Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2019)Volume 9, Issue 3
Mumps is a childhood disease with declining incidence in the western world and arthritis is a rare complication associated to the disease. Various presentations exist making diagnosis even more challenging. The mechanisms responsible for the joint involvement remain largely unknown but the timing of onset of the symptoms usually coincide with the rise in antibody titers arguing for an immunologic mediated response. We hereby report a rare case of polyarthritis in the onset of epididymoorchitis due to mumps infection in a HIV infected male patient. Elevated IL-6 serum level in our patient suggests that this cytokine may be an interesting biomarker for the diagnosis of mumps related arthritis.
Mumps; Polyarthritis; HIV; IL-6
Mumps is a childhood disease caused by Myxovirus parotidis, a single stranded RNA virus of the paramyxovirus family [1,2]. Before vaccines were available in 1960s a worldwide incidence of 100-1000 cases/100000 was reported. The incidence then dramatically decreased in areas with high vaccination rate although some outbreaks still occur [3,4]. Mumps typically causes parotid swelling and pain, fever and headache. Common complications includes meningitis, orchitis and deafness [3,5]. Other complications such as post-infectious encephalomyelitis and type 1 diabetes are linked to the development of an autoimmune reaction in response to the virus [6,7]. Arthritis is a rare complication linked to direct joints damage by the virus or to immune complexes deposition in the joints [8,9] In this paper, we report the case of a patient who developed diffuse polyarthritis in the onset of epididymoorchitis due to mumps infection.
We report the case of a HIV infected middle-aged man, originating from Eastern Africa and residing in central Europa who was admitted to hospital for a recent onset of high grade fever, diffuse myalgia, testicular pain and polyarthritis. One week prior to admission, based on clinical evaluation and urine examination, he was treated for a suspicion of epididymoorchitis and prostatis. Despite antibiotics treatment, the symptoms worsened and the patient was admitted to hospital for further investigation.
His medical history was remarkable for HIV infection on antiretroviral treatment (doravirine, tenofovir disoproxil and lamividune) with undetectable HIV viral load and high CD4 cell count. On physical examination, the patient showed a tympanic temperature of 39.5º associated to diffuse polyarthritis involving both knees, wrists, shoulder and bilateral metacarpophalangeal joints. Initial blood test demonstrated an elevated C-reactive protein at 202 mg/L (reference, <10 mg/L) and erythrocyte sedimentation rate at 62 mm/h (reference, <20 mm/h). Blood, synovial fluid and urine cultures remain sterile. Urine PCR testing for Chlamydia trachomatis and Neisseria gonorrhoeae were negative. Chest X ray was unremarkable. Tenosynovitis of right and left wrists was confirmed by ultrasound imaging.
Development of polyarthritis in a middle-aged HIV treated patient opens a wide differential diagnosis that includes autoimmune, infectious and crystal joint disorders. In HIV infected patients, diagnostic and management of arthritis is challenging. As compared to uninfected population, autoimmune arthritis is more frequent among HIV treated individual with undetectable viremia and normal CD4 count [10]. Autoimmune disorders during HIV infection are related to the development of autoantibodies and auto-reactive cells, through chronic activation of the immune system in response to sustained antigen stimulation and through the molecular mimicry between the virus and the host [11,12]. An association has been described between HIV infection and diseases that may affect the joints such as seronegative spondylathropathy, rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, sarcoidosis and vasculitis [11,13].
Infectious arthritis should also be considered in the differential diagnosis. Virus can initiate joint symptoms through various mechanisms including direct invasion, immune complex formation and persistent infection that can target the immune system. Most frequent germs involved in infectious arthritis are HIV itself, hepatitis B and C viruses, Epstein-Bar virus and parvovirus B19. Certain bacteria, including Borrelia burgdorferi, can trigger oligo- or polyarthritis than can mimic inflammatory arthritis.
Based on the clinical history and presentation, additional tests were performed to further investigate the origin of the polyarthritis. Rheumatoid factor, anti-cyclic citrullinated peptide (anti-CCP), antibody and anti-nuclear antibodies were negative. Complement components C3C and C4 were not reduced. Inflammatory cytokine profile was measured based on a Luminex xMAP technology using a sandwich ELISA approach (ProcartaPlex, Thermo Fischer, Switzerland) and, interestingly, showed an important elevation of interleukin (IL)-6 (Figure 1). Some other pro-inflammatory cytokines were also slightly augmented. Serologic tests for Syphilis, Lyme disease and Brucellosis were negative. Serologic test for mumps was positive for the detection of IgM at 2.0 (reference, 0.5-1) and IgG at 3.28 (reference, 0.35-0.5). To confirm the diagnostic of acute mumps infection, anti-mumps IgG was also measured in a frozen sample that was collected one year prior to current investigations and showed an IgG level of 0.04. In light of this clinical workup, we concluded that the patient suffered from a polyarthritis in the onset of an epididymoorchitis related to mumps virus infection. Therapy with glucocorticoid (Prednisolone 20 mg/day, tapered over 2 weeks) was initiated and the patient showed a rapid improvement of symptoms, without recurrence after therapy discontinuation.
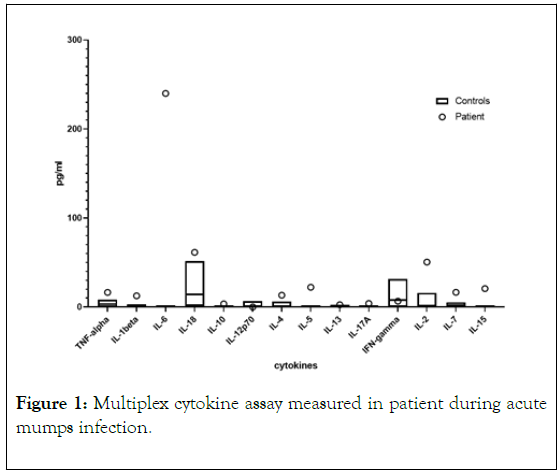
Figure 1. Multiplex cytokine assay measured in patient during acute mumps infection.
In this case, the patient developed polyarthritis after epididymoorchitis related to Myxovirus parotidis infection. Development of polyarthritis following mumps infection is a relatively rare complication that was described for the first time by Rilliet in 1850 [14]. In 1984, Gordon et al. published a review about 32 cases of mumps arthritis [8]. Since the implementation of routine vaccination, there has been a massive decline in mumps infection that explains why only few additional cases were reported in the past few years [15-17] However, the Seroprevalence of Mumps and other childhood disease remain low among HIV-positive immigrants [18].
Mumps arthritis can occur before, during or without parotitis [8]. Males are more often affected than female with a male to female ratio 3.6:1. Moreover, patients who develop arthritis tend to be older than those with uncomplicated mumps infection [8]. Most patients with mumps arthritis present extra salivary manifestation of the disease, epididymoorchitis being one of the most frequent associated condition [8,19]. Three different clinical forms of mumps arthritis have been described: arthralgia without clinical signs of inflammation, polyarthritis, which is often migratory, and mono-articular arthritis [8]. Symptoms duration is highly variable, but self-limited without description of permanent joint damage. Treatment with a short course of systemic steroids leads to a quick improvement in most case [8]. In our case, the patient first presented diffuse arthralgia that subsequently evolved into frank symmetrical polyarthritis and was associated with an important systemic inflammation.
The mechanisms responsible for joint involvement by mumps remain largely unknown. The main hypotheses include direct synovial infection by the virus itself or immune mediated response linked to immune complex deposition.
In vitro study showed that the virus could infect and even persist for two to three months in synovial cells, suggesting the possibility of direct damage and pro-inflammatory effect by the virus to the joint synovial tissue [20]. However, to date there is no description of Myxovirus parotidis isolation from the synovial fluid of patients suffering from mumps arthritis.
In the review by Gordon and al., seventy-two percent of the patients developed arthritis between one and three weeks after parotid glands involvement or after symptoms of non-specific viral illnes [8]. This timing coincides with the rise in antibody titers arguing for an immunologic mediated response [8]. Nevertheless, no immune complex deposits have been detected so far in the joints of patients suffering from mumps arthritis [21]. In our patient, complement factors C3C and C4 levels reduction, which would have been an argument for immune complex deposition, was not present.
Multiple cytokines assay showed an important elevation IL-6, compared to other detected cytokines (Mainly TNFa, IL1, IL-2, Il-4, IL-5, Il-7, IL-15, IL-18), which were only slightly elevated (Figure 1). IL-6 is produced by a broad spectrum of cells, including innate immune cells, such as macrophage and monocytes [22]. Only a few studies have evaluated peripheral blood cytokines during acute mumps infection and have mainly shown an elevation of T helper (Th) -1 cytokines, such as IFN γ [23,24]. In addition, one study found an elevation of IL-6 in a series of Chinese acute mumps-infected patients at levels below those observed in our case and without correlation between IL-6 levels and mumps-related organ complications [24]. Despite limitation inherent to a case report, our data suggest that IL-6 may be an interesting biomarker for the diagnosis of mumpsrelated arthritis.
To our knowledge, this is the first reported case of mumps arthritis in a HIV infected patient. The role of HIV infection in the development of mumps arthritis is unknown. Overall, the onset of immune complex and reactive arthritis of any origin is more prevalent in HIV infected patients, even with undetectable viremia and normal CD4 count. However, no specific data are available in the context of Myxovirus parotidis infection and further studies are needed to understand how mumps and HIV co-infection interact.
In immigrant populations, the onset of arthritis or arthralgia should prompt the search for mumps infection, especially if other suggestive clinical symptoms are present.
The authors have declared that no conflict of interest exists.
Citation: Van Singer M, Felix N, Perreau M, Lebowitz D, Comte D (2019) A Rare Case of Diffuse Polyarthritis in the Context of an Epididymoorchitis due to Mumps Infection. Rheumatology (Sunnyvale). 9:257. DOI: 10.35248/2161-1149.19.9.257
Received: 10-Dec-2019 Accepted: 24-Dec-2019 Published: 31-Dec-2019 , DOI: 10.35248/2161-1149.19.9.257
Copyright: © 2019 Van Singer M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.