Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Case Report - (2023)Volume 13, Issue 1
Antiphospholipid syndrome can cause blood clots to form within the arteries, veins and organs. It can also cause miscarriage and stillbirth in pregnant women.Symptoms may include blood clots, which may occur in the legs, arms or lungs. Recurrent miscarriages may also be common. Blood-thinning medication can reduce the risk of blood clots.
Antiphospholipid syndrome; Blood-thinning medication; Lupus anticoagulant; Anticardiolipin antibodies
Antiphospholipid Syndrome (APS) is an autoimmune disease characterized by the presence of antiphospholipid antibodies: Lupus anticoagulant, anticardiolipin antibodies and anti-β2- glycoprotein 1 antibodies. APS can present with different clinical manifestations, including vein and arteries thromboembolism, as well as obstetrical complications, such as recurrent miscarriage, early delivery, oligohydramnios, prematurity, intrauterine growth restriction, fetal distress, fetal or neonatal thrombosis, pre-eclampsia/eclampsia, HELLP syndrome.
Current treatment to prevent obstetrical complications relies on low-dose aspirin and/or low-molecular-weight heparin.
The authors therefore present the case of a 31 years old primigravida woman, with negative past medical history, which had a diagnosis of IUGR pregnancy at 25 weeks of gestation. The patient was followed up as an outpatient but mostly in hospitalization regimen. When she was at 30+1 weeks of pregnancy, hospitalized in the OB/GYN Pathology Unit ward, she reported vaginal bleeding and after a cardiotocography trace openly abnormal, an emergency C-section was performed. A male baby was delivered, weighting 975 g, who died after a few hours.
The day after the C-section, variant hemoglobin analysis, Kleihauer-Betke test, antiphospholipid antibodies, not previously investigated, were applied for in the patients’ blood tests. The results showed a slight increase of Hb-F (1.6%, laboratory cut-off 1.2%), and LAC positivity, while anticardiolipin antibodies and anti-β2-glycoprotein 1 antibodies were negative [1-5].
The patient is a 31 years old woman, primigravida, with no relevant medical history, blood group and Rh factor: A positive.
The pregnancy was dated at the first trimester screening, and an intermediate risk was estimated for trisomy 21, and a low risk for trisomies 13 and 18. The patient had access to a NIPT test, which resulted negative for any of the chromosomal disorders tested. A second trimester ultrasound screening was performed at 20+5 weeks: No anatomical anomalies were detected, a regular biometry for Biparietal Diameter (BPD), Head Circumference (HC), Abdominal Circumference (AC) were found, but a Femur Length (FL) at 13th centile according to Intergrowth-21 fetal growth standards; an Uterine Artery Doppler Ultrasound Measurement (UtAD) was performed, showing a medium plasticity index>95th centile with left notch.
Since this ultrasound finding, the patient had periodic ultrasound evaluations at the clinic. When she was 25+4 weeks, an ultrasound scan revealed CA<3rd centile, FL<3rd centile; fetal Umbilical Artery Doppler (UAD) Pulsatility Index (PI) was>95th centile with Absent End-Diastolic flow (AED) in almost half of the samplings. Referring to ISUOG Practice Guidelines we determined a diagnosis of early fetal growth restriction. The patient was then hospitalized and monitored daily with clinical examinations, blood tests, cCTGs, and fetal doppler velocimetry 2-3 times/week. We included in the blood tests the evaluation of placental biomarkers, and the sFlt-1/PlGF ratio was in a first measurement 71.4 at 25+5 weeks; in a second measurement it was 103.46, at 27+0 weeks, suggestive for a pre-eclampsia outset in the next four weeks.
Antenatal corticosteroid therapy for fetal lung maturation was given to the patient (two 12-mg doses of betamethasone intramuscularly 24 hours apart). The patient, previously on therapy with low dose aspirin, was then treated with lowmolecular- weight heparin (Enoxaparin, 4000 UI/daily) [6-8].
The patient was hospitalized for 22 days and then she went home to prosecute the check-ups 2-3 times/week since the cCTG traces and the fetal doppler velocimetry were considered stable. After seven days we decided to admit her again to the ward, due to a worsening of the cCTG trace (“NST criteria unsatisfied, short term variability 9.8 ms”). The monitoring was done as in the previous hospitalization. A rescue dose of antenatal betamethasone was administered the day of the admission in the ward.
After two days of monitoring, the patient referred to the ward midwifes that she had vaginal bleeding. A CTG was immediately done and the clinical visual analysis interpreted it as an ACOG 3 trace, frankly abnormal (absent variability, shallow late decelerations). Emergency C-section was performed, at 30+1 weeks of gestation, in the suspect of a placental abruption. A male baby was delivered, weighting 975 g, Apgar 5’: 5; the analysis of umbilical cord blood reported venous pH 7.05, BE -14.1, arterious pH 6.99, BE -14.1, compatible with an acute hypoxia overlapped to a chronic intrauterine hypoxic state. The newborn unfortunately died after a few hours. It is right to report that the same morning a cCTG trace and a fetal doppler velocimetry were performed: the cCTG reported NST criteria unsatisfied, no high variability, short term variability 6.1 ms (similar to the traces of the previous days); fetal doppler velocimetry showed UAD-PI 1.70,>95th centile, end diastolic flow positive, normal a-wave of the ductus venosus observed [9-12].
The day after the C-section we decided to include in the blood tests hemoglobin variant analysis, Kleihauer-Betke test, and APS antibodies. Hemoglobin variant analysis showed a slight increase of Hb-F (1.6%, laboratory cut-off 1.2%); the Kleihauer-Betke test had a negative result; anticardiolipin antibodies and anti-β2- glycoprotein 1 antibodies were negative, but we found positivity for LAC (dRVVT 1.32, dRVVT+PL 1.35).
The acute hypoxia over a chronic hypoxic state was confirmed by the histopathological analysis of the placenta: it was reported a retroplacental hematoma (maximum diameter 5 cm, involving 30% of the basal plate) that supported the clinical suspect of placental abruption; compatible findings of moderate chronic hypoxia, such as low weight of the placenta (177 g) and delayed villous maturation, were also reported.
The patient was followed up according to national and international guidelines for IUGR pregnancy. The clinical conduct was based on the reports given mainly by cCTG traces and fetal Doppler velocimetry, but considering also clinical examination, evaluation of fetal active movements, vital signs of the patient, blood tests. After the negative outcome we decided to take additional blood tests that we would like to discuss. First of all, hemoglobin variant analysis, that showed a slight increase of Hb-F (1.6%, laboratory cut-off 1.2%). This test is included in the first trimester screening blood tests in our country, and it was taken by the patient at the right time with a normal spectrum.
The test is routine in first trimester blood test screening to exclude maternal variants, and it is not generally repeated to evaluate the possibility of a fetomaternal transfusion. We decided to take the test to explore this possibility, and the result is ambiguous since the minimum rise of fetal Hb encountered. The result might be referred to the acute event of placental abruption, but we cannot exclude a chronic process of fetomaternal transfusion.
The performance of Kleihauer-Betke test is not generally done in the clinical practice, also when a fetomaternal hemorrage is suspected. The test is considered to be only recommended for the Rh-negative pregnant patient with major trauma , but some advocate its use in all pregnant trauma patients, and it is reported in literature that has obstetrical implications in the diagnosis and prognosis of preterm labor, fetal demise, and other conditions. In this case, we decided to apply the test and it resulted negative. Considering that the patient is Rh positive, the application of the test is discussed for Rh+ women since it seems to be lacking in precision. Anyway, we decided to use this tool in our investigation to have a wider view on the case, and we would recommend a more frequent application of this test in reason of its low cost and of the obstetrical implications described above.
Coming to the search for APS antibodies, according to the recommendations of the Italian society of clinical pathology and laboratory medicine, the diagnosis of antiphospholipid syndrome relies on at least one of the clinical criteria (venous/ arterious thrombosis, pregnancy complications) and on the positivity of APS antibodies that must be confirmed after 12 weeks [13]. APS antibodies are considered positive when LAC and/or increase of anticardiolipin antibodies (IgG or IgM) and anti-β2-glycoprotein 1 antibodies (IgG or IgM) occur (Figure 1).
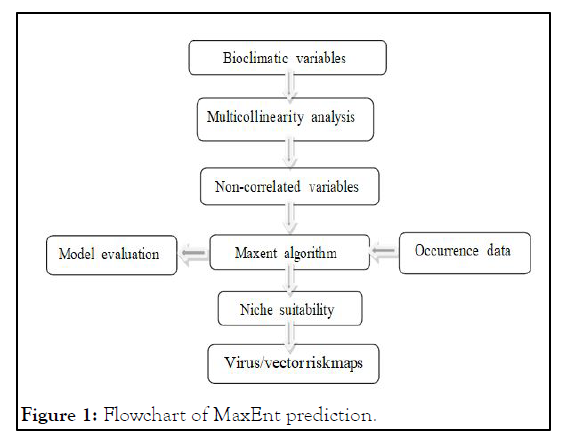
Figure 1: Pathophysiology of antiphospholipid antibodyassociated thrombosis.
In our case we found a positivity for LAC (dRVVT 1.32, dRVVT +PL 1.35), while anticardiolipin antibodies and anti-β2- glycoprotein 1 antibodies resulted negative. If the LAC result will be confirmed after 12 weeks, we will have a diagnosis of antiphospholipid syndrome. APS antibodies must be investigated after obstetric morbidity such as the unexplained death of one or more morphologically normal fetuses at or beyond the 10th week of gestation, and/or one or more premature births of a morphologically normal neonate before the 34th week of gestation, and/or three or more unexplained, consecutive spontaneous abortions before the 10th week of gestation. The clinical criteria for APS do not include intrauterine death, pre-eclampsia, fetal growth restriction that is anyway demonstrated to be associated with APS. To our judgment all these conditions should be investigated as well for APS, and this is why we requested the test for this patient. In our clinical case the patient had been in therapy with low-dose aspirin since the report of alterations in Uterine Artery Doppler Ultrasound Measurement (UtAD), and at the beginning of the first hospitalization we switched to low-molecular-weight heparin, so the therapeutic measures would not have been different with a previous diagnosis of APS; but surely they would have been taken sooner (from the first trimester), and if the diagnosis will be confirmed, this must be considered in the planning of a future pregnancy.
We have presented the case of a 31 years old primigravida woman, with negative past medical history, which had a diagnosis of IUGR pregnancy at 25+4 weeks of gestation, followed-up till 30+1 weeks of gestation when an emergency C-section was performed in the suspect, subsequently confirmed, of placental abruption. In this case report we wanted to discuss the tests that we performed only after the tragic delivery, consisting in hemoglobin variant analysis, Kleihauer-Betke test, and the dosage of APS antibodies. As we illustrated, the hemoglobin variant analysis evidenced a slight rise of fetal Hb. The result might be to be referred to the acute event of placental abruption, but we cannot exclude a chronic process of fetomaternal transfusion.
Concerning the Kleihauer-Betke test, the negative result does not support the theory of a pre-existing fetomaternal transfusion, but it should be evaluated in similar cases to explore this diagnostic possibility, and we recommend its application in virtue of its low cost and of the possible positive result in many pathologic pregnancies.
APS antibodies were investigated regarding to the possibility on APS underlying the clinical picture of IUGR and altered placentation. Even if there is no direct indication to the testing of APS antibodies after a single event in a IUGR pregnancy, and in the waiting of a possible confirmation of the diagnosis in 12 weeks, we give value to the execution of this test since probably it would have not changed the clinical and therapeutically management nor the negative outcome, but it is a precious information first of all in the interest of the patient health status, then it should be considered in the planning of a future pregnancy.
Citation: Battini L, Mazzanti R, Carmignani A, Cattani R, Zandri S, Bottone P (2022) Anti-Phospholipid Syndrome Associated to Intrauterine Growth Restriction: Additional Blood Tests Performed after an Adverse Outcome. Gynecol Obstet. 12:599.
Received: 31-Jul-2022, Manuscript No. GOCR-22-18617; Editor assigned: 02-Aug-2022, Pre QC No. GOCR-22-18617(PQ); Reviewed: 26-Oct-2022, QC No. GOCR-22-18617; Revised: 23-Nov-2022, Manuscript No. GOCR-22-18617(R); Accepted: 24-Jan-2023 Published: 06-Feb-2023 , DOI: 10.35248/2161-0932.22.12.599
Copyright: © 2022 Battini L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.