Endocrinology & Metabolic Syndrome
Open Access
ISSN: 2161-1017
ISSN: 2161-1017
Research Article - (2025)Volume 14, Issue 1
The efficacy of acupuncture in treating Polycystic Ovary Syndrome (PCOS) has been a subject of debate, primarily due to the limitations of previous studies such as small sample sizes, ethnic disparities and an absence of in-depth exploration into the mechanisms at play. This comprehensive meta-analysis aims to synthesize the available evidence and deliver a definitive and unambiguous conclusion. Our search, which extended to July 2024, encompassed international scientific databases including PubMed, Web of Science, Embase and Scopus. We included all meta-analyses that investigated acupuncture as a treatment modality for PCOS. The pooled results were derived using both fixed and random effects models, contingent upon the heterogeneity observed. Heterogeneity was assessed using the I2 statistic and the Cochrane Q test. The quality of the included meta-analyses was meticulously evaluated using the Assessment of Multiple Systematic Reviews 2 (AMSTAR 2) tool. Our review included a total of 10 studies, encompassing 34,946 patients. The findings suggest that acupuncture is significantly associated with an elevated pregnancy rate (Relative Risk (RR): 1.50, 95% Confidence Interval (CI): 1.40-1.61) and ovulation rate (Mean Difference (MD): 1.62, 95% CI: 1.09-2.16). Furthermore, acupuncture has been shown to substantially decrease insulin resistance, as measured by the Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) (MD: -0.35, 95% CI: -0.43 to -0.26), serum testosterone levels (MD: -0.15, 95% CI: -0.19 to -0.11), Luteinizing Hormone (LH) levels (MD: -1.60, 95% CI: -1.90 to -1.31), fasting insulin levels (MD: -2.29, 95% CI: -2.47 to -2.12), miscarriage rate (RR: 0.76, 95% CI: 0.58 to 0.99) and Body Mass Index (BMI) (MD: -1.28, 95% CI: -1.46 to -1.10). Sensitivity analysis substantiated the robustness of these findings. Acupuncture's impact on metabolic indicators is noteworthy; it significantly reduced insulin resistance (HOMA-IR: MD: -0.35, 95% CI: -0.43 to -0.26), testosterone levels (MD: -0.15, 95% CI: -0.19 to -0.11), LH levels (MD: -1.60, 95% CI: -1.90 to -1.31) and fasting insulin levels (MD: -2.29, 95% CI: -2.47 to -2.12). The treatment also had a pronounced effect on reducing the miscarriage rate (RR: 0.76, 95% CI: 0.58 to 0.99), BMI (MD: -1.28, 95% CI: -1.46 to -1.10) and waist-hip ratio (MD: -0.03, 95% CI: -0.03 to 0.02). The improvements in menstrual frequency (MD: -0.41, 95% CI: -0.63 to -0.19) and menstrual cycle regularity (RR: 1.22, 95% CI: 1.17 to 1.26) further underscore the positive influence of acupuncture on the endocrine milieu of PCOS patients. Although the reduction in adverse events did not achieve statistical significance (RR: 0.95, 95% CI: 0.85 to 1.07), this observation is still of interest. The significant decrease in Fasting Blood Glucose (FBG) (MD: -0.36, 95% CI: -0.55 to -0.17) adds to the evidence base for acupuncture's role in ameliorating metabolic dysregulations in PCOS. This meta-analysis, with its rigorous methodology and broad scope, provides compelling evidence supporting the therapeutic benefits of acupuncture for PCOS, offering a valuable addition to the current treatment options.
Acupuncture; Polycystic Ovary Syndrome (PCOS); Meta-analysis of meta-analyses; Reproductive health; Complementary medicine
Polycystic Ovary Syndrome (PCOS) is a complex and heterogeneous disease, also the most common endocrine disorder among women of reproductive age affecting an estimated 11%-13% of women globally. Its main features are hyperandrogenism and oligomenorrhea, which can lead to serious complications such as type 2 diabetes, premature atherosclerosis, infertility and endometrial cancer. The treatment of PCOS should be comprehensive. Although conventional treatments (oral combined hormonal contraceptives, metformin) have achieved good results, their safety and the possibility of long-term use are concerning. With the advancement of research, an increasing body of evidence suggests that acupuncture, as a treatment or part of a combined treatment, has achieved significant effects in treating PCOS [1].
Acupuncture has been used as a medical treatment in China for thousands of years. It can improve insulin sensitivity and reduce testosterone in patients and animals with PCOS. Studies have shown that acupuncture may regulate hormone levels by modulating the Hypothalamic-Pituitary-Ovarian (HPO) axis or by adjusting the levels of Anti-Mullerian Hormone (AMH) and cytochrome P450 aromatase and may also improve insulin resistance by upregulating the Insulin Receptor Substrate 1 (IRS-1)/PI3 K/Glucose Transporter 4 (GLUT4) pathway or by inhibiting the PI3K/AKT pathway. Additionally, acupuncture can improve the mood of PCOS patients. However, due to the lack of a theoretical and scientific research system in traditional Chinese medicine, this ancient and traditional therapy lacks affirmation in modern medicine. The latest surveys have found that acupuncture therapy is not fully utilized and there is insufficient clinical evidence supporting the efficacy of acupuncture in treating PCOS in women, with unclear mechanisms, leading to ongoing controversy.
The current meta-analysis of meta-analyses aims to synthesize the meta-analyses of acupuncture treatment for PCOS, carefully analyze the safety and efficacy of acupuncture treatment for PCOS, to gain a deeper understanding of the subject and resolve disputes and strive to draw more attention to the treatment of PCOS with acupuncture.
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The protocol of this study has been registered on PROSPERO (Registration number: CRD42024574835).
Search strategy
We searched the PubMed, Web of Science, Embase and Scopus databases to identify meta-analyses related to the treatment of PCOS with acupuncture. The search was extended up to July 31, 2024. The search employed a combination of MeSH terms and free text terms: Ovary syndrome, Polycystic (MeSH terms) or (PCOS(title/abstract)) or (syndrome, polycystic ovary (title/ abstract)) or (polycystic ovarian syndrome(title/abstract)) or (ovarian syndrome, polycystic (title/abstract)) and (acupuncture (MeSH terms)) and (meta-analysis (publication type)) or (metaanalysis (title/abstract)) OR (meta (title/abstract)).
Inclusion and exclusion criteria
Inclusion criteria: 1) Study types are meta-analyses evaluating the treatment of PCOS with acupuncture; 2) Study subjects are patients with a confirmed diagnosis of PCOS; 3) Intervention measures involve the intervention group receiving acupuncture treatment and the control group receiving routine treatment, placebo or sham acupuncture; 4) Outcome indicators. The primary outcomes are pregnancy rate and ovulation rate and secondary outcomes include HOMA-IR, testosterone levels, LH levels, fasting insulin levels, miscarriage rate, BMI, menstrual cycle, waist-hip ratio, adverse events, menstrual frequency and Fasting Blood Glucose (FBG) [2].
Exclusion criteria: All studies that are not "meta-analyses" and non-English literature are excluded.
Assessment of methodological quality and grading of evidence
To assess the reliability and quality of the included metaanalyses, two independent researchers (RTW and YHW) used the Assessment of Multiple Systematic Reviews 2 (AMSTAR 2) questionnaire. It consists of 16 scoring items that should be answered with "yes," "partially," "no," or "not applicable to metaanalysis." The AMSTAR 2 checklist has four quality levels: "very low quality," "low quality," "moderate quality," and "high quality."
Study selection and data extraction
According to the inclusion criteria, preliminary screening (i.e., screening of titles and abstracts) was conducted by two reviewers (RTW and YZZ). Full texts of potentially eligible articles were obtained and the final eligibility of each reference was independently assessed by two reviewers (RTW, YZZ). Any disagreements were resolved by discussion with a third reviewer (XCL). The following data were extracted from the eligible articles: Publication year, sample size, study location and acupuncture treatment duration, Standardized Mean Difference (SMD), Odds Ratio (OR) and Relative Risk (RR), as well as CIs for related symptoms. Due to the small sample size, to make the data more precise, the OR values were equated to RR values and data analysis was performed using RR and MD.
Statistical analysis
All statistical analyses were conducted using STATA version 16.0 (STATA Corporation, College Station, TX, US). A randomeffects model was used when heterogeneity was greater than 50%, which is based on the assumption of heterogeneity among studies and their different effect sizes. The confidence interval was 95% CI. Heterogeneity was assessed using the standard I2 test and sensitivity analysis was performed to evaluate the robustness of the study results [3].
Study selection
Figure 1 illustrates the systematic review workflow. The initial database search yielded a total of 70 studies from PubMed (n=10), Web of Science (n=22), Embase (n=6) and Scopus (n=32), of which 22 studies were duplicates. After screening the titles and abstracts of the remaining 48 articles, full-text assessments were conducted on 21 articles and 12 articles met the inclusion criteria for qualitative synthesis. For the purpose of quantitative synthesis, a total of 10 studies were included.
Study characteristics
The carefully selected 10 studies included a total of 34,946 female participants. The eligible studies were conducted between 2016 and 2023. These investigations took place in three countries: China (8), Australia (1) and South Korea (1). All included randomized controlled trials used acupuncture in combination with herbal medicine or traditional treatments or not as the experimental group treatment for PCOS. Table 1 displays the characteristics of the included meta-analyses (Figure 1).
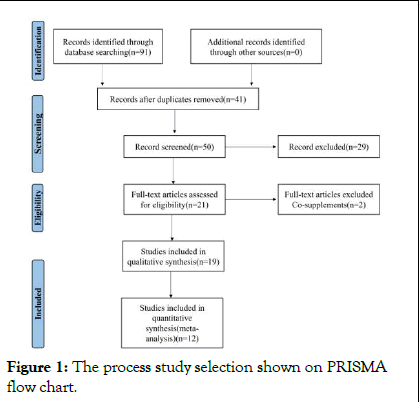
Figure 1: The process study selection shown on PRISMA flow chart.
| Study, year, country | Study number | Therapy | Period of treatment | Outcome | Quality |
| Chen X, 2022, China | 1 | 1. Acupuncture+Metformin | 3 months 6 months |
Pregnancy rate Ovulation rate HOMA-IR |
Yes (Allocation; selective) No (Random; blinding; incomplete) Low |
| Jo J, 2017, Korea | 10 | 1. Electro-acupuncture 2. Manual acupuncture 3. Manual acupuncture+Metformin 4. Electro-acupuncture+Clomiphene citrate 5. Manual acupuncture+ Clomiphene citrate 6. Manual acupuncture +Metformin+Clomiphene citrate 7-Manual acupuncture +Chinese herbal medicine+metformin+ Diane-35 8. Manual acupuncture +Chinese herbal medicine 9. Manual acupuncture +Metformin+Diane-35 10. Manual acupuncture+ Clomiphene citrate+ Chinese herbal medicine |
2 months 3 months 4 months 6 months |
Ovulation rate Menstruation rate LH levels Testosterone levels Fasting insulin levels Pregnancy rate |
Yes (Random; incomplete) No (Blinding; selective; allocation) Low |
| Li PS, 2022, China | 5 | 1. Manual acupuncture + Needle warming moxibustion 2. Manual acupuncture +Suspended moxibustion 3. Electroacupuncture +Needle warming moxibustion 4. Electro-acupuncture + Ginger-separated moxibustion 5- Manual acupuncture +Moxibustion box |
3 months 6 months 3 cycles 6 cycles |
Pregnancy rate Ovulation rate HOMA-IR Miscarriage rate LH levels Testosterone levels Fasting insulin levels BMI |
Yes (Random; incomplete selective) No (Blinding; allocation) Moderate |
| Liang X, Y Main, 2023, China | 13 | 1. Chinese herbal medicine+Acupuncture 2. Chinese herbal medicine+Acupuncture +Diane-35+Metformin 3. Chinese herbal medicine+Acupuncture +Letrozole 4. Chinese herbal medicine+Acupuncture +Diane-35 +Clomiphene 5- Chinese herbal medicine + Acupuncture + Clomiphene 6. Chinese herbal medicine+Acupuncture +Letrozole+HCG 7. Chinese herbal medicine+Acupuncture +Marvelon+Letrozole +HCG 8. Chinese herbal medicine+Acupuncture +Metformin 9. Chinese herbal medicine+ Acupuncture+ Letrozole+Metformin 10. Chinese herbal medicine+ Acupuncture+Diane-35 +Letrozole 11. Chinese herbal medicine+ Acupuncture+Diane-35 12. Chinese herbal medicine+ Acupuncture+HCG 13. Chinese herbal medicine+ Acupuncture+Diane-35 |
3 months 6 months |
Ovulation rate Menstruation rate LH levels Testosterone levels Fasting insulin levels Pregnancy rate Waist-hip-ratio Testosterone levels |
Yes (Random; incomplete; selective) No (Blinding; allocation) Moderate |
| Lim CE, 2016, Australia | 2 | 1. Acupuncture 2. Low-frequency electroacupuncture, physical exercise |
3 months 7 months 12 weeks |
Multiple pregnancy Ovulation rate Pregnancy rate | Yes (Allocation; random; selective) No (Blinding; incomplete) Moderate |
| Liu Y, 2023, China | 6 | 1. Electro-acupuncture 2. Acupuncture+ Metformin 3. Eectro-acupuncture +Metformin 4. Electro-acupuncture +Placebo 5. Acupuncture 6. Acupuncture+ Clomiphene citrate |
2 months 3 months 4 months 6 months |
HOMA-IR BMI Adverse events Fasting blood glucose Fasting insulin level |
Yes (Random; selective; incomplete) No (Allocation; blinding) Moderate |
| Qu F, 2016, China | 5 | 1. Acupuncture+ Chinese medicinal herbs 2. Electro-acupuncture 3. Acupuncture+ Ethinylestradiol and cyproterone acetate tablets 4. Acupuncture+ Gonadotropin 5. Acupuncture+ Metformin |
NR | Menstrual cycles BMI LH levels |
Yes (Allocation; random; incomplete; selective) No (Blinding) Moderate |
| Wu JL, 2020, China | 7 | 1. Electro-acupuncture 2. Manual acupuncture +Electro-acupuncture 3. Abdominal acupuncture 4. Electro-acupuncture +Clomiphene citrate 5. Manual acupuncture +Clomiphene citrate 6. Manual acupuncture +Chinese medcine 7. Electro-acupuncture + Diane-35+Letrozole +Chinese medicine |
3 months 6 months 16 months 3 cycles |
LH levels Ovulation rate Pregnancy rate Menstrual frequency | Yes (Random; selective; incomplete) No (Allocation; blinding) Moderate |
| Yang LJ, 2023, China | 3 | 1. Acupuncture + Moxibustion 2. Clomiphene combined+ Acupuncture+ Moxibustion 3. Acupuncture+ Clomiphene combined |
NR | Ovulation rate Pregnancy rate | Yes (Selective) No (Allocation; random; blinding; incomplete) Low |
| Zheng RQ, 2021 | 1 | 1. Acupuncture | 3 months 6 months |
BMI Waist-to-hip ratio Fasting plasma glucose Testosterone levels |
Yes (Selective; random; blinding; incomplete) No (Allocation) High |
Table 1: Characteristics of the meta-analysis investigating the impact of inositol supplementation on gestational diabetes.
Meta-analysis of meta-analysis results
Pregnancy rate: There are six publications with a total of 10 studies on the pregnancy rate. Among these 10 studies, six studies involve acupuncture combined with conventional treatment (Acupuncture plus metformin vs. metformin [1]; Acupuncture plus herbal medicine vs. conventional treatment; Acupuncture plus herbal medicine plus conventional treatment vs. conventional treatment; Acupuncture plus clomiphene vs. clomiphene; Acupuncture plus metformin vs. metformin; Acupuncture plus medication vs. metformin); two studies have the experimental group with acupuncture and the control group with sham acupuncture (Acupuncture vs. sham acupuncture; Acupuncture vs. sham acupuncture); one study is on acupuncture combined with moxibustion treatment (Acupuncture combined with moxibustion vs. conventional treatment); one study is on acupuncture vs. metformin [4].
Among them, five publications with a total of six studies use the RR (Relative Risk) statistical measure and one publication with a total of four studies uses the MD (Mean Difference) statistical measure. A fixed-effects model was used. The results show that acupuncture treatment has a significant effect on improving the occurrence of pregnancy rates (RR: 1.50; 95% CI: 1.40, 1.61; I2=82.1%, p-heterogeneity<0.001; Figure 2A), (MD: 1.62; 95% CI: 1.09, 2.16; I2=0.0%, p-heterogeneity=0.494; Figure 2B). Sensitivity analysis on studies using the RR statistical measure found no heterogeneity among the six studies (Figure 3A).
Ovulation rate: Six pieces of literature encompassing seven studies on the ovulation rate were identified. Among these seven studies, four studies involved acupuncture combined with conventional treatment or moxibustion (Acupuncture plus metformin vs. metformin; Acupuncture combined with moxibustion vs. conventional treatment; Acupuncture combined with medication vs. medication; Acupuncture plus clomiphene vs. clomiphene); three studies had acupuncture as the experimental group with conventional treatment or sham acupuncture as the control group (Acupuncture vs. conventional treatment; Acupuncture vs. sham acupuncture; Acupuncture vs. clomiphene).
Four studies utilized the RR (Relative Risk) statistical measure. Three studies employed the MD (Mean Difference) statistical measure. A fixed-effects model was used. The results indicate that in the four studies using the RR measure, acupuncture treatment significantly impacted the occurrence of ovulation rates (RR: 1.25; 95% CI: 1.19, 1.31; I2=34.1%, pheterogeneity= 0.208; Figure 2C). However, in the three studies using the MD measure, acupuncture treatment did not have a statistically significant effect on the occurrence of ovulation rates (MD: 0.04; 95% CI: -0.07, 0.16; I2=92.8%, pheterogeneity< 0.001; Figure 2D). Sensitivity analysis on the studies using the MD measure revealed significant heterogeneity between the study by Jo J, et al., and the other studies (Figure 3B). After excluding this study, a random-effects model was applied (MD: 0.81; 95% CI: -0.46, 2.09; I2=88.9%, pheterogeneity= 0.003). Due to the limited number of studies using the MD measure and the sensitivity analysis only having two studies from the same literature, we cautiously conclude that acupuncture treatment significantly impacts the occurrence of ovulation rates (RR: 1.25; 95% CI: 1.19, 1.31; I2=34.1%, pheterogeneity= 0.208; Figure5A).
HOMA-IR: Three pieces of literature encompassing four studies on Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) were identified. Among these four studies, three studies involved acupuncture combined with conventional treatment (Acupuncture plus metformin vs. metformin; Acupuncture combined with conventional treatment vs. conventional treatment; Acupuncture combined with conventional treatment vs. conventional treatment) [5].
A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of HOMA-IR (MD: -0.35; 95% CI: -0.43, -0.26; I2=93.5%, pheterogeneity< 0.001; Figure 4G). Sensitivity analysis revealed significant heterogeneity between the studies by Liu Y, et al., and the other studies (Figure 3C). After excluding these two studies, a fixed-effects model was cautiously applied and the results showed a significant impact (MD: -0.33; 95% CI: -0.50, -0.17; I2=82.2%, p-heterogeneity=0.018; Figure 5B).
Testosterone levels: Four pieces of literature encompassing a total of ten studies on testosterone levels were identified. Among these ten studies, six studies involved acupuncture combined with conventional treatment (Acupuncture plus metformin vs. metformin; Acupuncture plus medication vs. metformin; Acupuncture plus herbal medicine vs. conventional treatment; Acupuncture plus herbal medicine plus conventional treatment vs. conventional treatment; Acupuncture plus herbal medicine plus conventional treatment vs. conventional treatment; Acupuncture plus medication vs. medication); one study had the experimental group with acupuncture combined with moxibustion and the control group with conventional treatment; two studies had the experimental group with acupuncture and the control group with sham acupuncture. One study had the experimental group with acupuncture and the control group with metformin.
A fixed-effects model was used. The results show that acupuncture treatment significantly impacts the reduction of testosterone levels (MD: -0.15; 95% CI: -0.19, -0.11; I2=89.0%, pheterogeneity< 0.001; Figure 4A). Sensitivity analysis revealed significant heterogeneity between the study Jo J, et al., and the other studies (Figure 3D). After excluding this study, a randomeffects model was cautiously applied and the results continued to show a significant impact (MD: -0.41; 95% CI: -0.62, -0.20; I2=88.2%, p-heterogeneity<0.001; Figure 5F).
LH levels: Four pieces of literature encompassing a total of ten studies on Luteinizing Hormone (LH) levels were identified. Among these ten studies, six studies involved acupuncture combined with conventional treatment (Acupuncture combined with medication; Acupuncture plus metformin vs. metformin; Acupuncture combined with medication vs. metformin; Acupuncture plus herbal medicine vs. conventional treatment; Acupuncture plus herbal medicine plus conventional treatment vs. conventional treatment; Acupuncture plus herbal medicine plus conventional treatment vs. conventional treatment); one study had the experimental group with acupuncture and the control group with sham acupuncture; one study had the experimental group with acupuncture combined with moxibustion and the control group with conventional treatment; one study had the experimental group with acupuncture and the control group with conventional therapy [6].
A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of LH levels (MD: -1.60; 95% CI: -1.90, -1.31; I2=72.9%, pheterogeneity< 0.001; Figure 4B). Sensitivity analysis revealed significant heterogeneity between the study by Li, PS, et al., and the other studies (Figure 3E). After excluding this study, a random-effects model was cautiously applied and the results continued to show a significant impact (MD: -1.56; 95% CI: -2.24, -0.88; I2=66.8%, p-heterogeneity=0.002; Figure 5E).
Fasting insulin level: Three pieces of literature encompassing a total of seven studies on fasting insulin levels were identified. Among these seven studies, three studies involved acupuncture combined with conventional therapy (Acupuncture plus metformin vs. metformin; Acupuncture combined with conventional therapy vs. metformin; Acupuncture combined with conventional therapy vs. metformin); one study had the experimental group with acupuncture and the control group with sham acupuncture; one study had the experimental group with acupuncture combined with moxibustion and the control group with conventional therapy; two studies had the experimental group with acupuncture and the control group with conventional therapy.
A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of fasting insulin levels (MD: -2.29; 95% CI: -2.47, -2.12; I2=73.9%, p-heterogeneity<0.001; Figure 4F). Sensitivity analysis revealed no significant heterogeneity among the studies (Figure 3F).
Miscarriage rate: Three pieces of literature encompassing three studies on the miscarriage rate were identified. Among these three studies, one study involved acupuncture combined with conventional therapy and herbal medicine; one study had the experimental group with acupuncture and the control group with sham acupuncture.
A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of the miscarriage rate (RR: 0.76; 95% CI: 0.58, 0.99; I2=79.7%, pheterogeneity= 0.007; Figure 4D). Sensitivity analysis revealed significant heterogeneity between the study by Lim CE, et al., and the other studies (Figure 3G). After excluding this study, a random-effects model was applied and the results continued to show a significant impact (RR: 0.47; 95% CI: 0.31, 0.70; I2=0.0%, p-heterogeneity=0.746; Figure 5C).
Menstrual frequency: Two pieces of literature encompassing four studies on menstrual frequency were identified. A fixedeffects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of menstrual frequency (MD: -0.41; 95% CI: -0.63, -0.19; I2=40.8%, pheterogeneity= 0.167; Figure 4K).
Menstrual cycle: Two pieces of literature encompassing five studies on the menstrual cycle were identified. Among these five studies, four studies involved herbal medicine combined with acupuncture one study had the experimental group with acupuncture and the control group with conventional therapy.
A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the prolongation of the menstrual cycle (RR: 1.22; 95% CI: 1.17, 1.26; I2=83.9%, pheterogeneity< 0.001; Figure 4E). Sensitivity analysis revealed no significant heterogeneity among the studies (Figure 3H).
Adverse events: Two pieces of literature encompassing three studies on adverse events were identified. A fixed-effects model was used. The results show that acupuncture treatment does not have a statistically significant effect on the reduction of adverse events (RR: 0.95; 95% CI: 0.85, 1.07; I2=97.9%, pheterogeneity< 0.001; Figure 4I).
BMI: Five pieces of literature encompassing nine studies on BMI were identified. Among these nine studies, five studies involved acupuncture combined with medication (Acupuncture combined with conventional therapy vs. conventional therapy; Acupuncture plus herbal medicine vs. conventional treatment; Acupuncture plus herbal medicine plus conventional treatment vs. conventional treatment).
A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of BMI (MD: -1.28; 95% CI: -1.46, -1.10; I2=70.1%, pheterogeneity< 0.001; Figure 4C). Sensitivity analysis revealed significant heterogeneity between the study by Liu Y, et al., and the other studies (Figure 3I). After excluding this study, a random-effects model was applied and the results continued to show a significant impact (MD: -1.16; 95% CI: -1.56, -0.76; I2=63.1%, p-heterogeneity=0.008; Figure 5G).
Waist-hip ratio: Two pieces of literature encompassing four studies on waist-hip ratio were identified. Among these four studies, three studies involved acupuncture combined with medication (Acupuncture plus herbal medicine vs. conventional treatment; Acupuncture plus herbal medicine plus conventional treatment vs. conventional treatment). One study had the experimental group with acupuncture alone [7].
A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of waist-hip ratio (MD: -0.03; 95% CI: -0.03, 0.02; I2=93.7%, p-pheterogeneity< 0.001; Figure 4J). Sensitivity analysis revealed significant heterogeneity between the study Liang XY, et al., and the other studies (Figure 3J). After excluding this study, a random-effects model was applied and the results continued to show a significant impact (MD: -0.06; 95% CI: -0.09, -0.02; I2=86.6%, p-heterogeneity<0.001; Figure 5D).
FBG (Fasting Blood Glucose): Two pieces of literature encompassing three studies on Fasting Blood Glucose (FBG) were identified. A fixed-effects model was used. The results indicate that acupuncture treatment significantly impacts the reduction of FBG (MD: -0.36; 95% CI: -0.55, -0.17; I2=0.0%, pheterogeneity= 0.680; Figure 4H).
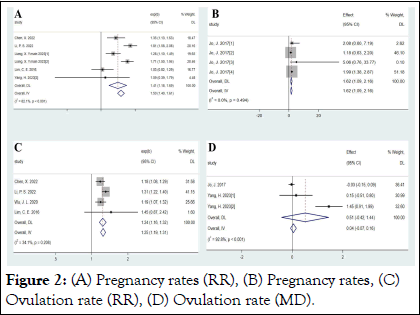
Figure 2: (A) Pregnancy rates (RR), (B) Pregnancy rates, (C) Ovulation rate (RR), (D) Ovulation rate (MD).
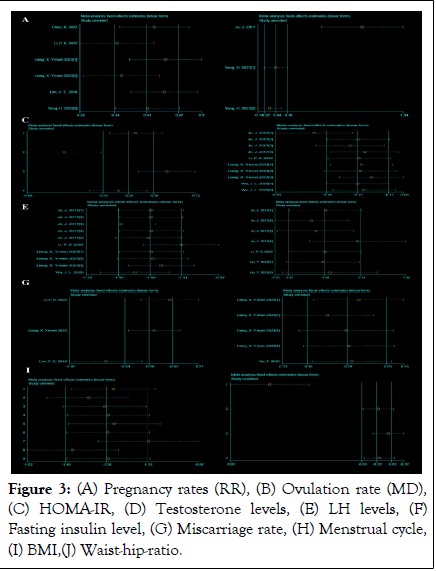
Figure 3: (A) Pregnancy rates (RR), (B) Ovulation rate (MD), (C) HOMA-IR, (D) Testosterone levels, (E) LH levels, (F) Fasting insulin level, (G) Miscarriage rate, (H) Menstrual cycle, (I) BMI,(J) Waist-hip-ratio.
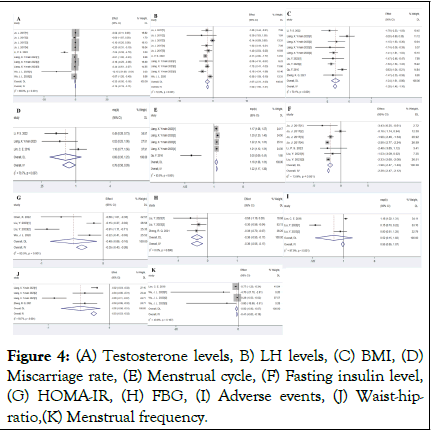
Figure 4: (A) Testosterone levels, B) LH levels, (C) BMI, (D) Miscarriage rate, (E) Menstrual cycle, (F) Fasting insulin level, (G) HOMA-IR, (H) FBG, (I) Adverse events, (J) Waist-hipratio,( K) Menstrual frequency.
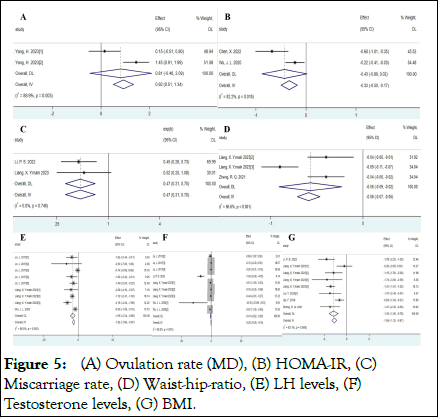
Figure 5: (A) Ovulation rate (MD), (B) HOMA-IR, (C) Miscarriage rate, (D) Waist-hip-ratio, (E) LH levels, (F) Testosterone levels, (G) BMI.
As research into Polycystic Ovary Syndrome (PCOS) progresses, it has been found that lifestyle interventions, including dietary control and moderate exercise, can reduce weight and improve metabolic conditions, thereby treating PCOS. However, the ultimate choice for treating PCOS, especially for patients with fertility requirements, remains pharmacological intervention, although its safety remains controversial.
It is important to find new and effective methods for treating PCOS and a promising example of this is acupuncture treatment. Previous studies have shown encouraging effects of acupuncture in treating PCOS, indicating that acupuncture therapy is a promising treatment strategy. In this context, several meta-analyses of observational and Randomized Controlled Trials (RCTs) have been conducted to assess whether acupuncture can treat PCOS, but existing meta-analyses and related RCTs still have shortcomings such as small sample sizes and single ethnicity. There is still controversy over the treatment of PCOS with acupuncture. This study is a comprehensive review of 10 meta-analyses, assessing the effectiveness of acupuncture in treating PCOS and related diseases. However, the impact of acupuncture on reducing adverse events is not statistically significant, suggesting that more evidence may be needed to support its safety [8].
In this study, based on the results of the meta-analysis, we found that acupuncture, with or without medication, can significantly treat PCOS. However, there is heterogeneity between different meta-analyses. For the high heterogeneity of the results, after conducting sensitivity analysis, there is still significant heterogeneity, so the results should be interpreted with caution. Although the overall effect of the previous meta-analysis was significant, there are also some controversies. The differences in the results can be attributed to different treatment plans and durations, different types of analyses, different meta-analysis qualities and different sample sizes.
In the included meta-analyses, we assessed the quality of the included meta-analyses using the AMSTAR 2 checklist (Table 2). This checklist includes 16 questions covering different aspects of the meta-analysis. Among all included studies, there are 2 highquality meta-analyses, 5 moderate-quality meta-analyses and 3 low-quality meta-analyses, indicating that our meta-umbrella results should be interpreted with caution; therefore, more research is needed to make our results conclusive.
|
Study |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Q8 |
Q9 |
Q10 |
Q11 |
Q12 |
Q13 |
Q14 |
Q15 |
Q16 |
Overall |
|
Chen X, 2022 |
√ |
× |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
× |
√ |
√ |
× |
× |
High |
|
Jo J, 2017 |
√ |
× |
√ |
√ |
√ |
√ |
√ |
× |
× |
× |
√ |
× |
× |
× |
× |
× |
Moderate |
|
Li PS, 2022 |
√ |
× |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
× |
× |
√ |
× |
× |
Moderate |
|
Liang X, Y Main, 2023 |
√ |
× |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
× |
× |
√ |
× |
× |
Moderate |
|
Lim CE, 2016 |
√ |
× |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
× |
High |
|
Liu Y, 2023 |
√ |
× |
√ |
× |
√ |
√ |
√ |
√ |
√ |
√ |
√ |
× |
× |
√ |
× |
× |
Moderate |
|
Qu F, 2016 |
√ |
× |
√ |
× |
√ |
√ |
√ |
√ |
× |
× |
√ |
× |
× |
√ |
× |
× |
Moderate |
|
Wu JL, 2020 |
√ |
× |
√ |
√ |
√ |
√ |
√ |
√ |
× |
× |
√ |
× |
× |
× |
× |
× |
Low |
|
Yang LJ, 2023 |
√ |
× |
√ |
× |
√ |
√ |
√ |
× |
× |
√ |
√ |
× |
× |
× |
× |
× |
Low |
|
Zheng RQ, 2021 |
√ |
× |
√ |
× |
× |
× |
× |
√ |
× |
× |
√ |
× |
× |
√ |
× |
× |
Low |
|
Note: |
|||||||||||||||||
Table 2: The results of quality assessment included meta-analyses based on AMSTAR2 questionnaire.
In polycystic ovary syndrome, various factors can affect ovarian function. PCOS not only leads to a series of complications but also reduces female fertility. The first-line drug treatment for PCOS patients is currently oral selective estrogen receptor modulators, such as clomiphene. However, it is ineffective in 40% of patients diagnosed with PCOS and is associated with significant side effects such as headaches, bloating, mood swings and breast tenderness. The use of metformin as an insulin sensitizer is also increasing, but the details of its mechanism of action remain elusive. Therefore, lifestyle interventions and acupuncture treatment for PCOS are increasingly valued.
Multiple studies have confirmed that acupuncture has a positive effect on promoting follicular development and improving pregnancy outcomes. As an alternative therapy, acupuncture has gradually been used in the treatment of PCOS and has been confirmed as a suitable method for treating PCOS. Clinical evidence suggests that acupuncture has a specific effect on improving the symptoms of PCOS. In the included metaanalyses and studies, by focusing on the impact of acupuncture or moxibustion or electroacupuncture on the pregnancy outcomes of PCOS patients, as well as the impact on fasting insulin, blood sugar and other metabolic levels, the clinical effects of acupuncture on PCOS have been objectively evaluated [9].
Our study has some advantages. To our knowledge, the current study is the first comprehensive analysis of acupuncture treatment for PCOS. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, which improved the transparency and reproducibility of the study. However, there are also some limitations in this study. The number of included studies is small and there is a certain degree of publication bias. We suggest further meta-analysis research in this direction. The quality of primary studies included in the meta-analysis is uneven and the quality of the meta-analysis is moderate; therefore, high-quality studies are needed in the future. In addition, we suggest further metaanalyses to separately evaluate acupuncture or electroacupuncture, as the effects of these two therapies may differ. We also suggest further meta-analyses to assess different treatment acupoints and the frequency of acupuncture. Since the main population included in the meta-analysis is PCOS patients, we cannot evaluate the impact of acupuncture on other female reproductive diseases; therefore, we recommend future research on this to better understand the more comprehensive impact of acupuncture [10].
This meta-analysis synthesizes existing meta-analyses on the treatment of PCOS with acupuncture, aiming to assess its impact on reproductive health indicators. Our results suggest that acupuncture offers a non-pharmacological treatment option for PCOS.
The high heterogeneity observed in this Meta-analysis may stem from various factors. Differences in study design, including the implementation of randomization and blinding, may affect the reliability of the results. Additionally, inconsistencies in patient baseline characteristics, such as age, Body Mass Index (BMI) and disease severity, may also influence the therapeutic effects. The diversity of acupuncture protocols, including acupoint selection, stimulation intensity and treatment frequency, further increases heterogeneity between studies. Future research should adopt standardized treatment plans and be validated in multicenter, large-sample studies.
As a non-pharmacological treatment method, the safety assessment of acupuncture is equally important. Although this meta-analysis did not find an association between acupuncture treatment and an increased risk of adverse events, existing studies have deficiencies in the assessment and reporting of adverse events. Considering the physiological responses that acupuncture may trigger, including pain, bleeding and infection risks, future studies need to adopt standardized adverse event assessment tools and conduct long-term follow-ups.
The application of the AMSTAR 2 tool revealed differences in methodological quality among the included meta-analyses. This highlights the need to strictly follow established methodological standards when conducting systematic reviews and metaanalyses. Future studies should adopt preset protocols, including clear inclusion and exclusion criteria, transparent reporting and comprehensive data analysis.
The results of this meta-analysis provide clinicians with scientific evidence on the treatment of PCOS with acupuncture. However, given issues with study quality and heterogeneity, clinicians should be cautious when recommending acupuncture treatment and conduct individualized assessments based on the specific circumstances of the patient. Moreover, clinical practice should consider combining other treatment modalities, such as lifestyle interventions and pharmacological treatments, to achieve optimal therapeutic outcomes.
This Meta-analysis indicates the potential efficacy of acupuncture in treating PCOS but also exposes various shortcomings in existing studies regarding design, execution and reporting. Future research should strive to improve methodological quality, reduce sources of heterogeneity and enhance the reliability and generalizability of the results. In addition, further exploration of the biological mechanisms of acupuncture, as well as its applicability and safety in different populations, will be an important direction for future research.
Rutong Wang: Data curation; investigation; resources; data organization; writing-original draft (lead author); conceptualization; formal analysis.
Yanhong Wei: Data organization; investigation; writing-original draft.
Bingsheng Huang: Investigation; writing-original draft.
Weihua Nong and Xiaocan Lei: Conceptualization; methodology; project administration; supervision; writing-review and editing.
Not applicable.
No animals/humans were used in this study.
The data and supportive information are available in the article.
This work was supported by the 2022 scientific research and technology development program of Baise city (no. 20224124) and hunan province innovation and entrepreneurship training program for college students (no. s202410555233).
The authors declare no financial or other conflicts of interest.
Thanks are extended to Clinical Anatomy and Reproductive Medicine Application Institute, Hengyang Medical School, University of South China, for their assistance.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Wang R, Wei Y, Zhu Y, Wang M, Nong W, Lei X (2025) Acupuncture for PCOS: A Meta-Analysis of Meta-Analyses. Endocrinol Metab Syndr. 14:441.
Received: 16-Aug-2024, Manuscript No. EMS-24-33503; Editor assigned: 21-Aug-2024, Pre QC No. EMS-24-33503 (PQ); Reviewed: 04-Sep-2024, QC No. EMS-24-33503; Revised: 03-Jan-2025, Manuscript No. EMS-24-33503 (R); Published: 10-Jan-2025 , DOI: 10.35248/2161-1017.25.14.441
Copyright: © 2025 Wang R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.