Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Research Article - (2016) Volume 6, Issue 1
Background: Pediatric trauma patients present unique clinical challenges such as different mechanisms of injury, physiological responses, and indications for operative versus nonoperative management compared to adults. Nonoperative management for blunt abdominal trauma is generally preferred in hemodynamically stable children and its outcomes are generally excellent. However, therapeutic strategy for pseudoaneurysms (PA) after solid organ injury (SOI) is controversial.
Methods: Patients aged ≤ 15 years admitted to our hospital from April 2008 to March 2014 because of blunt abdominal trauma were enrolled in this study. The patients were divided into two groups: those complicated with PA (PA group) or without PA (non-PA group). Result: Among the 294 patients admitted with abdominal injury, 17 were enrolled in this study. No significant differences in patient characteristics, treatment course, or outcomes between the PA (n=4) and non-PA (n=13) groups were detected. All PA cases resolved spontaneously with close observation.
Discussion: All PA cases were treated conservatively without the need for surgical procedures, including transarterial embolization, which is frequently required for adult PA cases after SOI; however, no consensus on transarterial embolization for pediatric cases has been reached, owing to its technical difficulty and potential complications. Our analysis suggested that PA after abdominal SOI can be successfully managed conservatively.
Conclusion: Although the length of hospital stay and the period of restriction from full activity tended to be long, all our pediatric PA cases achieved spontaneous occlusion without any complications. Life-threatening complications such as delayed rupture of PA are rare and thus close observation is one of the best methods for treating hemodynamically stable children with PA caused by blunt abdominal trauma.
Keywords: Pseudoaneurysm, Pediatrics, Abdominal injury, Transarterial embolization
CT: Computed Tomography; ISS: Injury Severity Score; NOM: Nonoperative Management; OIS: Organ Injury Scale; PA: Pseudoaneurysm; SOI: Solid Organ Injury; TAE: Transarterial Embolization; TRISS: Trauma and Injury Severity Score
In comparison to adult trauma patients, pediatric trauma patients present differences in the mechanisms of injury, physiological responses, and indications for operative versus nonoperative management (NOM) [1]. NOM for blunt abdominal trauma is the “gold standard” of care for hemodynamically stable children and its outcomes are generally excellent [1-4]. Prior to 2000, 79% of such patients were treated nonoperatively; however, this percentage has increased considerably to 94% thereafter [5]. Removal of the spleen for major splenic injury at young age results in reduced bacterial phagocytosis and a diminished antigen response, resulting in a high risk of sepsis [6]. Younger children are at an increased risk of overwhelming post-splenectomy infection, which has a morbidity rate 5% and historical mortality rate of 25% [7]. The safety of NOM has been validated in many studies, with only very rare complications such as delayed rupture, abscess formation, pseudoaneurysm (PA) formation, and ruptured PA. However, once these complications have occurred, patients are immediately exposed to potential life-threatening events [8]. The frequency of PA in the solid organ injury (SOI) is reportedly 2%−5% in children [2,9]. In adult cases, transarterial embolization (TAE) is often performed immediately after PA is detected [10]. In children, this therapeutic strategy for PA after SOI is controversial due to the danger of rupture and difficulty of TAE [8,11-13].
We retrospectively reviewed the clinical cases of patients aged ≤15 years treated at our institution who had SOI after blunt abdominal trauma and analyzed the patient characteristics to clarify the necessity of TAE for PA after SOI.
Our hospital, Juntendo University, Urayasu Hospital, includes almost all possible medical facilities, including pediatrics, pediatric surgery, emergency physicians, and other types of specialized surgical support, including cardiovascular surgery, neurosurgery, and orthopedic surgery. Approximately 20,000 patients visit our Emergency Room and 5,000 patients are transported by ambulance to our facility each year. All surgeons and anesthesiologists are available throughout the 24 h each day; therefore, staffs are always available to perform emergency operations, even on pediatric patients. Our Emergency and Critical Care Center is similar to level 1 trauma center in USA.
This is a retrospective study that was conducted at a single facility reviewing its clinical records. Amount all the patients who visited our critical care center and patients aged (≤ 15 years) admitted to our hospital from April 2008 to March 2014 because of blunt abdominal trauma were enrolled in this study. Patients with cardiopulmonary arrest on arrival who underwent laparotomy during their treatment were excluded. Patients with severe head injuries (Glasgow Coma Scale < 8) were also excluded from the analysis because their hospital days included extended intensive care and rehabilitation stages, which allowed for a longer period of time to evaluate the potential effects of blunt abdominal injury. Our strategy for SOI in abdomen is shown in Figure 1. Briefly, hemodynamically unstable pediatric patients were prioritized for laparotomy or TAE, whereas, hemodynamically stable pediatric patients underwent enhanced computed tomography (CT), and in case of no extravasation and vascular injury, conservative closed observation was conducted with repeated enhanced CT to check for PA. TAE was also performed if extravasation was confirmed during initial enhanced CT. Based on Table 1, hemodynamically stable pediatric patients without any findings of extravasation and vascular injury in enhanced CT were suitable candidates for NOM [14]. Pediatric patients undergoing NOM were finally selected for this study. Aquilion 64 (Toshiba Medical Systems Corporation, Tokyo, Japan.) was used for detecting trauma.
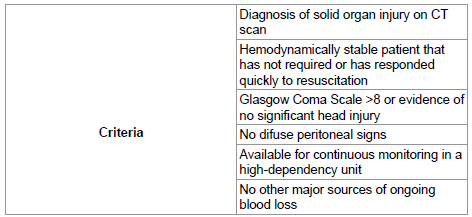
Table 1: Recommended criteria for NOM for children with blunt abdominal trauma.
All patients were evaluated physiologically first and anatomically second and were stabilized according to the Japan Advanced Trauma Evaluation and Care guidelines [15]. All patients were admitted to the critical care center at our hospital for close observation. Normally, patients stay in the intensive care unit for several days depending on the severity of their injury [16]. The SOI management strategy for our critical care center is shown in Figure 1. TAE is performed when a pediatric patient is in shock with extravasation detected using CT. Enhanced CT was performed repeatedly every 5-7 days on pediatric patients with blunt SOI with or without PA to reevaluate the status of their vascular injuries. In general, if no PA is detected, pediatric patients are discharged after their activities of daily living increase, whereas if PA is revealed, pediatric patients rest calmly and are monitored continually, until discharge after PA resolution. The use of TAE for PA in pediatric patients with blunt abdominal injury is controversial. Based on literature (Inoue et al.), the longest duration for observing delayed rupture of PA was 3 weeks after the injury, and spontaneous occlusion was seen in cases of PA with a size below 10 mm [12]. Therefore, in case of confirmed PA on enhanced CT that do not occlude spontaneously until 3 weeks, with confirmed, increase of more than 10 mm in size, TAE was conducted at our department.
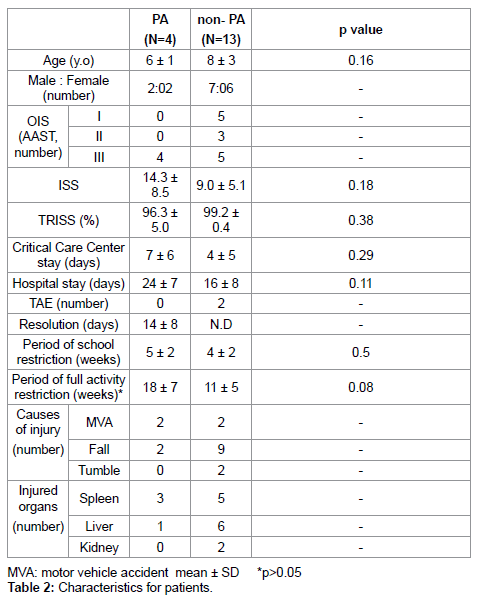
All SOIs were classified using CT images and were graded as described for the American Association for the Surgery of Trauma Organ Injury Scale (OIS) [17]. The patients were divided into 2 groups depending on whether they developed PA (PA group) or did not develop PA (non-PA group). The PA group was further subdivided depending on whether the PA spontaneously resolved during their hospital stay, TAE was performed, or they were switched to operative management. The clinical characteristics of the two groups were evaluated and included age, sex, cause of blunt abdominal injury, and injury severity according to OIS, Injury Severity Score (ISS), and Trauma and Injury Severity Score (TRISS). Therapeutic intervention, clinical complications, and outcomes were compared between groups as primary outcomes. Length of stay in the critical care center, days of hospital stay, interval of school restriction, and interval of full activity restriction were evaluated between the two groups as secondary outcomes.
All the clinical data were reviewed from clinical records and the study protocol was approved (2011-034) by the Institutional Review Board of the Juntendo University (Chiba, Japan). Written informed consent was obtained via the internet website of our hospital or after providing a verbal explanation of the study to each patient or a close relative.
Within the PA group, the number of patients who were switched to TAE from conservative therapy, days of hospital stay, and time to resolution of PA were also retrospectively reviewed from medical records and CT images. The causes of blunt abdominal injury, therapeutic intervention, complication, and outcome were also analyzed.
Data were described as mean ± standard deviation, and values of the two groups were compared by the Mann–Whitney U test using SPSS version 22 for MAC (IBM®, NY, USA). P-values <0.05 were considered to be statistically significant.
Patient selection
Within the observation period, a total 132,406 patients were transported to or visited our Emergency Room, among whom 32,584 patients were aged ≤ 15 years. Among these pediatric patients, 11,600 patients were cases of injury caused by motor vehicle accident, fall, sports, violence or other accidents. 294 patients required hospital admission for intensive care including surgery or close observation. Finally, 17 patients with abdominal injury were enrolled in this study from the 294 injured pediatric patients (Figure 2). There were no deaths among this cohort and all patients were discharged without any subsequent complications.
Clinical characteristics of pediatric abdominal injury
Table 2 presents the clinical characteristics of all 17 pediatric abdominal trauma patients with SOI. Nine male patients and the mean ± standard deviation patient age was 8 ± 3 years. Patients were divided into two groups: PA group (n=4) or non-PA group (n=13), as described above. ISS and TRISS were not significantly different between the groups. Critical care center stay, total hospital stay, time period of school restriction, and time to recover for participation in full contact sports were also not significantly different between the groups.
Spontaneous resolution of PA case
Table 3 shows the clinical course of spontaneous PA resolution as documented with enhanced CT. There was no correlation between the size of the PA, the date that it was detected, or the time periods of school or full contact sports restriction.

Table 3: Literature review on PA management in pediatric cases.
NOM for the blunt abdominal trauma is the most preferred for hemodynamically stable patients, particularly in pediatric patients because its outcomes are generally excellent [1-4]. However, complications such as PA should be treated carefully as they can be potentially life-threatening occurring after blunt abdominal trauma, because the wall of the PA is thin and weak, thus easily causing leak and internal bleeding [18]. The potential for PA development following blunt abdominal trauma must be considered regardless of the cause or severity of the injury [12,13]. It remains controversial whether PA occurring after SOI should be embolized immediately after diagnosed or be observed conservatively.
In the present study, only four of 17 patients developed PA as a complication during their clinical course. All PAs were detected by enhanced CT within 1 week of occurrence. Even when no vessel injury is observed in the solid organ at the initial CT, planned, repeated CT should be performed to detect any subsequent PAs in their early phase. The OIS grade may play a significant role regarding the risk of PA in adult patients; however, no predictive value has been reported for pediatric patients. In addition, the classification of organ injury is not predictive for the occurrence of complications [13,17,19,20], with PA reported to develop even with OIS grade I, including one instance of rupture [21]. Thus, the possibility of PA at injury grade cannot be completely excluded [21,22]. In our study, OIS, ISS, and TRISS, all anatomical or physiological major severity scores, did not reflect PA formation at the initial presentation. Therefore, planned, repeated CT should be performed, even for pediatric patients.
In adult cases, PA is detected in 67% of blunt abdominal trauma patients who failed NOM, and delayed rupture also occurs in 5% of the patients [1,23]. Because of high incidence of PA, TAE is often performed for PA in adults [10,24-27]. TAE offers many advantages compared to surgery, such as precise localization of PA and assessment of collateral flow and easier approach to the injury, particularly in case of intrahepatic PA. In combination, these benefits help reduce patient complication and mortality rates [28]. In hemodynamically stable patients with a non-ruptured PA, occlusion is achieved by embolization in 88%−100% of cases [25,26]. However, there are also some important potential complications associated with TAE.
In pediatric patients, PA after blunt abdominal trauma is rare and therapeutic strategies for treating PA in pediatric cases are still controversial [1,2,13,18,29-31]. There are reported pediatric cases where TAE was performed in the same manner as that for adults [4,8,9,13,17,18,30,32,33]; however, the risks associated with angiography and TAE in children include the difficulty of the procedure, bleeding, PA formation in the femoral artery, abscess formation, PA rupture, intra-abdominal organ infarction, fever, and coil migration [13,29]. The incidence of complications caused by catheterization procedures in younger patient ranges is 0.3%−20% [34]. For patients aged < 3 years, therapeutic intervention and use of a ≥ 6Fr sheath can increase the risk of iatrogenic groin complications, thus necessitating surgical intervention [35]. As we reported previously, spontaneous occlusion of PA in a solid organ can occur, particularly in pediatric cases [2,11,18,23,36,37]. Martin and Inoue et al. have reported literature reviews on PA managed with NOM (Table 3) [11,12]. Martin reviewed 45 patients with PA; nine patients were treated with close observation, and PA resolved in eight patients (90%) without any complications [11]. TAE was performed in 34 patients; however, the PA resolved in only 25 (74%) of these patients and complications occurred in nine patients (26%). Splenectomy was performed on three patients (9%) and splenic infarction occurred in six patients (18%). Splenectomy was performed in two patients initially. Martin reported there was no basis for routinely performing TAE when potential complications were considered. Inoue et al. reviewed 10 patients with PA after SOI and also confirmed spontaneous resolution of PA without TAE [2,12,18,37-39].
Because of the risk of delayed PA rupture is low and almost all of pediatric PA cases after SOI resolved spontaneously without any complications, close observation should be initiated to avoid TAE. Observation should be encouraged as the best method to treat PA after SOI in pediatric patients. Based on previous reports, we observe patients with PA closely for at least 3 weeks in our critical care center and avoid TAE unless the PA increases to a large size with a diameter of >10 mm.
We could manage all our pediatric PA cases without surgical intervention, including TAE, and PA resolved spontaneously. The apparent healing of splenic PA in pediatrics and the success of spontaneous occlusion is attributed to children’s thicker, more fibrous splenic capsule and denser, more elastic parenchyma [2,8]. The mechanism of spontaneous occlusion of PA in solid organs has been attributed to self-tamponade with formation of thrombus [2,23]. With this conservative strategy, parent and patient education is necessary to explain appropriate activities of daily living, including bed rest, sitting, standing, walking during their hospital stay, and return to school life, physical exercise, and contact sports. However, there are currently no specific guidelines for cases of pediatric SOI and timing of their return to normal daily activities, including ordinal school life and social activities.
The American Pediatric Surgical Association guidelines define the length of hospital stay and restriction period of full contact sports [16]. With our cases, the length of hospital stay and restriction period for full contact sports was longer than that presented in the guidelines. Because there are no guidelines for cases of PA, patients rested in bed until the PA had resolved. The restriction period for full contact sports was longer, however, no life-threatening events occurred with the patients in our study. It is difficult to predict the occurrence of PA, however PA can be treated with close observation without the occurrence of a lifethreatening event.
We clearly showed that PA after SOI could be managed conservatively and had the possibility to resolve spontaneously without TAE. This strategy for abdominal injury could avoid the complications for TAE. However, our retrospective study had some limitations, including small number of patients and the lack of data on long-term prognosis of pediatric patients. A large-scale prospective study or multicenter trial on pediatric SOI, including PA management with or without TAE, is required.
We analyzed the characteristics, treatment, and outcomes for pediatric patients with blunt abdominal trauma treated at our critical care center. PA after SOI was detected in four of 17 pediatric patients. All patients were successfully managed conservatively, with spontaneous resolution of the occlusion while avoiding TAE. Although the length of hospital stays and the period of restriction from full activity were longer, all of our patients achieved spontaneous PA resolution without any complications. Lifethreatening complications such as delayed rupture of PA are exceedingly rare such that close observation is one of the best methods to treat hemodynamically stable children with PA caused by blunt abdominal trauma.
The authors declare that no conflicts of interest are associated with this manuscript.