PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
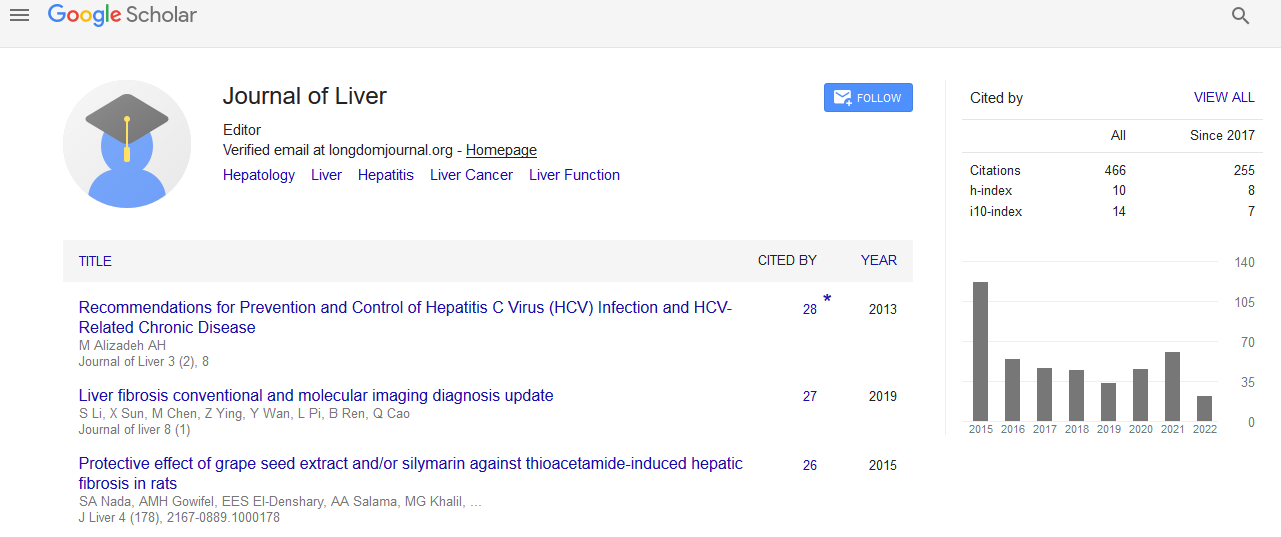
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Management of NAFLD in patients with DMT2
4th International Conference on Hepatology
April 27-28, 2017 Dubai, UAE
H Reynaert
UZ Brussel, Belgium
Keynote: J Liver
Abstract:
Non-Alcoholic Fatty Liver Disease (NAFLD) is defined by the presence of steatosis in >5% of hepatocytes. It comprises the spectrum of simple steatosis (Non-Alcoholic Fatty Liver or NAFL), and a progressive form, Non-Alcoholic Steatohepatitis (NASH), in which steatosis is accompanied by inflammation, fibrosis or even cirrhosis and hepatocellular carcinoma. NAFLD is associated with insulin resistance and its prevalence is increasing rapidly, paralleling the prevalence of metabolic syndrome. It is estimated that in some countries 30% of the population has NAFLD, but the prevalence in patients with diabetes mellitus type 2 (DMT2) is much higher. Moreover, in DMT2 patients, NASH is more prevalent. Therefore, it is imperative to screen patients with DMT2. In recent years, non-invasive methods to identify patients at risk have been developed. These include imaging techniques and several scoring systems consisting of clinical and biological data. In high risk patients, liver biopsy, which remains the gold standard for diagnosing and grading disease severity, should be performed. Patients at risk should be treated and strict follow-up to detect complications early is essential. We suggest an algorithm as depicted in Figure 1. Treatment of NASH is difficult and unsatisfactory. Weight loss by diet and life style changes (exercise) remains the cornerstone of treatment. It has been shown that �?�7% weight loss resulted in histological improvement. Weight loss is however problematic in this patient group: bariatric surgery improves all histological lesions in NASH including fibrosis. Up to now, no drug treatment has been shown to unequivocally improve NASH. PPAR-gamma agonists, vitamin E, FXR agonists, GLP-1 agonists and PPAR-alpha/delta agonists have shown favorable effects, but large phase 3 trials are lacking. A multitude of new drugs, targeting different metabolic pathways are being developed and tested. Hopefully, we will be able to treat patients with NASH more optimally in the near future.
Biography :
H Reynaert, MD, PhD is a Professor of Physiology and Pathophysiology at the Vrije Universiteit Brussel. He is Head of the Hepatology Unit at the University Hospital Brussels (UZ Brussel) and Senior Researcher in the Liver Cell Biology lab at the Vrije Universiteit Brussel. He is the past President of the Belgian Association for Study of the Liver (BASL) and current President of the Flemish Society of Gastroenterology (VVGE). He is the member of many national and international societies, including AASLD, EASL, and AGA. He is interested in many aspects of liver disease, including cirrhosis and its complications, viral hepatitis and non-alcoholic liver disease (NAFLD).