PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
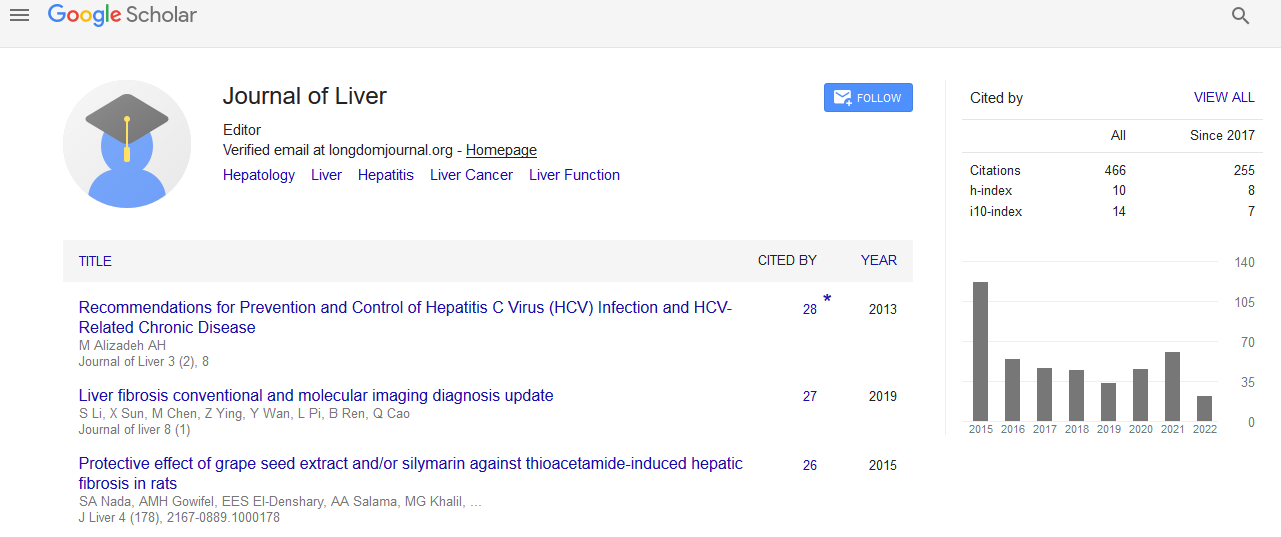
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Renal involvement in patients with Hepatitis B
4th International Conference on Hepatology
April 27-28, 2017 Dubai, UAE
Yuming Wang
Third Military Medical University, China
Keynote: J Liver
Abstract:
Chronic kidney disease (CKD) is defined as eGFR<60 mL/min-1.73m2 or a urinary albumin to creatinine ratio (ACR) >30mg/g is a global public health burden because of its increasing incidence and prevalence and progressive nature to end-stage renal disease (ESRD). The prevalence of adult CKD is over 10% and there are about 120 million adult CKD patients in China. Apart from major liver complications, clinical evidence suggests that chronic HBV infection exerts a negative impact on renal function, and can lead to glomerulonephritis, even in the absence of cirrhosis. In addition, nearly 15�??30% of patients with chronic hepatitis B (CHB) have baseline renal dysfunction or comorbidities associated with CKD. Prevalence of CKD is likely to rise in patients with CHB because of increasing age, more advanced disease, comorbidities and nephrotoxic therapies. A CHB infection can cause renal dysfunction through immune complex mediated glomerular diseases, such as membranous nephropathy and mesangiocapillary glomerulonephritis. In countries with endemic HBV infection, HBV-related glomerulopathies are an important cause of end-stage renal disease and renal replacement therapy. Currently, more and more attention is being paid to the safety issues for NUCs. Mitochondrial toxicity cannot explain the different adverse reactions, including nephrotoxicity, hyperlacticaemia, lactic acidosis, myopathy, peripheral neuritis, hepatic steatosis, etc. The currently approved oral antiviral agents are all primarily eliminated unchanged through the renal route. So, the core clinical issue is nephrotoxicity; other issues are either rare, related to a few special populations, or are easy to prevent. Consequently, current product labels recommend that in patients with renal insufficiency, dose reduction and/or increased dose intervals are recommended. Worsening of renal function during prolonged nucleotide therapy has primarily been reported with adefovir (ADV), but also with tenofovir (TDF). However, all current evidences indicate that among the NUCs, only telbivudine (LdT) therapy is associated with consistent increase in renal function (eGFR) across different CHB patient populations with decompensated and compensated disease. GLOBE study, a large scale clinical trial, has revealed that LdT significantly improved eGFR in CHB patients with compensated liver disease versus LAM/ETV. At the same time, most studies also revealed LdT can improve eGFR in patients with CHB versus ADV/TDF. But the mechanism of the beneficial effect of LdT therapy on renal function remains to be determined. These results may be important for clinicians to best assess the choice of antiviral therapy in those patients most vulnerable for renal dysfunction, including the elderly and those with baseline renal insufficiency, severe liver fibrosis, or decompensated liver disease. In summary, the number of patients with CHB with renal dysfunction is increasing. The key clinical safety issue for NUCs is nephrotoxicity. According to current evidence, patients with CHB receiving long-term NUC antiviral therapy should have renal function monitored. Renal function in patients with CHB improves steadily during long-term LdT monotherapy, while LdT+ADV/TDF combination therapy could improve eGFR as well. In addition, early prevention or protection of renal involvement is emphasized in clinical practice.
Biography :
Yuming Wang has obtained his MD degree and is a Professor and Chief Physician at Institute for Infectious Diseases, Southwest Hospital, Third Military Medical University, Chongqing. Currently, he serves as the Vice-President in Infectious Diseases Branch of Chinese Medical Doctor Association. His current research fields include severe hepatitis/liver failure, pathogenesis and treatment of viral hepatitis. He is the Chief Editor of 16 monographs, Associated Editor for 31 monographs and has published more than 400 papers, including Gastroenterology, Hepatology and CGH.
Email: wym417@163.com