Research Article - (2023)Volume 8, Issue 2
Background: In 2017, the results of an 18-month follow-up showed only 0.002% of new HIV infections (of the 3/1069 in the high-risk group participating in PrEP treatment). In 2018, the HIV prevalence rate in the MSM group in Vietnam was 10.8%.
Methods: The study followed an analytical cross-sectional design and a sample size of 256 people, Research objective: determine the rate of adherence to PrEP and the factors related to non-adherence to PrEP. PrEP treatment and evaluation of PrEP treatment outcomes in high-risk subjects Subjects and research methods: People with HIV infection risk behaviors should register for PrEP treatment in Ba Ria-Vung Tau province in 2020.
Results: Men make up 52.7% of the population; the age group 21–40 makes up 80.5% of the population; the self- employed (46.4%), MSM (45.7%), and sex workers (39%); and PrEP adherence is 47.7%. Age, occupation, and use of condoms when having sex are factors associated with non-adherence to treatment with PrEP in a multivariate logistic regression analysis with variables when analyzing univariate regression with p<0.1. Only three subjects were newly infected with HIV.
Conclusion: Recommendations: counseling and support for treatment adherence, focusing on groups under 40 years old develop a peer network; guidelines for PrEP treatment include maintaining condom use during sex.
Drug; Adherence; Pre-exposure prophylaxis; Treatment
AIDS: Acquired Immunodeficiency Syndrome; ARV: Antiretroviral; HIV: Human Immunodeficiency Virus; FDA: Food and Drug Administration; FHI: Family Health International; FSWs: Female Sexual Workers; MSM: Men who have Sex with Men; PEP: Post-Exposure Prophylaxis; PEPFAR: The President’s Emergency Plan for AIDS Relief; PrEP: Pre-Exposure Prophylaxis; PWID: People Who Inject Drugs; STIs: Sexually Transmitted Infections; TGW: Transgender Women; UNAIDS: The Joint United Nations Programme on HIV and AIDS; USAID: United States Agency for International Development; WHO: World Health Organization
Pre-Exposure Prophylaxis (PrEP) is a new evidence-based biomedical Human Immunodeficiency Virus (HIV) prevention intervention that includes the daily (or event-based) pre-administration of Anti- retroviral Drugs (ARVs) to reduce the risk of HIV transmission if exposed. In Vietnam, PrEP is a combination of two antiretroviral drugs, Tenofovir Didoproxil Fulmarate (TDF) with strength of 300 mg and Emtricitabine with strength of 200 mg in one tablet with a daily dose of one tablet [1].
According to the World Health Organization, the Global Sector Strategy on HIV highlights the need to accelerate and focus on integrated HIV prevention, including the introduction of PrEP. In Vietnam, HIV prevalence among MSM has been increasing since 2011, increasing from 4% to 10.8% in 2018. In 2017, Vietnam piloted PrEP treatment in Ho Chi Minh City. In high-risk groups, the 18-month follow-up showed that there were only 3 new HIV infections among the 1069 men who had sex with men participating in PrEP [2].
Therefore, the use of PrEP has great potential, helping to prevent HIV and dominating the current HIV prevention and intervention strategy. At present, there aren’t any officially published data nationwide, and there aren’t any research studies to comprehensively evaluate PrEP treatment in general and PrEP adherence in particular. As a result, in 2021-2022, we conducted the study Study on treatment adherence, some related factors, and results of HIV pre-exposure prophylaxis in subjects with high-risk behaviors in Ba Ria-Vung Tau Province with the goals of determining the rate of adherence to PrEP, understanding some factors related to non-adherence to PrEP, and evaluating the results of PrEP treatment in patients. subjects with high-risk behavior in Ba Ria-Vung Tau province in 2021-2022.
Sample selection criteria
People aged 16 years or older who registered to participate and had a medical record of HIV pre-exposure prophylaxis from July 2019 to December 2020 were followed for 6 months until June 2021 at Ba Ria Vung Tau Province, had a negative HIV test result at the start of the study, registered for daily HIV pre-exposure prophylaxis, and agreed to participate in the study.
Exclusion criteria
People with contraindications to PrEP treatment; people with incomplete medical records; People with comorbidities must be hospitalized.
Study period and place
From January 2021 to July 2022, the study was conducted at two PrEP treatment centers in the Ba Ria-Vung Tau province, namely Vung Tau City and Phu My Town Health Center.
Design of a cross-sectional descriptive study
Research sample size: Apply the formula for calculating the minimum sample size for the proportional estimate, with the confidence coefficient a=0.05, the estimated ratio p=0.5, the choice error d=0.065, plus 10% sample size loss. The calculated sample size was 251 people. Actually, i studied 256 subjects.
Sampling method: Since the calculated sample size is close to the target population, we choose the whole sample.
Data collection method: Extraction of medical records combined with telephone interviews. Medical Center and Phu My Town Medical Center.
Research content
Study variables included information during the first 6 months of PrEP participation if treatment was 6 months or longer, or from the time subjects started participating to the end of PrEP treatment if treatment was shorter. 6 months. Research content includes demographic characteristics; high-risk behaviors for HIV infection; assessment of adherence to PrEP treatment through the assessment of three factors: drug adherence, test compliance, and follow-up compliance; Among the outcomes of PrEP treatment were an investigation of the response to PrEP therapy during both treatment and the outcome of new HIV infection after treatment.
Ethics
The study was approved by the Ethics Council in Biomedical Research at the Can Tho University of Medicine and Pharmacy in document No. 456/PCT-HDD dated July 15, 2021, and by the consensus of the Science and Technology Council of the Center for Disease Control in Ba Ria-Vung Tau province, the director of Vung Tau City Medical Center, and the director of Phu My Town Medical Center. The study is subject to the consent and voluntary participation of the research subject. The research content does not affect the rights, prestige or personality of the research participants and does not contain information or activities contrary to the customs and ethics of the research community and individuals.
Most of the study subjects were treated at Vung Tau City Medical Center (70.7%). Up to 98.8% of research subjects are from the Kinh ethnic group, accounting for a very high percentage. The proportion of men and women participating in the study was nearly equal. Most of the study subjects were between the ages of 21 and 40 (80.5%). The majority of the study subjects resided in urban areas, 5 times higher than those residing in rural areas; more than 80% of subjects belong to 3 main occupational groups, including freelancers, workers, flight attendants, and service staff; the two most common risk groups are men who are homosexual (45.7%) and women who engaged with regular sexual activity (39.1%) (Table 1).
| Characteristics | Frequency (n) | Rate (%) | |
|---|---|---|---|
| Prep and treament facility | Vung Tau Medical Center | 181 | 70,7 |
| Phu My Medical Center | 75 | 29,3 | |
| Ethnic | Kinh | 253 | 98,8 |
| Other ethnicity | 3 | 1,2 | |
| Sex | male | 135 | 52,7 |
| female | 121 | 47,3 | |
| Age group | ≤ 20 years old | 18 | 7,0 |
| From 21-40 years old | 206 | 80,5 | |
| From 41-60 years old | 31 | 12,1 | |
| Over 60 years old | 1 | 0,4 | |
| Residence | City | 213 | 83,2 |
| Rural | 43 | 16,8 | |
| Career | Freelance labor | 120 | 46,9 |
| Worker | 54 | 21,1 | |
| Waiter, Service Taff | 33 | 12,9 | |
| Other occupations | 49 | 19,1 | |
| Rist group | Men who have sex with men | 117 | 45,7 |
| Women selling sex | 100 | 39,1 | |
| HIV negative sexual partner | 38 | 14,8 | |
| People who inject drugs | 1 | 0,4 | |
Table 1: Some general demographic and social characteristics of the subjects (n=256).
Subject’s adherence to PrEP treatment
Study subjects tend to have better adherence to treatment and testing than to medication and follow-up visits. Overall adherence decreased significantly over 6 months. During the first month, all subjects stopped treatment without the consent of health workers. Gradually, the rate of discontinuation of prescribed treatment (with medical staff's consent) gradually increased from 27.3% in the 3rd month to 81.8% in the 6th month (Table 2).
| Characteristics | First month n=256 (%) | Third month n=247 (%) | Sixth month n=220 (%) | |
|---|---|---|---|---|
| Adhere to taking medication | 213 (83,2) | 160 (64,8) | 130 (59,1) | |
| Compliance with re-examination | 215 (84,0) | 169 (68,4) | 133 (60,5) | |
| Test compliance | 235 (91,8) | 202 (81,8) | 169 (76,8) | |
| Adherence | 210 (82,0) | 159 (64,4) | 114 (51,8) | |
| Who stopped Prep | Consent of medical staff | 0 (0) | 9 (27,3) | 27 (81,8) |
| Not consent of medical staff | 18 (100) | 24 (72,7) | 6 (18,2) | |
| Total | 18 (100) | 33 (100) | 33 (100) | |
Table 2: Surveyed PrEP adherence and PrEP discontinuation rates at follow-up visits.
The percentage of study subjects that adhered to PrEP treatment was still low (47.7%) (Figure 1).
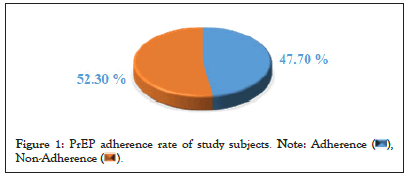
Figure 1: PrEP adherence rate of study subjects. 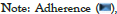
Some factors related to subjects' non-adherence to PrEP treatment
People aged 40 and under who do not adhere to treatment are 5.045 (1.816-14.010) times more numerous than the group of people over 40 years old. The group of workers who do not adhere to treatment is 0.317 (0.120-0.838) times higher than that of other occupations, which means that the group of workers who comply with treatment is 3.15 times higher than that of other occupations. The group of subjects who used safety contraceptions during sex did not adhere to treatment 3.527 (1.871-6.647) times more than the group that did not use condoms during sex (Figure 2 and Table 3).
Figure 2: PDepicts the response rate of study participants to PrEP
treatment and the rate of study subjects responding to PrEP treatment was
still low (46.1%). 
| Independent variables | OR | 95% CI | p | ||
|---|---|---|---|---|---|
| Age | ≤ 40 years old | 5.045 | 1.816 | 14.01 | 0.002 |
| >40years old | 1 | - | - | - | |
| Career | Freelance labor | 2.13 | 0.903 | 5.025 | 0.084 |
| Worker | 0.317 | 0.12 | 0.838 | 0.02 | |
| Waiter, Service taff | 0.854 | 0.281 | 2.596 | 0.781 | |
| Other Occupations | 1 | - | - | - | |
| Use condoms during sex | Yes | 3.527 | 1.871 | 6.647 | <0.001 |
| No | 1 | - | - | - | |
Table 3: Some factors related to non-adherence to PrEP (multivariate logistic regression model).
More than two-thirds of the subjects received PrEP treatment at the Medical Center of Vung Tau City because this is the first place to implement PrEP treatment in Ba Ria-Vung Tau province (July 2019). The health center in Phu My Town is deployed later (in July 2020). The age group 21-40 accounted for the highest percentage (80.5%), which is four times higher than the total of the remaining age groups. This is the period when people perform many activities and occupations with a high risk of HIV infection, and their social relationships are more complicated than those of other age groups. The subject’s average age was 32.1 ± 8.4 years. This average age is higher than the studies of Katherine (24.7 years old), Pich (28.9 years old), and Elizabeth. Wahome (25 years old) and lower than the study of Thomas HF Whitfield (37.67 years old) [3-6]. There is a difference in average age because of differences in cultural and social life. In most Western countries, adolescents reach adulthood early and engage in high-risk behaviors at a very young age, so those at high risk for PrEP are also younger than in Vietnam. However, in general, the difference in mean age between the studies is not large, and the same age group is 21-40, which is the age with the highest HIV prevalence in Vietnam and the world.
Because the two main groups of people who come for PrEP treatment are men who have sex with men (45.7%) and women who sell sex (39.1%), there is not much difference in the sex ratio of the subjects. (52.7% men and 47.3% women). This finding differs from Kimberly's previous research. Elizabeth Green, Alyson Hillis, Elske Hoornenborg, and Dou Qu were present when the authors chose MSM as the research subject [7,8]. The difference was that we aim to study all PrEP subjects in Ba Ria-Vung Tau province, not just MSM, which was the most popular and most successful group in the program. The PrEP program has been proven through many studies around the world and the PrEP demonstration project in Ho Chi Minh City.
The majority of study subjects residing in urban areas accounted for 83.2% of the total, five times more than those residing in rural areas. This result is similar to that of the study by Qu et al. 74% of the study subjects were in urban areas [8]. There is a similarity because urban areas have a complex living environment, a dense population, developed service industries, many social evils, and many potential risks, so the number of high-risk subjects is large. On the other hand, urban areas have developed information and communication facilities and a wide peer-to-peer network makes it easier for information about PrEP to reach high-risk populations. Up to 80% of subjects are employed in one of three major occupational groups: self-employed, workers, attendants and service staff. These are some of the occupations that are exposed to many high-risk groups, with most of the female sex workers claiming to be self-employed. We studied the 6-month treatment course of the subjects, determining the treatment adherence at the 1-month, 3-month and 6-month time points. The results found that, at each evaluation time, the rate of compliance with the test was always the highest and the rate of compliance with taking medication was the lowest. Because medical staff decides on testing in advance, testing for customers every time they come in for a follow-up visit simply cannot be done when the customer does not come. And because taking the drug is a relatively long process (because it is a daily oral PrEP), it requires the patience and self-discipline of the customer. Out of 256 subjects, 84 people (accounting for 32.8%) stopped treatment; this rate is still high. Especially in the first month, up to 100% of subjects stopped PrEP treatment without the consent of medical staff. The percentage of study subjects that adhered to PrEP treatment over 1 month, 3 months and 6 months gradually decreased significantly, to 82%, 64.4% and 51.8%, respectively. Maintaining the treatment until the 6th month, only 51.8% of the subjects still adhered to the treatment (a decrease of nearly half compared to the first month). This result is much lower than that of the author, Green, et al. According to Kimberly Elizabeth Green, at the end of month 1, self-reported PrEP compliance was over 90% at all times in the MSM. The study showed that the rate of adherence at the 3rd, 12th, and 18th months was 88.7%, 68.8% and 46.6%, respectively [9]. There is a difference because the two studies are different in terms of subjects. Author Kimberly Elizabeth Green mostly performed on the MSM group, while our study included the MSM group, sex workers, heterosexual partners, injecting drugs, etc. and different assessment timelines. In addition, because this is a new issue and studies are still interested in each individual content and subject, there is no exact definition of adherence to PrEP in general, so the standard for classification of treatment adherence may vary between studies. Considering the whole treatment process, the percentage of subjects adhering to PrEP was 47.7%. This result is lower than in the prospective cohort study from 2017 to 2020 conducted in West Africa by Laurent, et al. The author reported that 41% of subjects adhered to situational PrEP and 71% of subjects complied with daily PrEP [10]. This difference may be due to the two studies being conducted in different geographical areas with many differences in culture, socio-economic conditions, and daily behavior. In addition, the target group is not the same as when author Christian Laurent performed it in the MSM group, and we performed it on all high-risk subjects participating in PrEP treatment, so the adherence to treatment is different, especially because MSM subjects are considered to be the most suitable and most effective for PrEP treatment, so a higher adherence rate is appropriate. On the other hand, the HIV prevalence rate in West Africa is also higher than in Vietnam, which may also be a contributing factor in promoting adherence to HIV/AIDS prevention measures, including adherence to PrEP. However, when compared with the results of the above studies, although there are arguments based on science and practice, it is necessary to recognize the results of the lower overall adherence rate for PrEP treatment in Ba Ria-Vung Tau province. This is the scientific basis for the need to improve treatment quality, strengthen consultation, provide guidance, and develop practical solutions to improve the rate of adherence to HIV pre-exposure prophylaxis in the Ba Ria Vung Tau province in the coming time.
We found several factors related to non-adherence to PrEP treatment in subjects, including age group, occupation, and use of condoms during sex. People aged 40 and under who do not adhere to treatment with PrEP had 5,045 times higher than that of subjects over 40 years old (OR=5,045; 95% CI: 1,816-14,010). In our study, middle-aged subjects adhered better to treatment because of the maturity of their thoughts. They care about their health and take better care of their families, especially because of their anxiety and a sense of health protection; their experience in life and determination in disease prevention made them more serious about carrying out the requirements under the guidance of the doctor. The group of subjects under 40 years of age had poorer adherence to treatment; this result is quite similar to Yun’s study on 24,193 subjects in 2017, except for women and children, who by nature always worry about their health, which showed that female and younger subjects (under 30 years old) have a higher level of adherence to medication [11]. The study by author Pasipanodya on the trajectory and prediction of adherence to longitudinal exposure prevention measures in MSM also had similar results when detecting a younger age group and ethnicity. Ethnic minorities are associated with lower levels of compliance [12]. In addition to the target groups designated as subjects of the PrEP program, Vietnam now extends its attention to other subjects, such as issuing temporary guidance documents for PrEP implementation for pupils and students. The group of workers who have the highest risk of adherence to treatment is 0.317 times larger than the group of subjects with other occupations (OR=0.317; 95% CI: 0.120-0.838). It is understood that the group of workers who adhere to treatment is 3.15 times higher than that of other occupations. Compared with other high-risk occupational groups, workers are those with relatively more fixed working hours are familiar with compliance with rules and procedures in labor and production are accustomed to a disciplined, technical, and productive working style and are used to working in shifts and teams. While adherence to PrEP has similar compliance requirements, they are easier to adapt to and comply with [12].
Those who used condoms during sex were 3,527 times more likely to not adhere to treatment than those who did not use condoms during sex (OR=3,527; 95% CI: 2,520-12,258). The question arises: why are condoms easier to use, more convenient, and simpler than a strictly regulated process of PrEP, but those who do not wear condoms when having sex can comply with the regulations? Better PrEP treatment, because condoms reduce pleasure and desire and PrEP does not. This shows the gaps in the way towards eliminating HIV/AIDS. With all our efforts, we do not deny that the HIV prevention measures that have been used, especially the promotion of condoms when having sex, have brought a lot of results, great results. However, the survey in this study demonstrates that no single measure is optimal and that it is necessary to deploy many measures in tandem to achieve the desired effect. And PrEP was born as a new and potential measure, supporting additional protective barriers, increasing the chances of being healthy for highrisk people and reducing HIV infection. On the other hand, we refer to the study by Irungu, et al. which discussed condom use among PrEP users and health care providers in Kenya. According to research by Irungu, most healthcare providers recommend that PrEP users always use both PrEP and condoms, unless they are trying to conceive. PrEP providers say PrEP users are sometimes confused, even frustrated, when advised to use condoms in addition to PrEP. PrEP users often view PrEP as a more viable and desirable HIV prevention method than condoms, increasing sexual pleasure and conception while reducing conflict and the stigma associated with condom use [13]. Although the results of the study indicate that subjects who do not use condoms will have a higher adherence to PrEP treatment, it is still more important to recommend that subjects use a combination of PrEP and condoms to maximize disease prevention. At the end of treatment, the response rate to PrEP was 46.1% and only 1 subject tested positive for HIV. This result is higher than that of the pilot project for PrEP treatment in Minh City, where there was no case of HIV seroconversion after 12 months. On the one hand, our study has a significantly lower percentage of subjects with treatment adherence, which affects the quality of HIV exposure prophylaxis. Subjects newly infected with HIV in the study were non-adherent to PrEP treatment. On the other hand, subjects newly infected with HIV after 3 months of PrEP treatment should not exclude the cause when participating in PrEP and 1 month later, during the subject's window period, appearing falsely negative for an HIV test. The results of our study are also higher than those of the study by Tassi, et al. which recorded 29 new HIV infections, leading to an incidence rate of 0.19 cases per 100 people per year [14]. Maybe due to geographical differences (France and Vietnam), differences in culture and lifestyle, and differences in the knowledge, attitude and behavior of subjects about HIV/AIDS prevention and control in general and PrEP treatment in particular, there is different adherence to PrEP treatment. In particular, the study of Tassi was carried out on 9,893 people. The large difference in the number of study participants (9,893 versus 256) also affects the statistical ratio and the level of representation, leading to the insignificant comparison. In the study by Olsen, et al. a situational dose of PrEP reduced the number of subjects at risk for new HIV infection by 86%. This rate for daily PrEP is 44-86% [15]. However, when using PrEP, the rate of condom use decreases markedly over time, which also has many potential risks.
The rate of adherence to PrEP (pre-exposure prophylaxis for HIV) among subjects with high-risk behaviors for HIV infection was 47.7%. Some factors related to the study subject’s adherence to PrEP treatment are age, occupation, and use of condoms during sex. During the process of using PrEP to prevent HIV exposure, 46.1% of subjects achieved good prevention results. One subject turned HIV-positive while on PrEP treatment. It is necessary to improve the effectiveness of counseling and support for treatment adherence, especially for those under the age of 40. Promote the development of a network of peers and community groups to increase referrals, increase the number of customers, and help advice and support better treatment adherence for subjects. Consolidate and complete the process of management, counseling, treatment, and monitoring of PrEP treatment subjects, limiting treatment discontinuation due to loss of track. Men on PrEP should be instructed to combine condom use with having sex to prevent not only HIV transmission but also other sexually transmitted diseases.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the Can Tho University of Medicine and Pharmacy under Decision No. 456/PCT-HDDD signed on July 15, 2021, and with the consent of the City Health Center. Vung Tau and Phu My District Medical Center the procedures performed in this study adhered to the tenets of the Declaration of Helsinki. (from pre-study protocol approval to implementation monitoring and post-study reporting). All study participants were selected when they agreed and checked the consent section of the research questionnaire. All study participants have the cognitive ability and have given their informed consent, and they have the right to discontinue participation at any time during the study.
We hereby confirm that all experimental protocols (specifically, giving oral PrEP to subjects at risk of HIV exposure) have been approved by the medical ethics committee of the Can Tho University of Medicine and Pharmacy and the directors of Vung Tau City Medical Center and Phu My Town Medical Center.
The data and documents checked by the Can Tho University of Medicine and Pharmacy meet new requirements for conducting research. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
DPL, NVL, and TND jointly produced the ideas and the study design. DPL and NVL developed the survey tools. DPL and NVL Write a draft outline, Collect data and put it into SPSS software. Write a draft of the entire research topic. DPL and TND Check and revise the research outline; process research data. Discussions and recommendations should be in writing. All authors (DPL, NVL, and TND) read and reviewed the entire content of the topic and agreed to submit the manuscript to the Journal of Immunogenetics.
We would like to express our gratitude and respect to patients and their families who agree to and voluntarily contribute to the research's success.
We would like to express our sincere thanks and deepest gratitude to: Ladies and gentlemen on the Board of Directors; The Ethics Committee of Can Tho University of Medicine and Pharmacy, especially Associate Professor Dr. Nguyen Trung Kien, Rector of the University, has enthusiastically helped and supported the Faculty of Public Health. Our special collaborators are Dr. Nguyen Van Nen and Assoc. Prof. Dr. Tran Ngoc Dung, who have provided support to complete the study.
I'd like to express my heartfelt appreciation to the Board of Directors, Science and Technology Council, and Staff of the Methadone Treatment Department at Vung Tau City Medical Center; and the Board of Directors and Staff of the Examination Department at Phu My Medical Center.My town enthusiastically helped and supported me in the process of conducting this research.
I would like to thank my colleagues, research institutions, friends, family, and relatives who encouraged and supported me throughout the research process.
I sincerely appreciate everyone's good feelings and valuable help.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Duong LP, Nguyen LV, Tran DN (2023) A Study on the Adherence of Treatment, Associated Factors, and Outcomes of Oral Pre-Exposure Prophylaxis for High-Risk Patients' HIV Exposure in the Ba Ria-Vung Tau Province from 2021 To 2022. Immunogenet Open Access. 8:201
Received: 16-May-2023, Manuscript No. IGOA-23-24028; Editor assigned: 18-May-2023, Pre QC No. IGOA-23-24028 (PQ); Reviewed: 01-Jun-2023, QC No. IGOA-23-24028; Revised: 08-Jun-2023, Manuscript No. IGOA-23-24028 (R); Published: 15-Jun-2023 , DOI: 10.35248/IGOA. 23.8.201
Copyright: © 2023 Duong LP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.