
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2020)Volume 10, Issue 4
We describe a case of a 43-year-old female who was found unresponsive after an intentional overdose of bupropion and cyclobenzaprine. Upon transfer to our hospital she began to exhibit signs of Brain Death (BD). Electroencephalogram (EEG) showed burst suppression pattern, which has been documented in bupropion overdoses that mimic BD. We discuss mimics of BD and the need for caution before making this diagnosis when patients clinically present with signs of BD.
Toxicology; Psychiatry; Brain death; Intensive care
A 43-year-old female was transferred to our facility from an outside hospital for acute encephalopathy and possible status epilepticus after an overdose of cyclobenzaprine 150 mg and bupropion 2.7 g. The patient was found in a ditch on the side of the road by police with an unknown downtime. In the ED at the transferring facility she had a GCS of 3 and developed 6-8 seizure-like episodes each lasting 20 seconds necessitating intubation and treatment with IV levetiracetam and lorazepam. CT head was unremarkable. The patient’s mother found empty bottles of bupropion 300 mg (90 pills), cyclobenzaprine 5 mg (30 pills), and aspirin (unknown amount) in the patient’s home. She had QTc prolongation to 533 ms and hypotension with the systolic pressures being in the 70s. The patient was placed on pressor support. A sodium bicarbonate drip was started, possibly as empiric treatment for salicylate ingestion.
On arrival to the ICU around 2:00 a.m., labs revealed pH of 7.38 and bicarbonate 23.8 mmol/L (reference range: 21-31 mmol/L), hypokalemia with potassium of 2.7 mmol/L (reference range: 3.5-5.3 mmol/L), hypocalcemia with serum calcium of 1.73 mmol/L (reference range: 2.13-2.67 mmol/L), mild leukocytosis, and mild normocytic anemia. Urine drug screen was positive for amphetamines and benzodiazepines, but the patient had received benzodiazepines iatrogenically. TSH was within normal limits and salicylate level was negative. EKG demonstrated QRS widening at 156 ms (Figure 1). Poison Control recommended continuing sodium bicarbonate 150 meq in 1000 ml D5W with goal pH of 7.55 in order to establish normalization of the QTc and QRS on EKG. Repletion of electrolytes was initiated. Initial exam was remarkable for fixed 8 mm pupils, no brainstem reflexes, no withdrawal to noxious stimuli, and the patient was not triggering the ventilator. The neurology consultant’s impression was that she had suffered an anoxic brain injury subsequent to her overdose. They recommended an MRI and official BD testing.
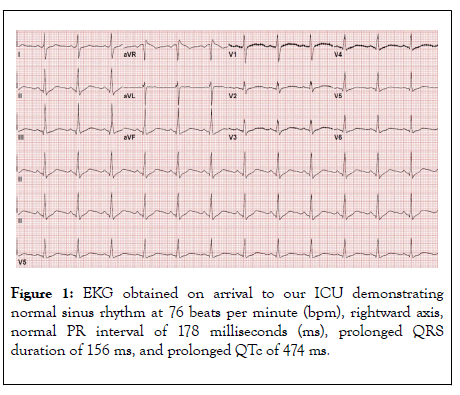
Figure 1: EKG obtained on arrival to our ICU demonstrating normal sinus rhythm at 76 beats per minute (bpm), rightward axis, normal PR interval of 178 milliseconds (ms), prolonged QRS duration of 156 ms, and prolonged QTc of 474 ms.
During rounds on hospital day 0, her physical examination was unchanged, except that she was now breathing over the ventilator. MRI brain was unremarkable. Initial EEG showed burst suppression pattern suggestive of nonspecific encephalopathy (Figure 2).
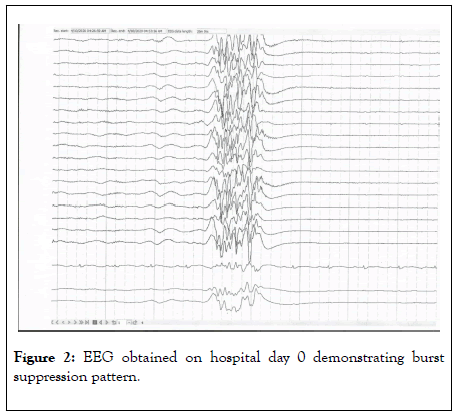
Figure 2: EEG obtained on hospital day 0 demonstrating burst suppression pattern.
Neurology now suggested that we wait 72 hours for full bupropion clearance from the patient ’ s body prior to any further neurologic prognostication. QTc prolongation peaked at 792 ms (Figure 3), which was treated with sodium bicarbonate and magnesium sulfate, and hypotension resolved on day 0. During hospital night 1, she was found to be in myoclonic status epilepticus, which broke with a combination of lorazepam 8 mg IV, levetiracetam 1000 mg IV, and valproic acid 500 mg IV once. Neurology increased daily levetiracetam (which was started at the outside hospital at 1500 mg BID) to 2000 mg BID and added valproate 500 mg BID. Burst suppression pattern persisted on EEG. By hospital day 2 the patient was withdrawing from pain and had reactive pupils. EEG demonstrated spindle coma pattern suggestive of severe metabolic vs. hypoxic encephalopathy on days 2-4. On hospital day 4 her sedation was weaned off and the patient was awake enough to open her eyes, follow commands, and was able to be successfully extubated. EEG at this time showed beta coma pattern again suggestive of severe metabolic vs. hypoxic encephalopathy. The patient’s strength gradually improved with rehabilitation and she was downgraded from the ICU on hospital day 10. On hospital day 20 she was discharged to inpatient psychiatry. She was released to her home neurologically intact less than one month after her initial presentation. Several weeks after discharge the patient reported significant memory issues but was very thankful to be alive. She had no recollection of her overdose.
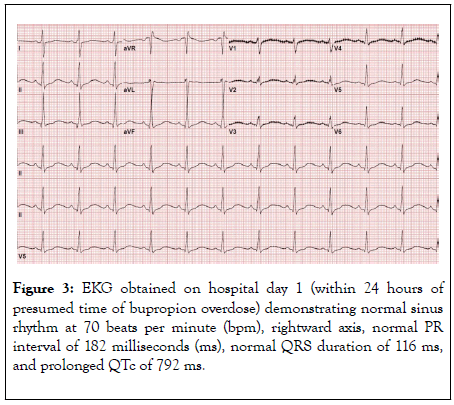
Figure 3: EKG obtained on hospital day 1 (within 24 hours of presumed time of bupropion overdose) demonstrating normal sinus rhythm at 70 beats per minute (bpm), rightward axis, normal PR interval of 182 milliseconds (ms), normal QRS duration of 116 ms, and prolonged QTc of 792 ms.
Bupropion overdoses that have the appearance of BD are extremely rare: only three other cases of bupropion overdoses who presented with the appearance of BD and were discharged from the hospital neurologically intact exist in the literature. One of them manifested signs of neurologic recovery at 36 hours, the other two on hospital day 3 [1-3]. Another of these patients showed movement of his fingers and pupillary light constriction as his body was being prepared for organ harvest [1]. All three patients showed burst suppression on EEG. Another case exists of a 13-year-old girl who presented after a 2.1 g bupropion overdose with signs of BD who subsequently died of ventricular fibrillation cardiac arrest. She too showed burst suppression pattern on EEG [4].
Burst suppression pattern on EEG is characterized by intervals of high voltage alternating with intervals of suppression or neutral electrical activity. The bursts and suppressions can last less than a second to more than 10 seconds. Burst suppression can be seen in deep stages of coma, but patients may exhibit intermittent myoclonic jerks, as did our patient [5]. Burst suppression pattern disappeared from our patient’s EEG by day 3, at which time her physical exam was no longer suggestive of BD. Given that the half-life of bupropion is approximately 20 (± 5) hours, and for its metabolites erythrohydrobupropion and threohydrobupropion 33 (± 10) and 37 (± 17) hours, respectively, Poison Control recommended that we wait at least 72 hours before performing official BD testing for this patient [2]. Waiting this amount of time for neurologic prognostication made it clear that this patient was suffering from a BD mimic, as it had for the previously mentioned bupropion overdose patients.
Overdoses of antiepileptic drugs and baclofen followed by polyneuritis constitute the primary and secondary most common causes of BD mimics [6]. Other cases reported in the literature include organophosphate toxicity, hypothermia, high spinal cord injury, and delayed neuromuscular blockade clearance [7]. For the declaration of BD, the American Academy of Neurology (AAN) requires that a patient be in an irreversible coma without respirations, with normal acid-base status, normal vital signs, and have no CNS depressant on board (and if one is present it is recommended by experts to wait at least five halflives prior to clinical determination of BD) [8]. Most BD mimics previously mentioned would be excluded based on these criteria, unless a history of toxic ingestion were unknown. This emphasizes the importance of obtaining collateral history when patients present with clinical signs of BD, particularly if they are otherwise young and healthy.
In summary, bupropion overdose mimicking BD is a rare entity. Our case highlights how essential it is to seek out additional information from friends or family when patients present with signs of BD, particularly when the circumstances surrounding their clinical state are unclear. There is no rapid serum diagnostic test for bupropion levels, so obtaining a history is key. Had a history of bupropion ingestion not been known, sufficient neurologic prognostication time may not have been provided. Critical care providers should include bupropion overdose on their differential diagnosis for conditions that can mimic BD.
Citation: Pelletier JN, Ie SR, Stromberg PE, Perkins JC (2020) Back from the Dead: A Case of Bupropion Overdose Mimicking Brain Death. J ClinToxicol. 10:447. DOI: 10.35248/2161-0495.20.10.447
Received: 01-Jul-2020 Accepted: 15-Jul-2020 Published: 22-Jul-2020 , DOI: 10.35248/2161-0495.20.10.447
Copyright: © 2020 Pelletier JN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.