BPH and CP/CPPS are linked to serious adverse side effects, such as sexual dysfunction, anxiety, depression, erectile dysfunction, decreased ejaculate volume and libido, and infertility. A new management strategy should implement the side-effects-free Thermobalancing therapy as the first-line treatment for BPH and CP/CPPS. This change can prevent the occurrence of additional health disorders associated with the use of medications for BPH and CP/CPPS. It is particularly important during a pandemic, as the at-home treatment with Dr. Allen ’ s Device reduces the number of hospital visits and reduces patient contact with healthcare providers, minimising the risk of the virus transmission. This strategy and practical approach to the management of BPH and CP/CPPS will significantly improve patients’ health, wellbeing and quality of life.
We are grateful to Professor IG Aghajanyan, the founder of the Armenian Association of Urology, for his support in conducting clinical trials.
Author contribution
SA made a contribution to the concept of the studies. AA made a contribution to the design of the studies. SA and AA analysed and interpreted patient data and wrote the manuscript. SA and AA approved the final manuscript.
Declarations
The authors declare no financial or any other conflict of interest with regard to the publication of this article.
Citation: Allen S, Adjani A (2020) Benign Prostatic Hyperplasia and Chronic Prostatitis Thermobalancing Therapy Can Prevent Sexual Dysfunction and Depression Linked to Medications: Importance During a Pandemic. Andrology 9:207. doi: 10.35248/2167-0250.2020.9.207
Received: 11-Jul-2020 Accepted: 21-Jul-2020 Published: 28-Jul-2020 , DOI: 10.35248/2167-0250.20.9.207
Copyright: © 2020 Allen S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited