Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
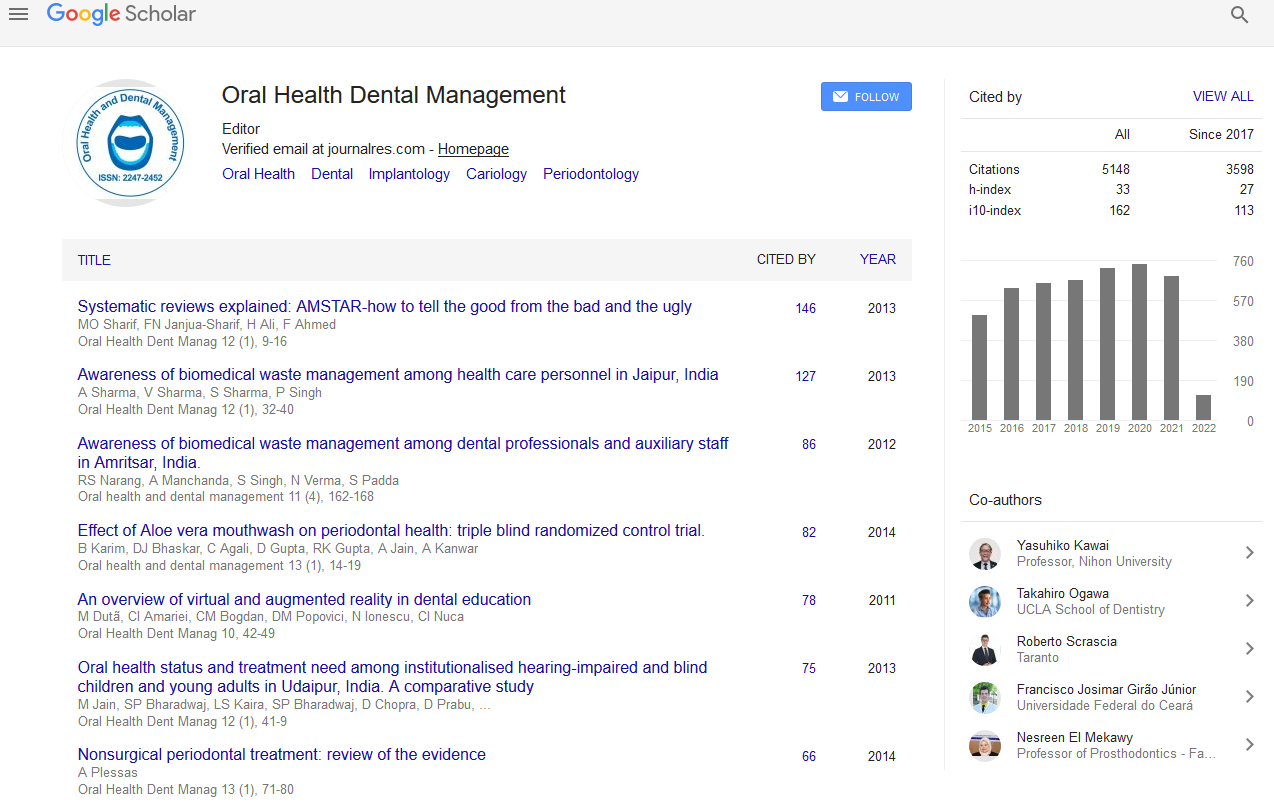
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Oral and craniofacial region treatments in the era of regenerative dentistry
5th American Dental Congress
October 05-07, 2015 Philadelphia, USA
Miroslav Tolar
University of the Pacific, USA
Keynote: Oral Health Dent Manag
Abstract:
Tissue bioengineering/regeneration is becoming a valid treatment modality in medicine and dentistry. It is making its way into oral and maxillofacial surgery, implantology, endodontics, orthodontics, prosthodontics. Patients like a regenerated own tissue that is maintained by its homeostatic mechanisms much more than artificial materials. It is clear that, at present, only adult mesenchymal stem cells (MSC) isolated from the patient and re-implanted to the same patient qualify for a clinical use. Research into biology and physiology of MSC revealed a number of interesting, sometimes surprising, features, by which MSC communicate with other cells. In response to tissue damage, MSC can synthesize and release growth factors and chemoattractants of immune cells, both supporting tissue regeneration. MSC can respond to biophysical clues in their environment (like oxygen tension and pH). MSC can also sense and respond to attachment substrate�??s elasticity variations and external mechanical forces. Of course, MSC can undergo their own tissue-specific differentiation process and become a source of regenerating cells. New findings show that MSC can form and release exosomes influencing behavior of neighboring cells when endocytosed. In situ microenvironment of MSC needs to be replicated as much as possible after explantation in vitro, namely physiological tissue normoxia and three-dimensional structure of cultures. Platelet-rich plasma or fibrins are often beneficial for both multiplication and differentiation of MSC. Recently, a number of clinical studies reported successful uses of bioengineered implants, thus showing possible ways for further investigations. Large mandibular defects were healed by bioengineered bone implants. Alveolar clefts were filled by bioengineered implants, sometimes in combination with distraction osteogenesis or guided bone regeneration. Dental pulp regeneration bioengineering technique has entered a clinical trial. Other clinical applications of MSC include engineering of soft-tissue, PDL, cartilage and skeletal muscle. Neural crest-derived MSC may differentiate into neurons or glia and support healing of spinal cord injuries. Promising developments indicate that an engineered bioroot may be available in a not very far future.
Biography :
Miroslav Tolar, MD, PhD, received his MD with honors at the age of 24 years from the 1st School of Medicine, Charles University in Prague, Czech Republic. He completed his PhD at the age of 29 years in the Institute of Physiology, Czechoslovak Academy of Sciences in Prague. Tolar’s research expanded from earlier tissue culture studies on nerve and muscle cell differentiation to his recent research focused on physiological ways of mesenchymal stem cell expansion in culture with the aim to preserve their normal functionality in the site of implantation in vivo. In addition to Czechoslovak Academy of Sciences in Prague, he conducted his research at the College of Physicians and Surgeons, Columbia University in New York, at Hyogo College of Medicine, Nishinomiya, Hyogo, Japan, and at several research laboratories at University of California in San Francisco. Dr. Tolar has over 50 scientific presentations, publications, invited and keynote lectures and held numerous visiting professorships. Recently, he gave courses in Kuwait, India, Nigeria and other countries on perspectives of tissue engineering and stem cells in dentistry. He established and is heading the Pacific Regenerative Dentistry Laboratory in the Dugoni School of Dentistry, University of the Pacific, San Francisco, CA, USA.
Email: mtolar@PACIFIC.EDU