Journal of Hepatology and Gastrointestinal disorders
Open Access
ISSN: 2475-3181
ISSN: 2475-3181
Case Report - (2022)Volume 8, Issue 3
Introduction: Systemic AL amyloidosis is a serious disease. Its prognosis depends on the extent of the amyloid deposits and the extent of cardiac involvement. Without effective treatment, the median survival is approximately 12 months. About 10% of patients with multiple myeloma have associated AL amyloidosis. The survival of patients with AL amyloidosis and MM is significantly less than the survival of patients with AL amyloidosis alone. Otherwise, hepatic involvement is frequent, and it is reported in 70% of patients with amyloidosis. Factor X deficiency is a possible but rare complication of primary AL amyloidosis (6% of cases). It is thought to be the consequence of binding between factor X and amyloid in all organs, especially the liver and spleen.
Case: We report a case of hepatic AL amyloidosis associated with acquired factor X deficiency, of a 59-year-old man with no prior medical history who was admitted for epigastric abdominal pain with asthenia, weight loss and anorexia.On physical examination we found atrophy of the thenar and hypothenar eminences and hepatomegaly. Laboratory tests showed prolonged prothrombin time (PT=14%), increased alkaline phosphatase level to 3 times normal and gamma glutamyltransferase level to 13 times normal. Transaminases, bilirubin, albumin, hemoglobin and platelet counts were within normal limits. Coagulation factor assays revealed a significant reduction in factor X activity, <5%, and factor VII activity of 18%. Other clotting factor activities were not decreased, particularly factor V activity (78%). Virological and immunological markers of liver disease in plasma serum were negative. Hepatic ultrasound showed homogeneous hepatomegaly. Upper gastrointestinal endoscopy was normal. The evolution during hospitalization was marked by the appearance of diarrhea, ascitic edematous syndrome and orthostatic hypotension. Urinalysis detected proteinuria of (3 g/day), while protein electrophoresis showed a decrease in blood protein level to 23 g/L with a decrease in albumin level to 13 g/L. The serum creatinine level was decreased and the serum creatinine level increased. Systemic amyloidosis with renal and hepatic involvement was suspected. A salivary gland biopsy was performed, and an AL-type amyloid deposit was identified. A bone marrow aspiration was performed; the results were consistent with multiple myeloma. Treatment with chemotherapy (Melphalan) and high-dose prednisone was started. However, the patient worsened and died 6 months after the initial diagnosis of multiple myeloma associated with systemic AL amyloidosis. The level of factor X activity remained unchanged under treatment.
Conclusion: Systemic AL amyloidosis secondary to multiple myeloma with liver involvement associated with severe factor X deficiency is a severe and fatal form, which requires early diagnostic and therapeutic management.
Light chain amyloidosis; Multiple myeloma; Factor X deficiency
Amyloidosis is a rare disease characterized by the deposit in tissues of toxic insoluble protein aggregates in bundles of β-sheet fibrillar protein. This process generates progressive dysfunction of the affected organ system [1,2]. Light chain Amyloidosis (AL) is the most frequent form of amyloidosis. It results from an excess production of immunoglobulin light chains by clonal plasma cells which are deposited as amyloid fibrils [3]. Liver involvement is not uncommon in amyloidosis but usually presents with no specific symptoms and with poor prognosis [4]. The assurance diagnostic is provide by histological examination of hepatic parenchyma fragment, which show up tintorials properties, particlarly red coloration by “Red Congo” in polarised light examination and characteristic yellow-green birefringency.
Otherwise, coagulation factor deficiency is frequently encountered in amyloidosis, and is associated with a risk of potentially serious bleeding complications. A close association has been reported with amyloidosis AL and acquired deficiency of factor X [3,5]. We report a case of hepatic AL amyloidosis associated with acquired factor X deficiency.
59-year-old man with no past medical history was admitted for epigastric abdominal pain with asthenia, weight loss and anorexia. Physical examination revealed thenar and hypothenar eminence atrophy and hepatomegaly. Laboratory tests showed a prolonged prothrombin time (PT=14%), an increase in alkaline phosphatase level to 3 times normal=465 UI/L (normal value <150 UI/L) and in gamma glutamyltransferase level to 13 times normal=720 UI/L (normal value <55 UI/L). Transaminase, bilirubin, albumin, haemoglobin levels and platelet count were within normal limits. The coagulation factor assays revealed a significant reduction of factor X activity, <5% and a factor VII activity of 18%. Other coagulation factor activities were not decreased in particular factor V activity (78%). Virologic and immunological markers of hepatic diseases in plasma serum were negative.
A liver ultrasound showed homogeneous hepatomegaly. Upper gastrointestinal endoscopy was normal. During hospitalization, the patient suddenly presented with diarrhea and ascetic edematous syndrome. An orthostatic hypotension was also noted. The urinalysis detected proteinuria of (3 g/day), while protein electrophoresis showed that protein level accounted for 23 g/L with decrease of albumin level to 13 g/L. The serum creatinine level was increased 180 μmol/L (normal value <105 μmol/L). A systemic amyloidosis with renal and hepatic involvement was suspected. Salivary gland biopsy was performed, and amyloid deposition type AL was identified (Figures 1 and 2).
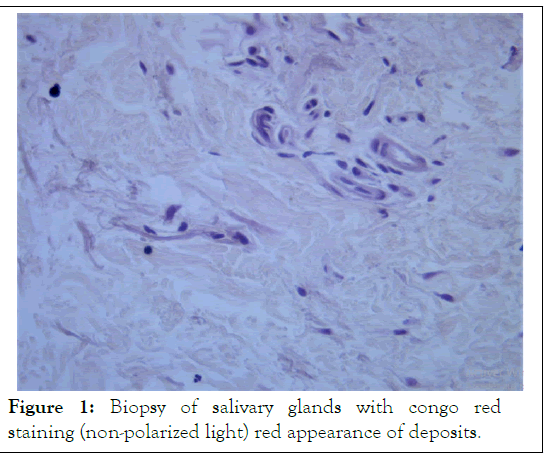
Figure 1: Biopsy of salivary glands with congo red staining (non-polarized light) red appearance of deposits.
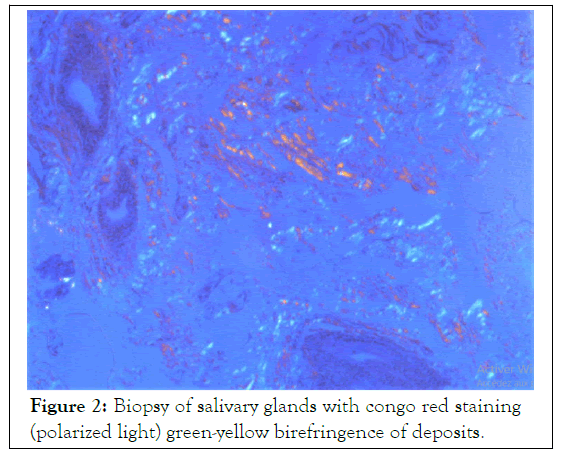
Figure 2: Biopsy of salivary glands with congo red staining (polarized light) green-yellow birefringence of deposits.
The patient underwent bone marrow aspiration and the findings were consistent with multiple myeloma (The presence of a medullary plasmacytosis greater than 10%). A chemotherapy based on Melphalan with high dose of prednisone was started. However, the patient’s condition progressively deteriorated and he died 6 months after the initial diagnosis of multiple myeloma associated with systemic AL amyloidosis. The level of factor X activity remained unchanged under treatment.
Systemic AL amyloidosis is the most common form of amyloidosis and in 15% of cases; it is associated with multiple myeloma as for our patient. The survival of patients with AL amyloidosis and multiple myeloma is significantly less than the survival of patients with AL amyloidosis alone. Hepatic involvement is actually frequent, and it is reported in 70% of patients with amyloidosis [2]. The majority of these patients presented with nonspecific symptoms such as fatigue and weight loss and in many cases hepatomegaly is described. Additionally, 61% of patients with hepatic AL amyloidosis had alkaline phosphatase levels of 500 U/I or more [5].
On other hand, 70% to 80% of the cases with hepatic amyloidosis associated nephrotic syndrome and neuropathic symptoms such as orthostatic hypotension [2,5]. Hepatic amyloidosis is mainly characterized by amyloid deposits in the liver parenchyma [2,6]. In some cases, the degree of amyloid deposition may be extensive enough to cause atrophy of hepatocytes and to interfere with the passage of bile. Hyperbilirubinemia is reported in about 5% of patients and confers a poor prognosis [2,6]. Additionally, the AL-type amyloid predominantly deposits within the space of Disease could lead to the increase in resistance to blood flow and portal hypertension secondary [7].
As described in the majority of cases in literature, our patient had asthenia, involuntary weight loss, hepatomegaly, orthostatic hypotension, nephrotic syndrome and cholestatic biological syndrome but with alkaline phosphatase level below to 500 UI/ L. On other side, he had a normal level of bilirubin and no clinical or endoscopic signs of portal hypertension. Due to coagulation factors deficiency, liver biopsy couldn’t be performed. It would have allowed appreciating the degree of amyloid infiltration of the liver. Acquired factor X deficiency is only observed in AL amyloidosis and it is the most common coagulation factor deficiency reported in 8.7% to 14% of patients according to recent reviews [8]. The mechanism by what factor X interacts with amyloid substance is still unclear but it is assumed that factor X is adsorbed into amyloid fibrils, which shortens the plasma half-life [9].
In a series of 32 cases of acquired factor deficiency over a study conducted par Choufani, including 368 patients with AL amyloidosis, more than 50% of patients experienced bleeding events and hepatic involvement was reported in 44% of cases [10]. Although, bleeding complications are relatively infrequent in systemic AL-amyloidosis with acquired factor X deficiency, and the baseline factor X level is not predictive of bleeding risk [11].
Our patient showed a severe factor X deficiency <5% but no bleeding event was reported. He received a treatment based on high dose of Melphalan chemotherapy and prednisone. This chemotherapy followed by autologous Stem Cell Transplantation (SCT) can lead to the amelioration of amyloid-related factor X deficiency as well as amyloid [10]. In our case, the physical deterioration under chemotherapy didn’t allowed the SCT and our patient died 6 months after initial diagnosis. This outcome confirms the poor prognosis of amyloidosis with hepatic involvement. Indeed, hepatic amyloidosis typically presents with advanced disease and dismal prognosis with a median survival of only 8.5 months based on available data [4,5].
That’s why some authors recommend to referral patients with hepatic amyloidosis to specialized amyloidosis centers where specific testing such as mass spectrometry to confirm amyloid protein composition and genetic testing which could permit to adapt therapy regimens and improve outcomes can be conduct. We have managed a patient with systemic AL amyloidosis secondary to multiple myeloma with hepatic involvement associated with severe factor X deficiency who survived only 6 months after diagnosis. This particular form often presents with nonspecific symptoms and needs an early diagnosis and a specialized management to improve outcome.
Citation: Mehrez CM, Hamzaoui L, Mahmoudi M, Khsiba A, Ayadi H, Chalbi E, et al. (2022) Acquired Factor X Deficiency in Amyloid Light-Chain Amyloidosis Associated with Myeloma: A Case Report. J Hepatol Gastroint Dis. 8:206.
Received: 18-Apr-2022, Manuscript No. JHGD-22-16907; Editor assigned: 21-Apr-2022, Pre QC No. JHGD-22-16907 (PQ); Reviewed: 06-May-2022, QC No. JHGD-22-16907; Revised: 12-May-2022, Manuscript No. JHGD-22-16907 (R); Published: 20-May-2022 , DOI: 10.35248/2475-3181.22.8.206
Copyright: © 2022 Mehrez CM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.