Journal of Alcoholism & Drug Dependence
Open Access
ISSN: 2329-6488
ISSN: 2329-6488
Case Report - (2023)Volume 11, Issue 4
Background: Vitamin deficiencies are systemic conditions that can involve the central nervous system, with varying clinical pictures. In particular, B vitamins are crucial for metabolism in the brain.
They may present with a subacute clinical picture and a sudden worsening. In the case of B1 deficiency with Wernicke's encephalopathy, the classic triad of symptoms is not always observed, making diagnosis more difficult. In addition to the prompt recognition of a deficiency encephalopathy, it is essential to identify the cause of the vitamin deficiency. Deficiency of these can be traced to gastro-intestinal disorders, unbalanced diets, and alcohol abuse.
Case presentation: The clinical case below discusses an adult woman who presents acutely-subacutely with neurological disorders attributable to vitamin depletion, confusion, ataxia, aphasia and ophtalmoparesis. In addition to the diagnosis of this neurological condition, the cornerstone of this clinical case is the identification of the pathology underlying this vitamin depletion.
Conclusion: In the case of dysimmune diseases of the gastro-intestinal system that damage the ileum, a vitamin deficiency can occur. If unresolved, it can lead to severe and irreversible effects on brain function. This clinical case shows how rarely, a neurological condition can be the most striking symptom of a neglected and undiagnosed systemic pathology. The importance of knowing and recognizing these situations is crucial not only in terms of cerebral prognosis, but also for the overall well-being of the individual with respect to the underlying pathology.
Encephalopathy; Crohn; Inflammation; Subacute
We present the clinical case of a woman with subacute neurological symptoms attributable to a systemic pathology determining vitamin B group depletion. This group of vitamins is crucial for brain functioning, and when reduced clinical symptoms [1]. The rise of do-it-yourself vegan diets and bariatric surgery could also lead to a re-emergence of these clinical manifestations. Other causes include autoimmune gastropathies with the presence of intrinsic factor antibodies, coeliac disease, alcohol abuse, Whipple's disease and inflammatory intestinal diseases. An involvement of B-vitamin depletion in the case of infection of the central nervous system by T. pallidum has also been observed. The typical symptoms of deficiency deficits are not always unambiguous; in the case of B-vitamin deficiency we can observe neuropathies, spinal cord pathologies, worsening cognitive impairment and psychiatric manifestations. Not infrequently, neurological manifestations of vitamin deficiencies are the warning sign for systemic problems. The neurologist's promptness is important not only in identifying the vitamin deficiency and its symptoms, but also in conducting the appropriate investigations to understand its nature, in order to correct it as soon as possible. In fact, rapid and targeted vitamin replacement therapy is the only way to bring about an improvement in the clinical picture.
A 51-year-old woman came to the emergency room because of disorientation and marked postural instability. She denied home therapy.
Blood tests revealed Megaloblastic anaemia (Hb 9.30 gr/dl, MCV 104.6 fL), hypomagnesaemia (1.10 mg/dl), and hypokalaemia (2.9 mEq/L), Reactive-C-Proteine 40 mg/L. Brain Computed Tomography Scan (CT) and angio-CT were normal.
The woman appeared alert, fatuous and partially cooperative. She was disoriented. Aphasia, dysexecutive deficits, notes of disinhibition and inattention were detected. Bilateral ophthalmoplegia was present. She had ataxic gait with retropulsion and hypostenia in all four limbs; ROTs were weak, symmetrical, RPCs were in flexion.
An in-depth anamnestic examination with the family revealed that for some months he had been presenting increased irritability, episodes of disorientation, unsteadiness in walking, episodes of falling. He has reported, also for some months, frequently diarrheic bowel associated with cramping abdominal pains.
An Electroencephalogram (EEG) was carried out, showing a tendency to fall asleep and slowed bioelectric activity. Mini- Mental State Examination (MMSE) was administered, with a result of 9/30. The case was classified within subacute cognitive impairment.
The cytomorphochemical, cultural and virological examination of the Cerebrospinal Fluid (CSF) was within normal limits.
Laboratory investigations showed severe deficiency of folate, vitamin B12 and thiamine, which was undetectable [2].
Brain Magnetic Resonance Imaging (MRI) documented areas of hyperintensity in T2-FLAIR with restriction in Diffusion-weighted Imaging (DWI) at peri-aqueductal and ponto-mesencephalic level, on the mesial side of both thalami, and frontal cortico- subcortical bilaterally, similar to a cortical ribboning, a diagnosis of deficiency Wernicke's encephalopathy was made.
The patient started intensive B group vitamin replacement, and within a few days the ophthalmoplegia resolved almost completely with improvement in balance and cognitive disturbance. MMSE after 14 days was repeated with the result of 16/30. Brain MRI after two weeks showed a slight reduction in the changes (Figure 1).
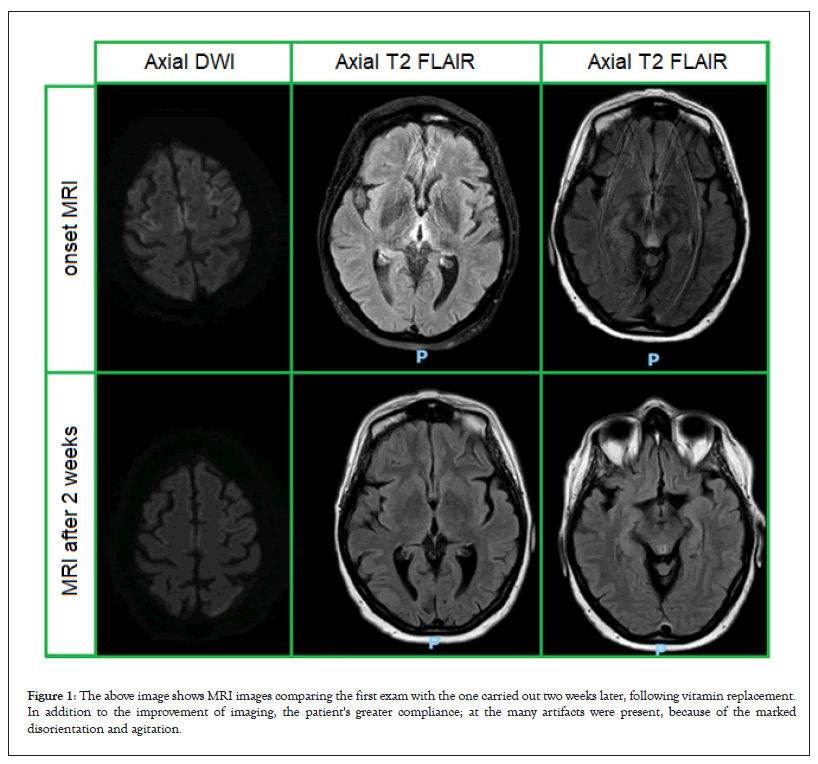
Figure 1: The above image shows MRI images comparing the first exam with the one carried out two weeks later, following vitamin replacement. In addition to the improvement of imaging, the patient's greater compliance; at the many artifacts were present, because of the marked disorientation and agitation.
Together with the management of the neurological scenario, the aetiology of the deficiency disorder was investigated. It did not appear to be related to a history of alcoholism. During hospitalisation, the patient continued to present Diarrhoea, sometimes with traces of blood. The faecal calprotectin test was over 300 mg/Kg, and chronic inflammatory bowel disease was hypothesised. Ferritin augmentation (824 ng/ml, nv<400 ng/ ml) and the reduction in transferrin (97 mg/dl, nv>200 mg/dl) confirmed the suspicion of chronic systemic inflammation.
Colonoscopy with Retrograde ileoscopy was performed, showing deep ulcerations of the intestinal wall, particularly at the level of the ileum, compatible with Crohn's disease [3]. The woman started a treatment for the intestinal disease, with an improving of her quality of life.
B vitamin-related deficiency encephalopathies are conditions that only if promptly diagnosed and treated can allow partial or total recovery of the patient's neurological condition. Although vitamin deficiency occurs chronically, and some symptoms may develop progressively and subtly, not infrequently the most striking neurological manifestations occur acutely/sub-acutely [4]. This abrupt onset may complicate differential diagnosis, involving vascular, infectious, and inflammatory or Paraneoplastic pathologies. Wernicke's encephalopathy classically presents with the symptom triad of ataxia, confusion and ophthalmoparesis. However, these features are not consistently present in the patient and often not even all at the same time [5]. In fact, particularly in patients with non-alcoholic Wernicke, the symptom triad is often absent. In addition, other clinical features may be present such as aphasia, altered ROTs, masking the classic triad, as in the case described.
Magnetic resonance imaging shows involvement of the periventricular regions, the medial formations of the thalamus, the floor of the third ventricle, and the mamillary bodies. Other structures involved are the periaqueductal region, the reticular formation of the midbrain, and the posterior corpora quadrigemina. The pathophysiology of WE is not totally cleared. Thiamine is used to maintain the osmotic gradients across cell membranes, thus, maybe its absence may determine oedema, and disrupture of hemato-encephalic barrier [6].
After the diagnosis of the brain condition, and the correct vitamin replenishment, the identification of the underlying cause is crucial. Inflammatory bowel disease can hinder thiamine uptake, and this may, in rare cases, be the most prominent onset symptom of the condition. The clinical and radiological features, together with the finding of a megaloblastic anaemia or other salient anamnestic features (vegan diets without supplementation, alcoholism, gastroenteritis), are useful elements in converging the diagnosis.
In the case of vitamin deficiencies, multidisciplinary work involving the neurologist, gastroenterologist and other specialists is important to identify the underlying problem. The clinical case described encourages collaboration between several figures.
This clinical case highlights the importance of the neurological symptoms that can occur in the course of inflammatory/systemic diseases; they can represent the first and only clinical expression of the disease. An accurate diagnosis that can be reached through a correct interpretation of imaging allows a correct therapy, radically changing the patient's prognosis, both neurologically and systemically. Indeed, if not corrected, vitamin depletion can lead to non-reversibility of the symptom and progressive involvement of other neurological functions. In this case, the importance of an accurate diagnosis was twofold, because on the one hand it allowed the progressive recovery of the neurological deficit, and on the other hand the establishment of an appropriate DMTs therapy for the intestinal autoimmune disease.
Citation: Bagnato MR, Pierantozzi M (2023) A Case Report on Deficiency Encephalopathy: What if it is only One Symptom of a Systemic Inflammatory Disease? J Alcohol Drug Depend. 11:403.
Received: 06-Oct-2023, Manuscript No. JALDD-23-27346; Editor assigned: 09-Oct-2023, Pre QC No. JALDD-23-27346 (PQ); Reviewed: 23-Oct-2023, QC No. JALDD-23-27346; Revised: 30-Oct-2023, Manuscript No. JALDD-23-27346 (R); Published: 06-Nov-2023 , DOI: 10.35248/2329- 6488.23.11.403
Copyright: © 2023 Bagnato MR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.