Journal of Pharmaceutical Care & Health Systems
Open Access
ISSN: 2376-0419
ISSN: 2376-0419
Research - (2019)Volume 6, Issue 2
Background: Clinical pharmacy services are patient oriented services developed to promote the rational use of medicines by maximizing therapeutic effect of medicines in individual patients. It has a positive impact on medical, economic and humanistic outcomes of the patients. In Ethiopia, the service is at its infant stage and there is lack of objective evidence on the strength, weakness, opportunity and threats. Therefore, the aim of this study was to undergo situational analysis of clinical pharmacy services in Tirunesh Beijing General Hospital using SWOT frame work.
Methods: A qualitative study was conducted in Tirunesh Beijing General Hospital from March 1 to March 14, 2016. An in-depth interview with flexible probing techniques was designed to collect the data from twenty key informants. A semi structured interview guide was prepared to explore ideas of key informants about situation of clinical pharmacy service, internal factors (strength & weakness), and external factors (opportunity & threats). A thematic analysis was then used to analyze the data.
Results: Internal factors such as presence of clinical pharmacists in the hospital and interest & willingness of the managers to support and give assistance to the services were found as the major strengths, while lack of adequate facilities & equipment; poor performance of clinical pharmacists in implementing the service; poor collaboration working relationship between the pharmacists and physicians and weak evaluation mechanism of the hospital management were found as the major weaknesses. External factors such as increasing number of graduating clinical pharmacists from different colleges and universities and availability of post graduate program in clinical pharmacy in the country were identified as opportunity. However, low coverage of promotion about the service by the responsible body was mentioned as threat for the hospital.
Conclusion: The study identified that clinical pharmacy services had a lot of limitations as compared to its strengths in the hospital. It is recommended that the hospital should expand and implement the service in all wards and facilitate experience sharing programs with other model hospitals in clinical pharmacy to strength the service.
Clinical pharmacy services; SWOT analysis; Tirunesh Beijing hospital
DTC: Drug and Therapeutic Committee; SWOT: Strength Weakness Opportunity and Threat; TBGH: Tirunesh Beijing General Hospital.
Pharmaceutical services are an essential component of health care service. Effective pharmaceutical services promote the safe, rational and cost-effective use of medicines thus maximizing health gain and minimizing risk to patients. A well-organized pharmaceutical service ensures the continuous availability of all pharmaceuticals that are required for patient care. At the same time, an effective pharmaceutical service should be able to respond to sudden increases in medicine demand, ensuring that adequate supplies are available to deal with any emergencies that arise [1]. The pharmaceutical service is undergoing a paradigm shift from product-oriented to patient-oriented service. Traditional role of the pharmacist that involving the preparation, dispensing and selling medications is shifted to the new clinical pharmacy services that practitioners not only dispense medications, but also assume responsibility for improving the quality of patients’ outcomes [2]. The service was started in the United States, and is now available in many parts of the world [3].
Clinical pharmacy requires an expert knowledge of therapeutics, a good understanding of disease processes and knowledge of pharmaceutical products. In addition, it requires strong communication skills with solid knowledge of the medical terminology, drug monitoring skills, provision of medicines information, therapeutic planning skills and the ability to assess and interpret physical and laboratory findings [4].
The positive impact of clinical pharmacy services on medical, economic and humanistic outcomes has been demonstrated in numerous studies [5]. For instance, ten to thirty percent of all acute hospital admissions are thought to be caused by medicine related problems and 50-70% of these are considered to be preventable by effective implementation of clinical pharmacy services [6]. For every dollar spent by hospitals or health systems to provide clinical pharmacy services, $4.81 was saved through lower medicine costs, reductions in adverse medicine events and medication errors and other savings [7].
Despite this, there is much variability between countries in the practice and implementation of clinical pharmacy. The practice is still in its early stages, in developing countries [5]. In these countries, implementation of clinical pharmacy service still encounters a number of hurdles, among which are time constraints, absence of recognized reimbursement system, unavailability of appropriate space, less access to patient medication record, insufficient number of competent pharmacists, and shortage of standard practice strategy [8].
The Ethiopian situation is not different from the rest of the developing world. The country has a large, predominantly rural, and impoverished population with poor access to safe water, housing, sanitation, food, and health services. These factors result in a high incidence of communicable diseases including TB, malaria, respiratory infections, diarrheal diseases, and nutritional deficiencies. The country is characterized by an inadequate number of well-trained health providers, limited health infrastructure, inadequate space, shortages of equipment and commodities at health facilities and weak health systems which results in low service utilization [9]. In addition to resource related challenges, the effect of limited number and quality of pharmacy personnel on the provision of health care in Ethiopia is prominent [10].
A number of different techniques can be used to determine where health care organization adjustments need to be made. One essential technique involves a discussion of an organization’s strengths, weaknesses, opportunities, and threats, commonly called SWOT analysis [11]. SWOT analysis is a tool used in the preliminary stages of decision making and as a precursor to strategic planning [12]. It requires the specification of the objectives inherent to the service under study and the identification of the internal and external factors, both favorable and unfavorable to achieve the proposed goals [13]. The objective of the internal analysis in a SWOT analysis is to identify the main Strengths and Weaknesses that characterize an organization, in a precise moment. On the other hand, the external analysis intends to identify the main Opportunities and Threats [13]. The most important parts of a SWOT analysis are its ability to specify the actions that correspond to the elements we identify as well as improving the viability of our health care organization [14].
Within the Ethiopian Health Service a number of reforms are currently taking place that affect hospital pharmaceutical services; and clinical pharmacy service is the one introduced within the nation’s health-care system in order to improve patients’ quality of life and medicine use [1]. Analysis of strengths, weaknesses, opportunities and threats is a crucial step in the planning process of this new services and evaluating its implementation.
Over all, since clinical pharmacy service is at the infant stage in Ethiopia, there is lack of objective evidence on the strength, weakness, opportunity and threats.
In Tirunesh Beijing Hospital most drug therapy decisions are made by physicians and pharmacist’s role is more reactive; (i.e. responding to prescribing errors long after the decision has been made, and without having direct clinical knowledge of the patient). In addition to these there is less frequent/no Pharmacists-physicians’ interaction and most of the Pharmacists practicing in the hospital fail to recognize themselves as member of the health care team results in huge gap in delivering the prospected quality clinical pharmacy service to patients.
Hence, assessing the strengths, weaknesses, opportunities & threats of the service in order to make further improvements in the areas where gaps are seen and to strengthen the areas in which it is good at is crucial. Therefore, the aim of this study is to undergo situational analysis of clinical pharmacy services and identify the strengths, weaknesses, opportunities & threats of Tirunesh Beijing General Hospital using SWOT frame work.
A qualitative study was conducted in Tirunesh Beijing General Hospital from March 1 to March 14, 2016. The hospital is located in Akaki -Kality sub city of Addis Ababa, the capital of Ethiopia. The hospital was inaugurated in May 2009 and it has started service since February 2012. The hospital has 114 beds & gives services for about 1.5 million people from Addis Ababa city administration and near Oromia special zone. The hospital has 461 Employees of which 146 were administrative workers and the rest 315 were health professionals. The hospital provides both diagnostic &medical as well disease prevention &control services which are categorized in to outpatient, inpatient, and emergency department. The service includes ophthalmology, psychiatry, physiotherapy, laboratory, pharmacy, radiotherapy, minor surgery, gynecology, Antenatal care, Orthopedics & pediatrics services and clinical pharmacy service was implemented in the hospital in 2013/14.
An in-depth interview with flexible probing techniques was designed to collect the data from twenty key informants. 8 General practitioners, 8 Clinical Pharmacists, Matron nurse, Medical director, Chief executive officer and the head of pharmacy department of the hospital were purposively identified as key informants based on their ability to address issues on clinical pharmacy service in the hospital. A semi structured interview guide was prepared to explore ideas of key informants about situation of clinical pharmacy service, internal factors (strength & weakness), external factors (opportunity & threats) and efforts in preventing or minimizing the weakness and threats. The interview guide was developed after literature search [5,10-14]. And it was tested for its face and content validity by two experts from social and administrative pharmacy group. The interview guide was prepared in the English language, and translated into Amharic and then to English to check message consistency. The Amharic version was used for the interview with key informants. The data was collected by two pharmacists and it was cross validated by the two experts. The data analysis involved an intensive reading through the interview in order to identify key themes. Audio-recorded interviews were transcribed verbatim and the raw data was categorized under pre-developed coded themes and sub themes. A thematic analysis was then used to analyze the data.
Ethical approval was obtained from the Head Department of Pharmaceutics and Social Pharmacy, School of Pharmacy, Addis Ababa University and from the hospital. Besides, a verbal consent was obtained from all participants before starting the interview. Confidentiality and anonymity of information was maintained throughout the data collection and analysis period by not linking personal identifiers in the data presentations.
Hospital pharmacy service
The hospital had Outpatient, Inpatient, Emergency pharmacies and a central medical store each directed by a registered pharmacist. It provides medicine dispensing & counseling service; drug information service; clinical pharmacy service and medicine supply and distribution service. The hospital also has Drug and Therapeutic committee (DTC) and prepared a medicine formulary list (Figure 1).
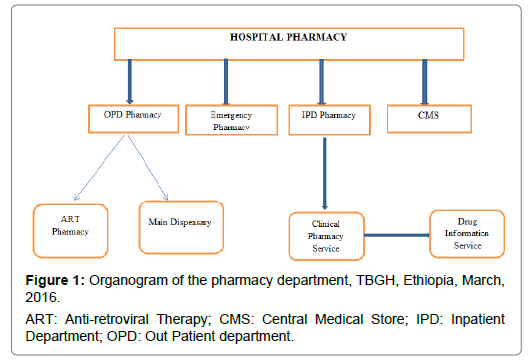
Figure 1: Organogram of the pharmacy department, TBGH, Ethiopia, March, 2016.
SWOT of clinical pharmacy services in hospital
In-depth interviews were held with general practitioners, clinical pharmacists, matron nurse, medical director, chief executive officer and head of pharmacy department of the hospital (a total of twenty) to gather information about the strengths, weaknesses, opportunities and threats (SWOT) to clinical pharmacy services of the hospital. 15 of the key informants were males and the remaining 5 were females. Majority of them were in the age group of 25 to 35 (30.9 ± 5.9) years with bachelor degree. The work experiences of the respondents ranged from 1 to 12 (5.1 ± 2.8) years.
Strength and weakness
Several internal factors for clinical pharmacy service of the hospital were mentioned by the key informants and four key themes were emerged in order to identify the strengths and weaknesses in the hospital. Key themes to emerge were: Human resource; premises, facilities & equipment; performance of clinical pharmacists and organizational management and quality improvement.
Human resources
The key informants were asked if the number of trained pharmacists is enough to provide clinical pharmacy services in the hospital and the response of all (including the clinically trained pharmacists) were yes. The main reason for this was the perception that clinically trained pharmacists give services limited to wards. Currently they were attached and provided the service in medical ward only. The service was given usually at morning during round time with physicians and occasionally at afternoon when the service was needed (Table 1).
| Factors | Strength | Weakness |
| Human resources | Presence of clinically trained pharmacists in the hospital Distribution of job description for pharmacists Delegation of clinically trained pharmacist in the hospital DTC Low attrition rate of clinical pharmacists as compared to other health professionals in the hospital. | Absence of supportive staffs for clinical pharmacy services. Lack of experience Shortage of pharmacists for other pharmaceutical service areas. Absence of dedication to provide the service on full-time basis. Weakness of the pharmacists to promote their profession and duties to the hospital staffs. |
Premises, facilities & equipment
Regarding premises and facilities, all the key informants mentioned that there was no separated pharmacists’ office, duty room and counseling booth in addition to the ward rooms for clinically trained pharmacist. They practiced all of their activity at bed sides in the medical ward. The respondents also revealed telephone, internet, computers and filing cabinets used for clinical pharmacy services were not adequately available in the hospital. But the accessibility of water, electric supply and separate toilet with adequate water supply for the clients and staffs were good (Table 2).
| Factors | Strengths | Weakness |
|---|---|---|
| Premises, Facilities & Equipment | Adequate accessibility of electricity and water supply in the hospital Availability of separate toilets with drainage system for staffs and clients Majority of the facilities and equipment including books required for drug information center were available. | Absence of separate pharmacists’ office and counseling booth in the ward. Inaccessibility of telephone & internet facility for clinical pharmacy services Lack of adequate furniture, filling cabinets, computer & other equipment required for clinical pharmacy services Inappropriate site of drug information center in which clinical pharmacists provide medicines information to the staffs. |
Table 2: Identified strengths and weaknesses of clinical pharmacy services in terms of premises & facilities in TBGH, Ethiopia, March, 2016.
Current performance of clinical pharmacy providers in the hospital
Regarding the current practice of clinical trained pharmacists in the hospital, all key informants (Physicians, matron nurse & CEO) said the performance of the pharmacists in practicing clinical pharmacy in the hospital was poor. However, all clinically trained pharmacists expressed their activity as they were practiced the service in medical ward only and they were actively participated in ward rounds with the health care team and in morning session with all staffs. They also said that the provision of drug information for physicians and other health professionals was made when the service is requested by the professionals and in the same way other services like information on appropriate route of drug administration, side effect prevention and management, dose calculation for patients and the like were provided when the service is needed (Table 3).
| Factors | Strengths | Weaknesses |
|---|---|---|
| Current performance /service delivery | High involvement of clinical pharmacists in identifying and reporting adverse drug reaction & obtained recognition letter from Ethiopia Food Medicine Health care Administration and Control Authority. | The service is limited in medical ward Poor collaboration between clinical pharmacists and physicians Communication barriers between pharmacists , physicians & hospital management Low frequency of interaction between physicians and pharmacists Absenteeism of pharmacists in their working area. |
Table 3: Identified strengths and weaknesses of clinical pharmacy services in terms of current performance in TBGH, Ethiopia, March, 2016.
Management and quality improvement practice for clinical pharmacy services in the hospital
All key informants agreed that no management and quality improvement activity was taken by the hospital management/board to strength the clinical pharmacy services and the monitoring and evaluation mechanisms were weak. According to the respondents no policies and procedures were established to improve the quality of the services. The performance of the clinical pharmacists was not evaluated and customer satisfaction survey on pharmaceutical care services was not conducted (Table 4).
| Factors | Strengths | Weaknesses |
|---|---|---|
| Organizational management and quality improvement | Interest & willingness of the managers to support and give any required assistance to the services in the future. Recognition & understanding the weakness of the service by the management and establishing a committee that reorganize the hospital pharmacy and follow the service provision to solve the current problem. | Weak evaluation mechanism Lack of support from administration/management Lack of standard operating procedures Unavailability of pharmaceutical care tools Absence of documentation of their activities by clinical pharmacists. |
Table 4: Identified strengths and weaknesses of clinical pharmacy services in terms of quality improvement practice in TBGH, Ethiopia, March, 2016.
Opportunity and threats
Several external factors were mentioned by the key informants as opportunities and threats for clinical Pharmacy services in the hospital. Increasing number of graduating clinical pharmacists from different colleges and universities and availability of post graduate program in clinical pharmacy were among the opportunities mentioned by the key informants (Table 5).
| Opportunity | Threats |
|---|---|
| Presence of model facilities on clinical pharmacy services in the country Increasing number of graduating clinical pharmacists from different colleges and universities Availability of post graduate program in clinical pharmacy Presence of national DIC center Presence of strong professional association Presence of scope of practice for clinical pharmacy Good commitment of the government to improve the quality of health care. | Misperception of physicians, other health professionals and administrative officials about the current role of clinical pharmacists Inadequate external monitoring and evaluation mechanism Lack of attention by the government and stake holders about the service Low coverage of promotion about clinical pharmacy service by the responsible body. |
Table 5: Identified external factors (opportunities and threats) of clinical pharmacy services in TBGH, Ethiopia, March, 2016.
This assessment has attempted to identify the strength, weaknesses, opportunity and threats of clinical pharmacy services of Tirunesh Beijing Hospital.
Majority of the health professionals (including clinically trained pharmacists & physicians) in the hospital were found from the age groups 25-30 years and their experience is less than 3 years, the main reason for this is the hospital was established earlier & most of the recruited professionals were fresh graduate. Indirectly it also indicated that clinical pharmacy services in Ethiopia is at infant stages. This has its own advantage for the hospital because evidence shows that more collaborative working relationship is established between young professionals than old professionals in health care team [15].
Regarding the number of clinical pharmacists in the hospital, all respondents agreed that there number is not adequate to give the services in the hospital. Similarly, a study done in Pakistan found that hospital pharmacists working in hospitals are very less in number to make the implementation of the pharmaceutical care services possible [16] and more recent researches from developing countries shows that increased clinical pharmacist staffing has been shown to result in enhanced patient outcomes by engaging in medication safety activities in hospitals [17].
All of the clinical pharmacists found in the hospital were provide dispensing services other than pharmaceutical care services. They were involved in dispensing of medicines at outpatient, inpatient, ART and Emergency pharmacies. The reason mentioned for this was shortage of pharmacists and druggists in other pharmaceutical services which brings gap to the clinical pharmacy services and absenteeism of the clinical pharmacists in their working area. This finding is in contrast with many studies done on this area in which, regardless of where pharmacists work in the hospital, clinical pharmacists should engaged in providing drug information, drug therapy evaluation, drug therapy intervention, and pharmacokinetic monitoring, medication reconciliation in geriatrics, review medication orders in emergency department and managed antimicrobial prophylaxis in surgical site [18].
The hospital pharmacy gives clinical pharmacy services limited to medical ward. The service was started in pediatrics ward but due to fewer acceptances of physicians working in the ward it is stopped and the services not yet started in other wards like surgical ward of the hospital. But evidences from previous studies have reported the contribution of clinical pharmacists to patient care in a variety of clinical settings like intensive care and pediatrics/specialty wards, internal medicine ward, immunology/hematology and neurology and many specialist clinical units such as neonatal critical care and oncology have relied on pharmacist participation during clinical rounds in order to resolve issues of adverse drug reactions, drug interactions and medication errors associated with complexity of medical conditions and medication regimens used in these units [18].
Different internal factors were mentioned by the key informants under the theme of current clinical pharmacy services in the hospital. Lack of active communication skill of clinical pharmacists, Absenteeism of pharmacists in their working area, Low acceptance level of physicians, Low frequency of interaction between physicians and pharmacists and poor collaborative working relationship between the two professions were the main reasons for limitation of current clinical pharmacy services in the hospital. This relatively revealed similar result with study done in hospitals of Kuwait, where the study participants indicated that the anticipated problems that may delay the implementation of pharmaceutical care in their practice were lack of time, lack of staff, lack of training, lack of resources, lack of communication skills, lack of knowledge and others including lack of patients and physicians trust on the ability of pharmacists [5]. This idea is also justified by other findings. However, there is a lack of information in relation the implementation of pharmaceutical care services in developing countries and its value. Barriers that impede the implementation of pharmaceutical care in a variety of settings were found to include attitudes of pharmacists, lack of pharmacists’ advanced practice skills, resource-related constraints, system-related constraints, and educational obstacles [19].
Lack of communication skills is most predominantly mentioned by all key informants other than clinical pharmacists as the main factor for the limitation of clinical pharmacy services in the hospital. Similarly evidences shows that poor communication skill is also a problem among clinical pharmacists. It is a big issue in patient centered care because ineffective communication skill makes exchange of information and building a trusting and ongoing relationship with patients and health care professionals to be difficult. Communication barriers between pharmacists and physicians results less collaboration between the two professions [15].
Regarding to monitoring and evaluation of the service, no policies and procedures were established by clinical pharmacists together with hospital DTC to improve the quality of the services. The performance of the pharmacists was not evaluated and customer satisfaction survey on pharmaceutical care services was not conducted. The main reason mentioned for this was the focus of the hospital DTC as well as stake holders working with the pharmacy service of the hospital are the drug supply management part/filling the gaps in supply of pharmaceuticals rather than strengthening clinical pharmacy services. According to Ethiopian Hospital Reform Implementation Guideline the role and responsibility of DTC includes establishing mechanisms to identify and address drug use problems, and oversee the drug use service in addition to involved in drug supply management parts [1].
All of the clinical pharmacists (n=8) mentioned that they did not record and document their activities and no registration and documentation that showed the service provided by clinical pharmacists in patient care was available. This result unable to know different indicators like the number of recommendation made and accepted by pharmacists and physicians, and the like which are also important to understand the level of their performance. Lack of documentation also refers the clinical pharmacists did not practiced all activities expected from them in which clinical pharmacists should document directly in the patient’s medical record the medication-related assessment and plan of care to optimize patient outcomes. This documentation should be compliant with the accepted standards for documentation within the health system, health care facility, outpatient practice, or pharmacy in which one works. Where applicable, accepted standards must be considered as they relate to the use of electronic health records, health information technology and exchange systems and e-prescribing [20].
The presence of established clinical pharmacy service in the hospital and interest & willingness of the managers to support and give assistance to the services were found as the major strengths, while lack of adequate facilities & equipment, poor performance of clinically trained pharmacists in implementing the service, poor collaboration working relationship between the pharmacists and physicians and weak evaluation mechanism of the hospital management were found as the major weaknesses of clinical pharmacy service in the hospital. Besides these external factors such as increasing number of graduating clinical pharmacists from different colleges and universities and availability of post graduate program in clinical pharmacy in the country were identified as opportunity for the hospital. However, low coverage of promotion about the service by the responsible body rose as threat. It is recommended that the hospital should make adequate facilities and equipment available at clinical pharmacy services; put standard operating procedures in place to guide the implementation of the service and should facilitate experience sharing programs with other model hospitals in clinical pharmacy service to strength the service in its own hospital.
The authors would like to acknowledge all study participants and individual who provided information. Our special thanks to Ato Gelana Gudeta, Ato Tsegaye Ababiya, Ato Alemayehu Negash and Dr. Tilahun Getaneh of Tirunesh Beijing Hospital for their cooperation. We are also grateful to Addis Ababa University, School of Pharmacy, Department of Pharmaceutics and Social Pharmacy staffs for facilitating this research.
The authors of this manuscript declare that they have no competing interests.
Citation: Gebremariam ET, Mekuria B (2019) A Qualitative Review of Strengths, Weaknesses, Opportunities and Threats of Clinical Pharmacy Services Provided by Tirunesh Beijing General Hospital. J Pharma Care Health Sys 6:206. doi:10.4172/2376-0419.1000206
Received: 02-Feb-2019 Accepted: 24-May-2019 Published: 31-May-2019
Copyright: © 2019 Gebremariam ET, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.