PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
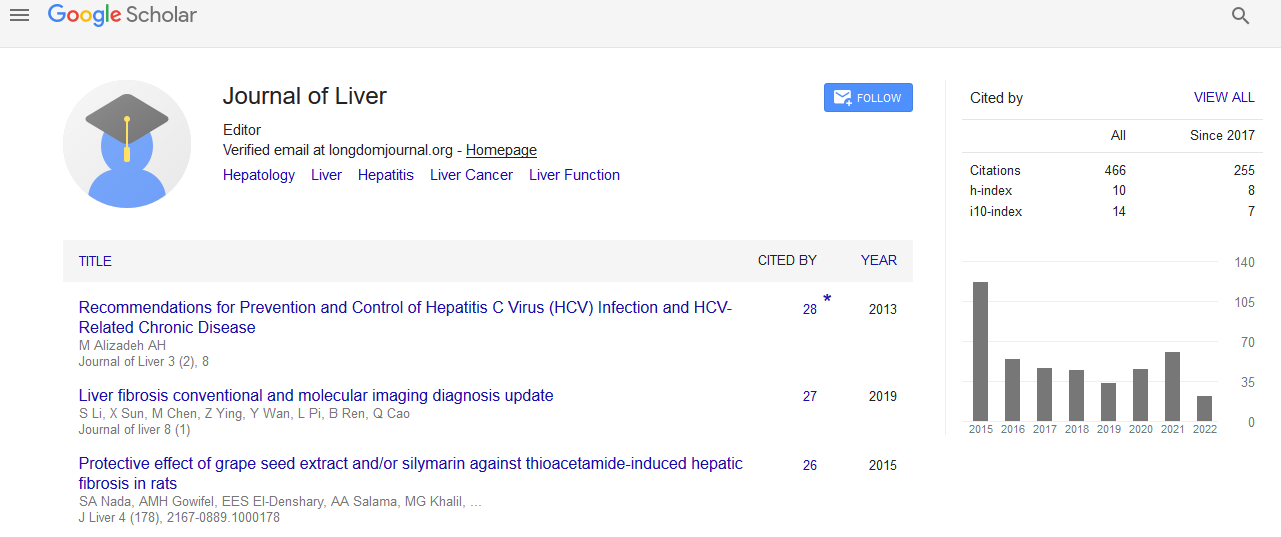
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Injudicious use of proton pump inhibitors: An audit from a tertiary care center in UAE
3rd World Liver Congress
December 17-18, 2018 Abu Dhabi, UAE
Fatima Hazin and M A Zahid
Tawam Hospital, UAE
Posters & Accepted Abstracts: J Liver
Abstract:
Background & Aim: Proton Pump Inhibitors (PPIs) are widely used and their use is associated with increased risk of adverse
events including increased risk of death. However, they are still widely prescribed often injudiciously in clinical practice. We
aimed to examine the current practices of PPI prescription especially the awareness among clinicians of its potential hazards.
Design: It is a retrospective audit study at Tawam Hospital, Al Ain, UAE.
Method: A random cohort of 50 inpatients currently on PPI therapy was selected. Information related to PPI therapy was
gathered using patient management software CERNER. Important information included indications and duration of therapy,
potential drug interactions and drug review or treatment modification along with useful information related to patient
characteristics like demographics and comorbidities.
Results: A total of 50 patients on current PPI therapy were selected for analysis. Average age was 68.34 years (Range 17-100).
Common comorbidities included Type-2 Diabetes mellitus (44%), Hypertension (68%), chronic kidney disease (34%) and
Ischemic heart disease (20%). Common drug interactions included Clopidogrel (24%), Benzodiazepine (4.4%), Phenytoin
(4.4%), Apixiban (6%) and Warfarin (8%). Average duration of PPI therapy was 72.1 months (range 2-115). The indications
were GERD (5/50, 10%), Prophylaxis on anti-platelet therapy (11/50 22%) and gastritis (1/50, 2%) whilst there was no clear
indication in 23 patients (46%). PPIs were also considered as prophylaxis for drugs that do not require PPI cover including
warfarin (6/50, 12%), steroids (3/50, 6%) and Apixiban (2/50, 4%). The average dose of therapy was 33.8 mg daily with treatment
divided among various drugs Omeprazole (8/50, 16%), Pantoprazole (16/50, 32%), Esomeprazole (24/50, 48%). PPI therapy
was started as intravenous treatment in 1 patient without any discernible indication. Drug therapy was reviewed in most of the
patients in prior 6 months but only resulted in drug cessation in 11(22%) patients with no treatment de-escalation in any patients.
Conclusion: The results suggest a trend towards excessive and often injudicious use of PPIs in most of the patients. Limiting
PPI use and duration to instances where it is medically indicated is highly warranted especially considering the increasing
concerns regarding their long term safety.
Biography :
Fatima Hazin is a Medical Resident in Tawam Hospital, Al-Ain. She is currently pursuing her third year Residency in Internal Medicine.
E-mail: fhazin@seha.ae