Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research - (2020)Volume 10, Issue 3
Background: Twin pregnancies continue to be associated with increased perinatal morbidity and mortality. The aim of this study is to describe our experience with twin deliveries and provide this data as reference.
Methods: In this retrospective study, twin deliveries occurring after 22+0 weeks of gestational age in the Department of Obstetrics and Gynecology, University Hospital Ulm were analyzed. 1663 datasets (including 3326 children) were available for analysis.
Results: Over time there was an average of 83 twin births per year (median 80, range 56 - 104) in our department, with a significant increase in the number of twin births per year over time (n = 20, rs = 0.821, p < 0.001). The average maternal age was 31 years (range 17 - 47), and in the time frame maternal age significantly increased (rs = 0.167, p < 0.001). The median gestational age at delivery was 35 weeks (range 22+0 - 42+0 weeks). Overall, 400 (20.1%) twin
births had a planned/elective cesarean section (C/S). In 575 (34.6%) cases both twins were delivered vaginally and in 641 (38.5%) cases both twins were delivered by secondary (unplanned / emergency) C/S. In 47 (2.8%) cases, the first twin was born vaginally, and the second twin by secondary C/S. Of the 575 vaginal twin births, both twins were born spontaneously in 471 (81.9%) and by assisted vaginal delivery in 24 (4.2%) cases. In 53 (9.2%) cases the first twin was
born by assisted vaginal delivery while the second twin was born spontaneously, and for 27 (4.7%) twin births this pattern was reversed.
Conclusions: The optimal mode of delivery of twins is still a subject of continuing debate. Though the database provides very detailed information on the delivery it is not possible to draw clinical conclusions from our results as these need to be evaluated in prospective randomized trials.
Gemini; Twins; Delivery; Outcome; Retrospective; Pregnancies
ACOG: American College of Obstetricians and Gynecologists; C/S Or CS: Cesarean Section; CTG: Cardio Toco Gram; EDD: Expected Due Date; GA: Gestational Age; IQR: Inter Quartile Range; NICHD: National Institute of Child Health and Human Development; SMFM: Society for Maternal-Fetal Medicine; WHO: World Health Organization
Conflicting data exists about the ideal mode of delivery for twin pregnancies. Most of the studies focus on the presentation of the (leading) twins and the gestational age at delivery. It is commonly accepted that a twin pregnancy is considered a risk pregnancy with increased ante- and intranatal risks. These risks range from complications related to chorionicity, malpresentation, discordant growth, twin-twin transfusion syndrome, cord prolapse, peripartal asphyxia and premature birth. Statistically has the first-born twin a lower morbidity risk than the second-born. With the rapid development and commonly use of intrapartum surveillance and postpartum care delayed deliveries of the second twin have become possible. Such reports of delayed twin deliveries in the second trimester have been reviewed by Cheung. Of course this approach is purely experimental but would hardly be possible with a cesarean section. And according to the authors the perspective for the second twin is more promising. But the maternal morbidity rate is as high as 39% [1-10].
Also in obstetrics there is always a parental bias. Some parentsto- be have not spared financial and temporal resources to come this way and are more than willing to accept this risk. In return expect the best delivery mode and postpartum care.
The debate starts at the optimal time of delivery. Preterm birth (delivery before 37 weeks of gestational age (GA) occurs in more than 50 percent of twin pregnancies. The chorionicity and the presentation of the leading twin have classified subgroups.The American College of Obstetricians and Gynecologists (ACOG) suggests elective delivery of uncomplicated dichorionic, diamniotic pregnancies between 380 and 390 weeks of GA, of monochorionic, diamniotic twin pregnancies between 340 and 380 weeks of GA and of monochorionic, monoamniotic twins between 320 and 340 weeks of GA (American College of Obstetricians and Gynecologists, 2013; Committee on Practice Bulletins-Obstetrics and Society for Maternal–Fetal Medicine. ACOG recommends offering a vaginal delivery for diamniotic twins when the first twin is in vertex presentation regardless of the presentation of the second fetus as per American College of Obstetricians and Gynecologists in 2013. Monoamniotic twins are always delivered by cesarean section (C/S) due to the high risk of cord complications.
If a trial of labor is offered the team should be able to perform emergency C/S within the recommended timeframe. In Germany perinatal centers of the highest standard (level 1) are required to maintain decision to delivery time of 20 minutes or less [11]. These precautions are necessary as a trial of labor reportedly ends in a C/S in 10% to 30%.
This internal audit compares our standard of care against the literature and describes our experience with twin deliveries. Our clinical data may be a valuable reference/benchmark for other delivery wards.
The detailed questions to be answered are:
• Has there been an increase of twin pregnancies over the last 2 decades
• Has there been a change of mode of delivery
• Has the outcome improved in the last 20 years
• Do the worst cases have something in common
Our data was retrieved from a first world, level three university hospital. The obstetrics and pediatrics units provide the highest level of ante- and postpartum care in its geographical area with the closest neighboring university being 110 km away. The basic obstetric quality is surveyed annually by the state. Our results provide a detailed longitudinal retrospective observation on the twin delivery outcome.
The general approach to twin parents-to-be is open for trial of vaginal birth. A planned cesarean section was strictly recommended in mono-amniotic twins leading twin in breach position and a more than 500 g lower estimated weight in the leading twin. In premature twins delivery mode was decided on the situation sometimes enabling a delayed second twin delivery. In this retrospective study, twin deliveries occurring after 220 weeks of GA in the Department of Obstetrics and Gynecology, University Hospital Ulm were analyzed. After excluding deliveries with incomplete data, 1663 datasets (including 3326 children) were left for analysis.
In the database information on maternal age at delivery, parity and gravidity, age of gestation at time of delivery, planned delivery mode, delivery time of both children, time interval between delivery of the twins, birth weight of both twins, neonatal outcome indicators (pH of the umbilical vessels) was collected and considered as a complete dataset. The database did not contain information on chorionicity.
An umbilical artery pH ≥ 7.18 at birth was considered normal. Acidosis was defined as slight (pH<7.18) moderate (pH<7.10) and severe (pH<7.00).
The expected due date (EDD) was determined by the last menstruation prior to the pregnancy. If the EDD of the early pregnancy/dating scan differed for 7 or more days from the menstruation EDD the GA was adjusted according to the ultrasound measurements.
The planned delivery mode was defined as primary (planned) C/S or trial of labor (i.e., vaginal delivery). The mode of delivery was defined as (primary (planned) C/S; secondary C/S (i.e., unsuccessful trial of labor); vaginal delivery (including vacuum extraction (ventuouse) or forceps).
Data on categorical variables were summarized using absolute and relative frequencies. Associations between categorical variables were analyzed with the chi-squared test or Fisher’s exact test (if expected frequencies in 2 × 2 cross tabulations were less than 5). As the distribution of all quantitative (metric) variables included in this study differed significantly from normal, these variables were described using median, inter quartile ranges and ranges. Accordingly, statistical comparisons between groups with regard to metric variables were performed by the non-parametric Mann-Whitney-U test (for comparisons between two groups) or the Kruskal Wallis test (for comparisons among three or more groups). Correlationsbetween metric variables were calculated using the non-parametric Spearman correlation coefficient rs. Comparisons among groups are illustrated using Box-and- Whisker plots, where the horizontal line inside the box represents the median and the box indicates the inter quartile range (IQR; the middle 50% of scores). The ends of the whiskers denote the lowest and highest values still within 1.5 IQR of the lower and upper quartile (i.e., the lower and upper end of the box), respectively. If there are no values more than 1.5 IQR below the lower or above the upper quartile (i.e., outliers), the ends of the whiskers denote minimum and maximum of the data. Outliers that are more than 1.5 IQR but less than 3 IQR below the lower or above the upper quartile are indicated by open circles, and extreme outliers more than 3 IQR below the lower or above the upper quartile are indicated by stars. All statistical analyses were performed with SPSS Statistics version 22 software; all statistical tests were two-tailed, and a pvalue of less than 0.05 was considered statistically significant.
After excluding incomplete datasets 1663 twin births were available for analysis (Table 1 gives further details). Over time there was an average of 83 twin births per year (median 80, range 56-104) in our department, with a significant increase in the number of twin births per year over time (n=20, rs=0.821, p<0.001 (Figures 1-6).
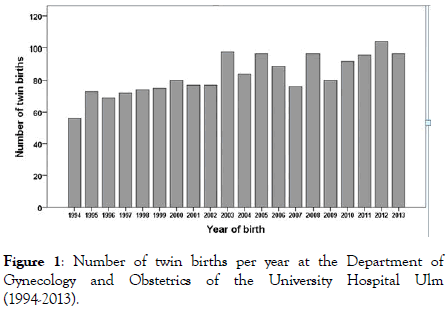
Figure 1: Number of twin births per year at the Department of Gynecology and Obstetrics of the University Hospital Ulm (1994-2013).
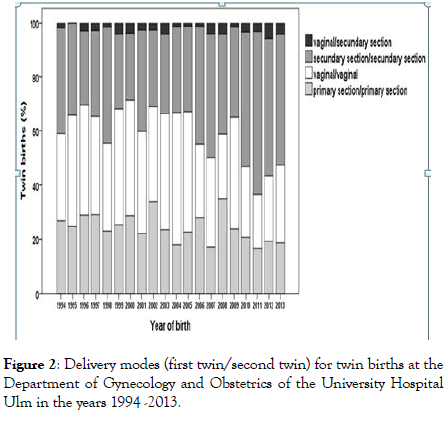
Figure 2: Delivery modes (first twin/second twin) for twin births at the Department of Gynecology and Obstetrics of the University Hospital Ulm in the years 1994 -2013.
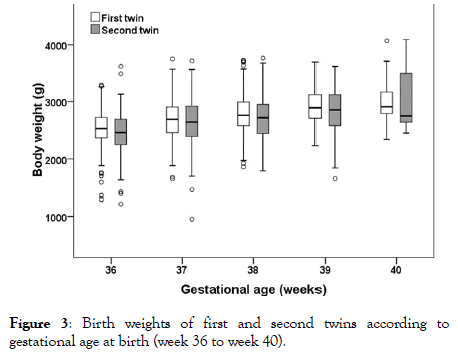
Figure 3: Birth weights of first and second twins according to gestational age at birth (week 36 to week 40).
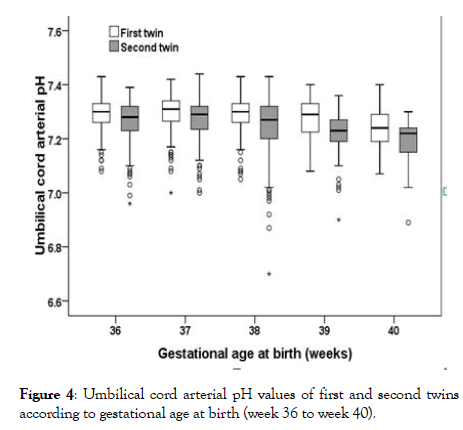
Figure 4: Umbilical cord arterial pH values of first and second twins according to gestational age at birth (week 36 to week 40).
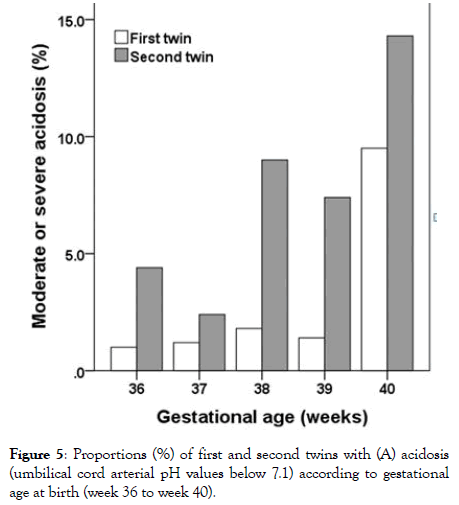
Figure 5: Proportions (%) of first and second twins with (A) acidosis (umbilical cord arterial pH values below 7.1) according to gestational age at birth (week 36 to week 40).
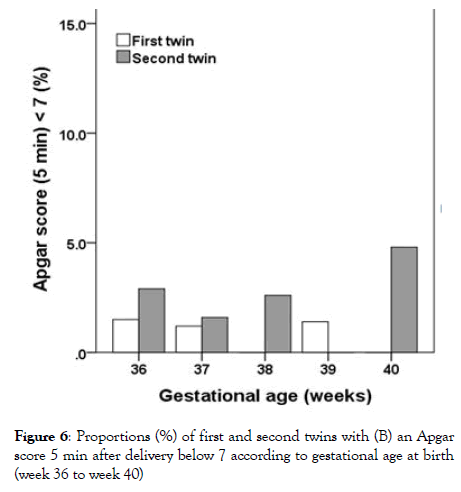
Figure 6: Proportions (%) of first and second twins with (B) an Apgar score 5 min after delivery below 7 according to gestational age at birth (week 36 to week 40)
| Variables | Total N=1663 |
|---|---|
| Maternal age (years) | |
| Median | 31 |
| Interquartile range | 28.0 - 34.0 |
| Range | 17-47 |
| Parity | |
| Primiparous | 929 (55.9%) |
| Multiparous | 734 (44.1%) |
| Gestational age at birth (weeks) | |
| 22 - 23 | 23 (1.4%) |
| 24 - 25 | 50 (3.0%) |
| 26 - 27 | 59 (3.5%) |
| 28 - 29 | 88 (5.3%) |
| 30 - 31 | 100 (6.0%) |
| 32 - 33 | 177 (10.6%) |
| 34 - 35 | 337 (20.3%) |
| 36 -37 | 460 (27.7%) |
| 38 - 39 | 340 (20.4%) |
| 40 - 42 | 29 (1.7%) |
| Mode of delivery (first twin/second twin) | |
| Vaginal/vaginal | 575 (34.6%) |
| Primary section/primary section | 400 (24.1%) |
| Secondary section/secondary section | 641 (38.5%) |
| Vaginal/secondary section | 47 (2.8%) |
| Fetal sex (first twin/second twin) | |
| Male/Male | 564 (33.9%) |
| Male/Female | 277 (16.7%) |
| Female/Male | 287 (17.3%) |
| Female/Female | 534 (32.1%) |
| Unknown | 1 (0.1%) |
| Fetal position (first twin/second twin) | |
| Cephalic/Cephalic | 799 (48.0%) |
| Cephalic/Breech | 456 (27.4%) |
| Breech/Cephalic | 195 (11.7%) |
| Breech/Breech | 210 (12.6%) |
| Other | 3 (0.2%) |
| Weight difference between first and second twin | |
| First twin heavier | 969 (58.3%) |
| Second twin heavier | 674 (40.5%) |
| Both twins with equal weight | 18 (1.1%) |
| Unknown | 2 (0.1%) |
| Time interval between birth of first and second twin (min) | |
| Median | 2 |
| Interquartile range | 01-Sep |
| Range | 0- 243 |
Table 1: Baseline maternal characteristics and birth data for 1663 twin births at the Department of Gynecology and Obstetrics of the University Hospital Ulm (1994 -2013).
The average maternal age was 31 years (range 17-47), and in the time frame maternal age increased significantly increased, with a median age of 29 years in 1994 and 32 years in 2013 (rs=0.167, p<0.001). The majority (55.9%) were primiparous. The proportion of primiparous and multiparous women did remained constant over the 20 years investigated (Chi-square test, p=0.498).
The median gestational age at delivery was 35 weeks (inter quartile range 330–370 weeks, range 220-420 weeks). Only 73 (4.4%) of the pregnancies did not complete 250 weeks of gestation. 497 (29.9%) twin deliveries were before 340/6 weeks, and 29 (1.7%) deliveries took place after 390/6 weeks. GA at delivery did not change significantly over the study period (Kruskal-Wallis test, p=0.562).
Overall, 400 (20.1%) twin births had a planned/elective C/S. In 575 (34.6%) cases both twins were delivered vaginally and in 641 (38.5%) cases both twins were delivered by secondary (unplanned/emergency) C/S. In 47 (2.8%) cases, the first twin was born vaginally, and the second twin by secondary C/S. Of the 575 vaginal twin births, both twins were born spontaneously in 471 (81.9%) and by assisted vaginal delivery in 24 (4.2%) cases. In 53 (9.2%) cases the first twin was born by assisted vaginal delivery while the second twin was born spontaneously, and for 27 (4.7%) twin births this pattern was reversed. Figure 2 shows the proportions of the different delivery modes for twin births per year over time. Overall, there was a significant increase of the proportion of twin births with secondary C/S for both twins over time (n=20, rs=0.605, p=0.005), and assisted vaginal deliveries (n=20, rs=0.6774, p=0.001), while the proportions of twin births with primary C/S (n=20, rs=-0.540, p=0.014) and vaginal birth of both twins (n=20, rs=-0.444, p=0.050) significantly decreased over time.
Same sex twins were observed in 1098 (66.0%) cases, while 564 (33.9%) twin births resulted in a male and a female baby. The median inter twin time for all deliveries was 2 minutes (range 0 - 243 minutes). The average vaginal inter twin time was 16 min/20 years (range 1-243 min/delivery and range 10-21 min/ annually).
In 799 (48.0%) twin births both twins were in cephalic position, in 210 (12.6%) twin births both twins were in breech position, and in 651 (39.1%) one twin presented in cephalic and the other twin in breech position. There were no significant differences among years with regard to the proportions of cephalic and breech presentation of first or second twins (both p>0.35).
There was no significant difference between first and second twins with regard to fetal sex, but second twins presented significantly more often in breech position than first twins (Table 2).
| Variables | First twin | Second twin |
|---|---|---|
| Fetal sex | ||
| Male | 841 (50.6%) | 851 (51.2%) |
| Female | 821 (49.4%) | 812 (48.8%) |
| Unknown | 1 (0.1%) | 0 (0.0%) |
| Fetal position | ||
| Cephalic presentation | 1256 (75.5%) | 995 (59.8%) |
| Breech presentation | 405 (24.4%) | 667 (40.1%) |
| Other | 2 (0.1%) | 1 (0.1%) |
| Fetal weight (g) | ||
| Median | 2365 | 2260 |
| Interquartile range | 1810 - 2730 | 1730 -2660 |
| Range | 410 - 4070 | 270 - 4090 |
| Unknown | 1 (0.1%) | 2 (0.1%) |
| Fetal body size (cm) | ||
| Median | 47 | 47 |
| Interquartile range | 44 - 49 | 44 - 49 |
| Range | 25 - 55 | 24 -55 |
| Unknown | 172 (10.3%) | 178 (10.7%) |
| Fetal head circumference (cm) | ||
| Median | 33 | 32.5 |
| Interquartile range | 31.0 - 34.0 | 31.0 - 34.0 |
| Range | 19.9 - 37.0 | 18.4 - 37.0 |
| Unknown | 204 (12.3%) | 201 (12.1%) |
| Apgar score (1 min) | ||
| Median | 9 | 8 |
| Interquartile range | 07-Sep | 06-Sep |
| Range | 0 - 10 | 0 - 10 |
| Unknown | 57 (3.4%) | 51 (3.1%) |
| Apgar score (5 min) | ||
| Median | 10 | 10 |
| Interquartile range | 09-Oct | 09-Oct |
| Range | 0 - 10 | 0 - 10 |
| Unknown | 101 (6.1%) | 96 (5.8%) |
| Apgar score (5 min)<7 | ||
| No | 1510 (90.8%) | 1485 (89.3%) |
| Yes | 52 (3.1%) | 82 (4.9%) |
| Unknown | 101 (6.1%) | 96 (5.8%) |
| Apgar score (10 min) | ||
| Median | 10 | 10 |
| Interquartile range | 10-Oct | 09-Oct |
| Range | 0 - 10 | 0 - 10 |
| Unknown | 104 (6.3%) | 99 (6.0%) |
| Umbilical cord arterial pH | ||
| Median | 7.31 | 7.28 |
| Interquartile range | 7.26 - 7.34 | 7.23 - 7.32 |
| Range | 6.75 - 7.52 | 6.70 - 7.47 |
| Unknown | 61 (3.7%) | 79 (4.8%) |
| Moderate or severe acidosis (umbilical cord arterial pH<7.10) | ||
| No | -- | -- |
| Yes | 1579 (94.9%) | 1513 (91.0%) |
| Unknown | 23 (1.4%) | 71 (4.3%) |
| 61 (3.7%) | 79 (4.8%) | |
| Umbilical cord venous pH | ||
| Median | 7.35 | 7.33 |
| Interquartile range | 7.32 - 7.38 | 7.28 -7.36 |
| Range | 6.99 - 7.60 | 6.73 - 7.52 |
| Unknown | 317 (19.1%) | 316 (19.0%) |
Table 2: Comparison between first and second twins from 1663 twin births.
The median birth weights of first and second twins were 2365 g (range 410 g-4070 g) and 2260 g (range 270 g-4090 g), respectively. Median birth weight difference between first and second twins was 60 g (range 1260 g–1690 g) and in 674 (40.5%) cases the second twin was heavier than the first-born. Pairwise comparisons revealed that overall first-born twins were both significantly heavier and larger than the second-born. Additionally, first twins had a significantly larger head circumference (Table 2). Birth weights of both first and second twins did not differ significantly over time (p=0.120 and p=0.428, respectively), and there was no significant increase or decrease in birth weight of first or second twins over time (first twins: rs=0.039, p=0.115; second twins: rs=0.044, p=0.074). In contrast, body size and head circumference of both first and second twins differed significantly (all p<0.02) and showed a significant increase over the years (body size first twin: rs=0.054, p=0.036; body size second twin: rs=0.069, p=0.008; head circumference first twin: rs=0.122, p<0.001; head circumference second twin: rs=0.126, p<0.001).
The Apgar scores 1, 5 and 10 minutes after delivery improved significantly over the years for both first and second twins (rs ranging from 0.133-0.206, all p<0.001). This was also reflected by a significant decrease of the proportion of first and second twins that had an Apgar score 5 minutes after delivery below 7 (cochran-armitage test for trend, both p<0.001). Overall, firstborn twins had significantly higher (interpreted as better) Apgar scores 1, 5 and 10 minutes after delivery than their second-born twin siblings; in addition, first-born twins significantly less often showed an Apgar score at 5 minutes below the critical value of 7 compared to second-born twins (Table 2).
Median umbilical artery pH values were 7.31 (range 6.75-7.52) and 7.28 (range 6.70-7.47) for first and second twins, respectively, and median umbilical venous pH values were 7.35 (range 6.99-7.60) and 7.33 (range 6.73-7.52) for first and second twins, respectively. Median umbilical arterial and venous pH increased significantly over the years both for first and for second twins (rs ranging from 0.235-2.95, all p<0.001). Generally first-born twins had significantly higher arterial and venous pH values compared to their second-born twin siblings (Table 2). First-born twins were significantly less often diagnosed with an acidosis (umbilical cord arterial pH values below 7.10 (Table 2).
Looking at the subgroup of 360 to 406 weeks GA (n=821), fetal weight, body size and head circumference showed significant increases (all rs>0.2, all p<0.001 (Figure 3) for fetal weight). However, differences in fetal weight between week 390 and week 406 were small and not significantly different for both first-born and second-born twins (both p>0.2). Umbilical cord arterial pH values differed significantly in the subgroup 360 to 406 for both twins (p-first=0.009, p-second<0.001), with lowest pH values observed for twin births in week 40 (Figure 5).
Umbilical cord venous pH values also differed significantly in this subgroup for the second twins (p<0.001), but not for the first twins (p=0.126). The proportion of twins with umbilical cord arterial pH<7.1 differed significantly for the second twins (p=0.008), but the differences were not significant for first twins (p=0.054) in this subgroup. The proportion of children with acidosis was highest for births in week 400/6 (first twins: 9.5%; second twins: 14.3%; (Figure 4). There were no significant differences among GA weeks 360 to 406 with regard to the Apgar scores 1, 5 and 10 minutes after delivery of the first twin (1 min: p=0.371; 5 min: p=0.111; 10 min: p=0.172). In contrast, the Apgar scores 1, 5 and 10 minutes after delivery differed significantly among GA weeks 360 to 406 for second twins (1 min: p=0.009; 5 min: p=0.004; 10 min: p=0.013). The proportion of newborns with a 5 min Apgar score below 7 did not differ significantly among GA weeks 360 to 406 (pfirst= 0.403, p second=0.5 (Figure 6).
An admission into the pediatric department in this subgroup was noted in 19% of all deliveries over the whole time period, in 19% of the planned cesarean sections and 20% of other delivery modes together. The admission rate in case of a successful vaginal delivery of both twins without assistance was 14% (Ptot=0.134 and Pvag=0.064).
WHO conducted a multinational multicentre questionnaire on maternal and newborn health in 2010-2012. In the participating 29 countries the outcome of twin pregnancies is unfavorable. Worldwide more detailed investigations have been published from several national birth registers, hospitals or reviews. Henry et al. published data to different antenatal clinics. A specialist twin clinic had a cesarean section rate of 55%, late preterm (340-366 weeks) births in 26% and an average birth weight of 2496 g confirming our general expertise over two decades. Similiar benchmarks were published by other authors.
Contributing factors to this improvement are the continuous education of obstetricians, pediatrics and midwifes in hospital and community alongside the technical improvements in the delivery room like ultrasound and electronic fetal heart monitoring. The intrapartum electronic fetal monitoring and ultrasound surveillance help to monitor the fetal ante- and intrapartum situation.
Planned cesarean section was scheduled in the prospective twin birth trial between 375 and 386 weeks but reported an actual delivery age of 370. A newer study showed no difference in neonatal outcome for cesarean section after 370. The prospective JUMODA trial reported the average gestational age in the planned cesarean section group at 356. With nearly 6000 participant this study showed no benefit for the planned cesarean section after 320 gestational ages. The NICE recommendation as per NICE in 2017 concludes therefore that ‘ in otherwise uncomplicated pregnancies at term where the presentation of the first twin is cephalic. CS should not routinely be offered outside a research context’. The guidelines also state that is cephalic, perinatal morbidity and mortality is increased for the second twin. However, the effect of planned CS in improving outcome for the second twin remains uncertain and therefore CS. In our hospital the elective cesarean section is planned at 380+.
Other approaches to reduce this increased risk for the second twin in low risk twin pregnancies have been monitoring and limiting the intertwin time. In Tunis/Algeria a retrospective single center analysis found a time frame of 15 min to be ideal. A recent analysis from Spain showed a decrease in the APGAR and umbilical pH with an intertwin time of more than 10 minutes. The delivery of the second twin within 30 min in nearly 90%. Essential is the close monitoring of the second twin via ultrasound and CTG. A time frame between 20 and 30 minutes was mostly achieved.
But with growing experience in the team this time frame can be extended in reassuring situations and continuous reassessment and may eventually lead to a delayed second twin delivery in premature situations.
Despite these recommendations the rate of unplanned C/S for the second twin is common. Our data confirms these rates over a long time period in a routine clinical setting. This important information needs to be part of the informed consent in order to prevent maternal post-partum feelings of guilt or incompetence. Also it needs to be mentioned that the second twin is more likely to have lower Apgar and pH values. Again our data confirms this finding but also shows the improvements over the last two decades made in the team and the reduced clinical relevance of these findings [12-15].
This can be due to our standard offer to mothers-to-be in our hospital to proceed with a trial of vaginal delivery for diamniotic twins when the first twin is in vertex presentation. Should the parents after informed consent opt for an elective C/S, the first twin present non-vertex or a C/S is recommended the surgery is planned in the 380/6 or beginning of the 39th week GA in uncomplicated pregnancies [16-21].
Currently good evidence data for the 'ideal' GA week for a vaginal birth trial is missing.
Leveno hypothesize that twins experience earlier pulmonary maturation than singletons [22]. Twenty years later Martilla showed a significant risk of respiratory distress in preterm twins [23]. Antenatal corticosteroids to enhance fetal lung maturation may be indicated in selected preterm twin deliveries.
A consensus statement from a workshop held by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Society for Maternal-Fetal Medicine (SMFM) suggested that, in the absence of a spontaneous birth, delivery should be induced at 380 weeks for uncomplicated dichorionic twin pregnancies and 340 to 370 weeks for uncomplicated monochromic diamniotic twin pregnancies.
The lowest perinatal mortality for twin pregnancy appears to be between 370 to 380 weeks GA. Our antenatal outcome parameters for all twin deliveries that occurred between 360 and 400 weeks GA, showed the highest Apgar scores for second twins born between 370 and 380 weeks GA with no differences for the first-born twin. Though this analysis is based only on retrospective data it supports the consensus recommendation [24-29].
Though the database provides very detailed information on the delivery it is not possible to draw clinical conclusions from our results as these need to be evaluated in prospective randomized trials. On the other hand are prospective obstetric trials difficult to get ethical approval and further the difficulty of recruiting patients willing to participate. With these limitations a retrospective analysis of a sufficient large database may be the clinical compromise to base the informed consents with our patients on.
Twin pregnancy remains a high-risk obstetrical situation. The management of twin pregnancies in the antenatal and intrapartum period should be done by health care professionals with appropriate training in high risk obstetrics. Appropriate antenatal monitoring and care at delivery is vital. The optimal mode of delivery of twins is still a subject of continuing debate. Our data suggests that a trial of vaginal birth is an option for women with diamniotic twin pregnancies with the leading twin in cephalic presentation and a well-trained obstetrical team.
The local ethics committee waived the need for approval. Patients consented to provide data for auditing and quality improvement purposes.
Not applicable
The datasets generated and analyzed during the current study are not publicly available due the detailed patient information but are available from the corresponding author on reasonable request. But restrictions may apply to the availability of these data.
The authors declare that she has no conflict of interest.
No funding for this analysis was received by any of the authors
AS, TWPF, NDG analyzed the data; FR, AP corrected the draft; WJ, FE drafted the article; AS, FE wrote the article; FE, NDG collected the data. All authors have read and approved the manuscript
The authors would like to thank the obstetrical teams of the last two decades. Their continuous efforts to improve patient care and documentation made this study possible.
This retrospective study was conducted as a quality control of the obstetrical department. The patients consent for quality improvement and outcome analysis is given in written by signing into the department. The local ethics commission had been consulted before the data was retrieved. A ethic votum was not necessary according to supplement 10 of the ethics commission.
Informed consent for participation in the retrospective study was not required as the analysis used anonymized data obtained after the patients had agreed to treatment by written consent.
The authors have no conflicts of interest to disclose.
Citation: Stoenescu A, Friedl WPT, De-Gregorio N, Reister F, Polasik A, Janni W, et al. (2020) A Single-Center Cohort Study on 1663 Twin Birthsfrom Two Decades: A Descriptive Statistics and General Trends. Gynecol Obstet (Sunnyvale) 10:520. doi: 10.35248/2161-10932.2020.10.520
Received: 19-Feb-2020 Accepted: 20-Feb-2020 Published: 27-Feb-2020 , DOI: 10.35248/2161-10932.20.10.520
Copyright: © 2020 Stoenescu A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.