Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2019)Volume 9, Issue 2
Osteonecrosis (ON) or avascular necrosis results from disruption of blood supply to bone marrow and trabecular bone leading to death of bone. Antiphospholipid Syndrome (APS) may be primary or secondary to other autoimmune disease. The involvement of multiple sites of ON has been documented with APS. Literature suggests that avascular necrosis predispose a septic arthritis in affected joints especially in immunosuppressed patients.
Osteonecrosis; Bone; Joint; Arthritis
A 29-year-old male patient was a heavy smoker with a past medical history of NSAID abuse and antral and duodenal ulcers. He admitted to the hospital with a sudden severe pain on the medial side of right knee associated with erythema and fever.
Patient diagnosed as a septic arthritis of the knee by joint aspiration and cytology. The aspirate culture revealed methicillin resistant Staphylococcus aureus (MRSA) and he started antibiotics. MRI of the right knee showed multiple bone infraction, synovitis, joint effusion, grade 1 medial collateral ligament (MCL) sprain (Figure 1).
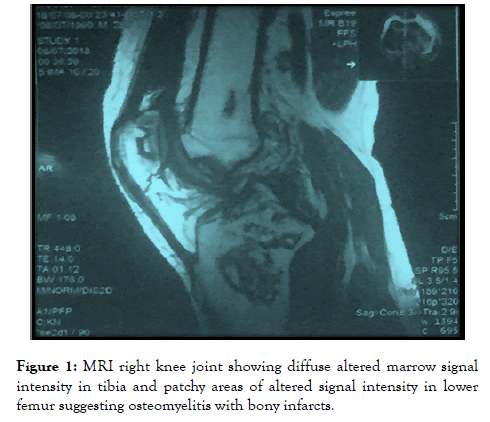
Figure 1. MRI right knee joint showing diffuse altered marrow signal intensity in tibia and patchy areas of altered signal intensity in lower femur suggesting osteomyelitis with bony infarcts.
He sought an orthopedic advice with surgery for bone biopsy and debridement of necrotic bone tissue. After 2 days of surgery, patient`s condition was deteriorated and admitted to intensive care with septic shock and disseminated intravascular coagulation. Laboratory investigation showed leukocytosis with high acute phase reactant (ESR&CRP).
Bone biopsy showed low grade inflammation collagenized vascular stroma with adjoining necrotic bone tissue neither malignancy nor typia. After a while, he transferred to the ward after controlling the sepsis with antibiotics and steroid.
Then, he went to home but he developed severe right knee pain, erythema associated with limitation of movement. One month later, he developed bilateral hip pain more on left side and knee pain progressed to knee effusion. MRI of both hip revealed bilateral femoral head avascular necrosis, more on left side.
Bilateral core decompression osteotomy was done but without significant improvement (Figure 2). Two months later, he developed bilateral ankle pain more on right side and MRI of right ankle joint showed multiple bone infraction at tibial plafond and talar dome.
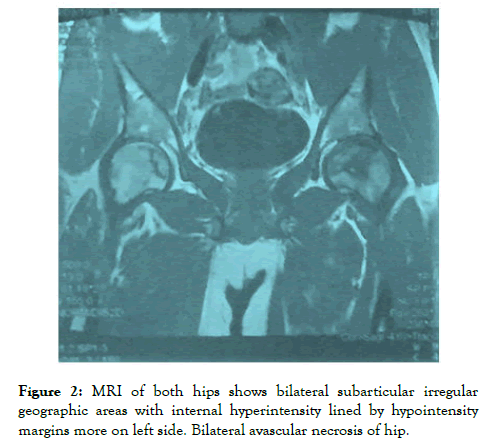
Figure 2. MRI of both hips shows bilateral subarticular irregular geographic areas with internal hyperintensity lined by hypointensity margins more on left side. Bilateral avascular necrosis of hip.
Infectious workup was done, quantiferon for tuberculosis was negative (three time), culture and sensitivity from right knee aspirate and biopsy showed bone infraction and MRSA and no acid fast bacilii, HIV Ab and PCR were negative (three times), and CD4+: CD8+ ratio was increased (Figure 3). Immunoglobin profile was increased, and protein electrophoresis showed hypergammaglobinemia. Hypercoaguable state investigation was done, showed normal protein s,c, factor V ledin, haemocystine in urine, MTHFER. In association Normal bone marrow aspirate and biopsy.
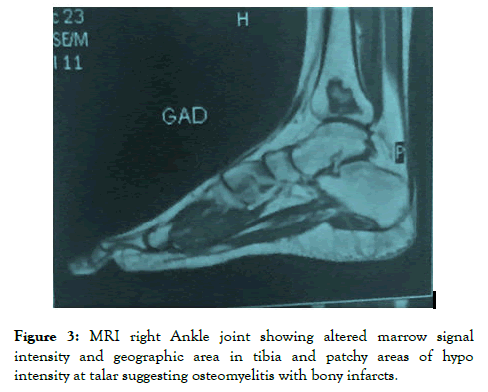
Figure 3. MRI right Ankle joint showing altered marrow signal intensity and geographic area in tibia and patchy areas of hypo intensity at talar suggesting osteomyelitis with bony infarcts.
Immunological panel was done, ANA, Antids DNA, RF, ANCA was negative, and lupus anticoagulant was negative. Anticardiolipin IgG titer and anti betaglycoprotein IgG were high and repeated after 3 months. Moreover, Computed tomography angiography and aortography revealed normal study. Patient sought medical advice with therapeutic dose of anticoagulant. Patient has undergone several surgeries for surgical debridement of recurrent septic arthritis of Right knee and patient was on anti MRSA antibiotic for 6 weeks. Finally, he is preparing for bilateral knee replacement.
Our patient fulfilled criteria of primary antiphospholipid syndrome (APS) as clinical entity (recurrent arterial thrombosis in picture of avascular necrosis) in absence of previous history of steroid and laboratory entity (positive antibodies for anticardiolipin and betaglycoprotein).
APS is an autoimmune disorder including a vascular thrombosis and/or recurrent pregnancy loss is observed in patients with laboratory evidence for antibodies against phospholipids or phospholipid-binding protein cofactors.
APS can occur as either a primary disease or secondary to a connective tissue disorder, most commonly systemic lupus erythematosus (SLE) (Table 1) [1].
| Clinical criteria | |
| Vasular thrombosis (confirmed by imaging studies or histopathological studies) | a. One more clinical episodes of arterial, venous or small-vessel thrombosis, in any tissue or organ |
| Pregnancy morbidity | a. Three or more sequential spontaneous abortions before 10th week of gestation; or |
| b. Unexplained foetal death of a morphologically normal foetus after 10th week of gestation; or | |
| c. Early birth before 34th week of gestation of a morphologically normal foetus due to eclampsia, severe pre-eclampsia or confirmed placental failure | |
| Laboratory criteria | |
| a. Lupus anticoagulant (LAC) present in plasma, confirmed on minimally two occasions with an interval of at least 12 weeks | |
| b. Anticardioliptin-antibodies (aCL),IgG-or-IgM-isotype, present in serum or plasma, with elevated titre (>99th percentile),confirmed on minimally two occasions with an interval of at 12 weeks | |
| c. Anti-β2 glycopreotein-I-antibodies, IgG -or IgM-isotype, present in serum or plasma (with titre>99th percentile), confirmed on minimally two occasions with an interval of at least 12 weeks | |
Table 1: Classification criteria for antiphospholipid syndrome [1].
Clinical manifestation of APS includes cerebrovascular disease, psychiatric disorders and musculoskeletal manifestation. Musculoskeletal manifestation of APS comprises avascular necrosis of bone (AVN) and bone marrow necrosis (Table 2) [2].
| Neurological manifestations of APS |
|---|
| Cerebro-vascular disease |
| Transient ischemic attacks |
| Ischemic strokes |
| Acute ischemic encephalopathy |
| Cerebral venous thrombosis |
| Epilepsy |
| Headache |
| Chorea |
| Multiple sclerosis |
| Transverse myelitis |
| Idiopathic intracranial hypertension |
| Other neurological syndromes |
| Sensori-neural hearing loss |
| Guillian-Barre syndrome |
| Transient global amnesia |
| Ocular syndromes |
| Dystonia parkinsonism |
| Cognitive dysfunction |
| Dementia |
| Other psychiatric disorders |
| Depression |
| Psychosis |
| Musculoskeletal manifestations of APS |
| Arthralgia/arthritis |
| Avscular necrosis of bone |
| Bone marrow necrosis |
| Complex regional pain syndrome type-1 (reflex sympathetic dystrophy) |
| Muscle infraction |
| Non-traumatic fractures |
| Osteoporosis |
Table 2: Clinical manifestation of antiphospholipid syndrome [2].
Pathophysiology of APS includes the activation of endothelium through oxidized LDL mediated vascular injury, Heparin Induced Thrombocytopenia (HIT) and molecular mimicry [3,4].
AVN documented in systemic lupus erythematous patients [5]. Prolonged high doses of Corticosteroid (CS) have been suggested as the highest risk for developing AVN, such patients usually have numerous associated risk factors such as Raynaud’s phenomenon, vasculitis, hyperlipidemia, and aPL antibodies [6].
it postulated that CS causing the AVN by suppression of osteoblastic function and interference with repair of microfractures, analgesic effect such as a Charcot-like arthropathy, production of periarterial and perivenous edema with secondary vascular compression, induction of blood hypercoagulability, alteration of fat metabolism and fatty emboli, or intramedullary lipocyte proliferation or hypertrophy [7]. The link between APS and avascular necrosis is still unknown [8]. Some authors suggest that antiphospholipids antibodies might predispose to AVN by causing microvascular thrombosis [9-12].
Staphylococcus aureus has been previously documented as the causative micro-organism in 80% of patients with septic polyarthritis, which is usually associated to previous joint disease, particularly rheumatoid arthritis. Polyarticular septic arthritis has also been described in patients with underlying SLE, but gram-negative bacteria and particularly Salmonella species are the more frequent causative agents.
Citation: Fayed F (2019) A Mono-Articular Septic Arthritis and Multifocal Avascular Necrosis in Absence of Corticosteroid Use: An Unusual Presentation of Primary Antiphospholipid Syndrome. Rheumatology (Sunnyvale). 9:255. DOI: 10.35248/2161-1149.19.9.255
Received: 25-Nov-2019 Accepted: 05-Dec-2019 Published: 12-Dec-2019 , DOI: 10.35248/2161-1149.19.9.255
Copyright: © 2019 Fayed F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.