PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
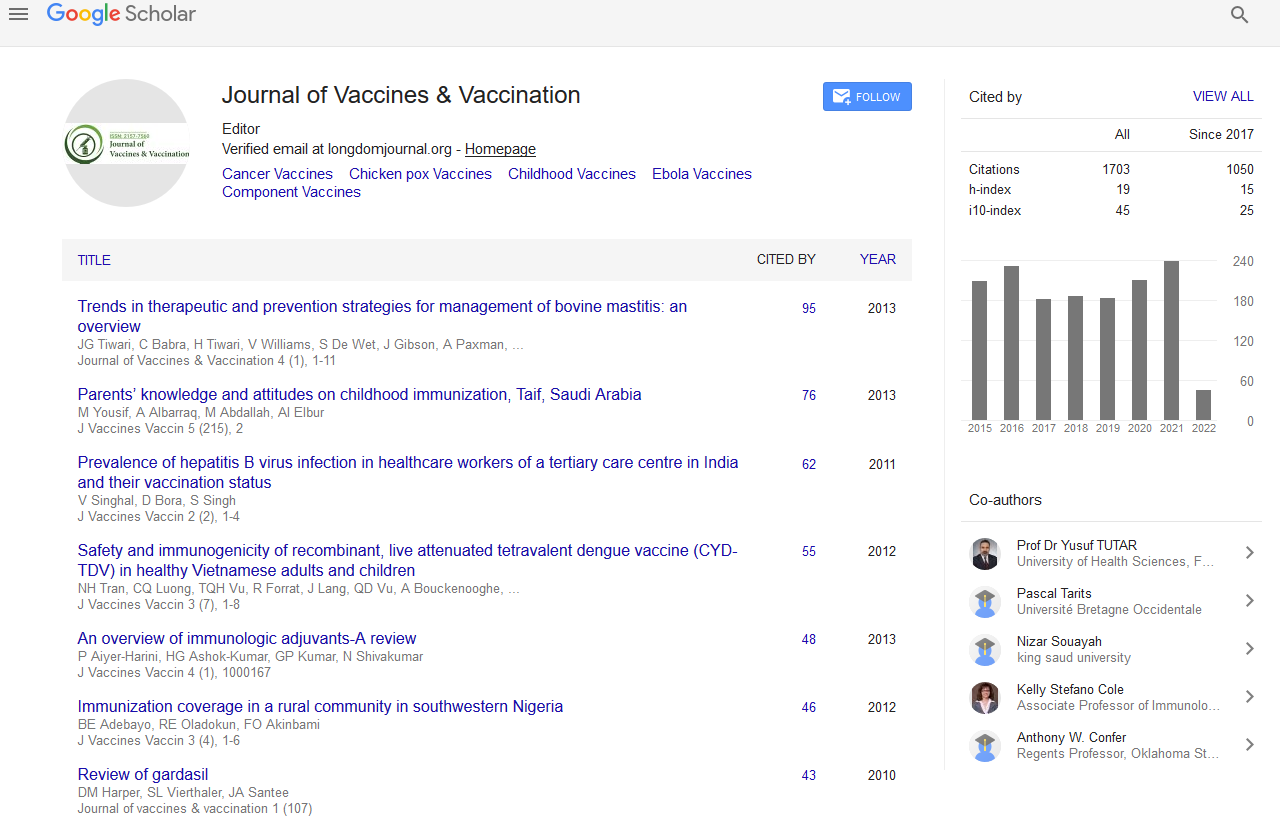
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Vaccination in risk groups with special focus on non-responsiveness to routine vaccines
4th International Conference on Vaccines & Vaccination
September 24-26, 2014 Valencia Convention Centre, Spain
Ursula Wiedermann
Scientific Tracks Abstracts: J Vaccines Vaccin
Abstract:
W orldwide vaccination programs against the most prevalent vaccine preventable diseases have been introduced by the health authorities to reduce morbidity and mortality rates, minimize disease outbreaks, and ultimately eradicate diseases. These recommendations are based on clinical trials performed in selected, healthy populations. The situation is unlike for patients with different chronic diseases and/or immunodeficiencies, since there is a lack of prospective randomized studies. Consequently, the vaccination recommendations are primarily based on theoretical considerations and are often quite imprecise, leading to suboptimal vaccine preventive care. Within the last years we concentrated our research programs on the immunological characterization of non-responsiveness to routine vaccines in healthy as well as different risk groups. Non- responsiveness in healthy individuals occurs in 2-10% of vaccinees and is defined by a lack of sufficient protective immune- responses after primary or booster vaccination. We could demonstrate that non-responsiveness to tick-borne encephalitis vaccine is associated with both, low humoral and cellular antigen-specific immune responses. In genetically pre-disposed hepatitis B non-responder, showing an association to certain HLA-DR subtypes, high IL-10 levels as well as increased regulatory T and B cells are linked to non-responsiveness to hepatitis B but also to other vaccine antigens. Immunosenescence is another risk factor for non-responsiveness to vaccination. With increasing age (>60 yrs) humoral and cellular responses are significantly lower, particularly to novel vaccine antigens, than in younger vaccinees and thus associated with increased infection susceptibility. We recently described that primary vaccination with Japenese encephalitis vaccine led to humoral and cellular non/low responsivenss in 47% of the vaccinated elderly. The frequency of regulatory T cells as well as late differentiated effector memory cells was significantly higher compared to the young vaccinees and this was associated with increased CMV-seropositivity. This study indicated that elderly may require different vaccination strategies, modified booster schedules and other adjuvants systems for vaccines, while primary vaccination should be encouraged to be done before the age of 60. Similar studies are now being performed in allergic patients and obese individuals, since their immunological status seems to be impaired as well and the effectiveness of vaccination is currently unclear. Along these lines, a multicentre study on vaccination of cancer patients is on the way to answer important questions, such as the influence of tumor entity, stage of diseases and chemotherapy on vaccine responsiveness. Thus, based on the obvious need for significant and solid data on vaccine responsiveness in diseased subjects, such studies will provide evidence for improved vaccination recommendations and specific vaccination strategies in the different risk groups of growing incidence with global impact on health systems and medical care.
Biography :
Ursula Wiedermann had studied Medicine in Vienna, Austria. Between 1990-1995, she completed her PhD thesis in Sweden at the Institute of Clinical Immunology, University of Gothenburg. Back in Vienna she continued her research career at the University of Vienna concentrating on mucosal vaccination against allergic diseases. After her habilitation (veniadocendi) in 1999 she founded the research group ?Mucosal Immunity and Vaccination?. In 2001 she finished her medical training as specialist for ?Immunology? and ?Specific Prophylaxis and Tropical Hygiene?. In 2004 she became Head of the Institute of Specific Prophylaxis and Tropical Medicine and in 2006 she was assigned Professor for Vaccinology at the Medical University Vienna. She is member of the Austrian Supreme Board of Health and since 2011 chair of the Austrian Advisory Committee for Immunization Practice of the Austrian Ministry of Health. She has more than 100 publications in peer reviewed journals and is frequently giving presentations at international and national conferences.