PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
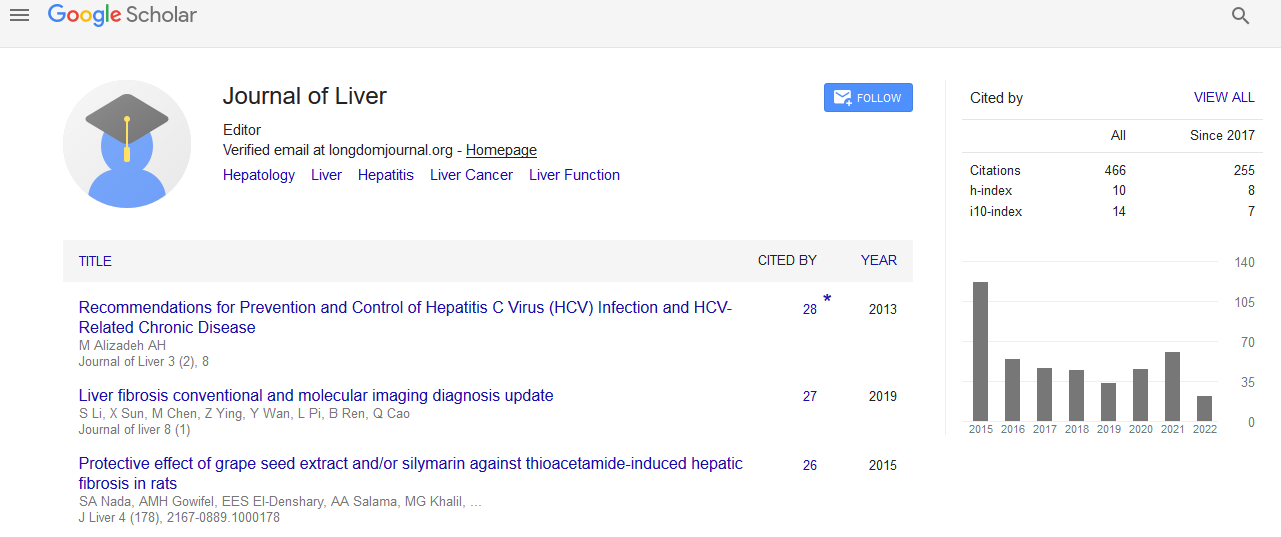
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
New advances in approaching of the alteration of Intrahepatic microcirculation in cirrhotic livers
World Congress on Hepatitis
July 20-22, 2015 Orlando, Florida, USA
Ying-Ying Yang
Posters-Accepted Abstracts: J Liver
Abstract:
From a hemodynamic point of view, the hepatic vascular resistance and portal inflow determine the level of portal pressure. Factors that determine the hepatic vascular resistance include both structural and dynamic components. Among the structural components are histological characteristics such as steatosis, fibrosis and regeneration nodules and neoangiogenesis. Dynamic structures include cells with contractile properties such as hepatocytes, hepatic stellate cells, sinusoidal endothelial cells and Kupffer cells. The contributions of the interactions between four cells in cirrhotic livers resulted in hepatic endothelial dysfunction, hepatic microcirculatory dysfunction, hepatic venous dys-regulation, hepatic fibrogenesis and subsequently increased intrahepatic resistance and portal hypertension in cirrhosis. The pathogenic mechanisms triggering the associated abnormalities in hepatic microcirculations including persistent endotoxemia, increased hepatic oxidative stress, activated endocannabinoids substances, pathogenic sinusoidal remodeling and hypo-perfusion in cirrhotic livers. Cumulative data suggested various therapeutic strategies targeting on the hepatic microcirculation effectively improvement of the systemic abnormalities of cirrhosis. Accordingly, the mechanistic and therapeutic approaches focusing on the disarrangement of hepatic microcirculation will introduce in this article.