PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
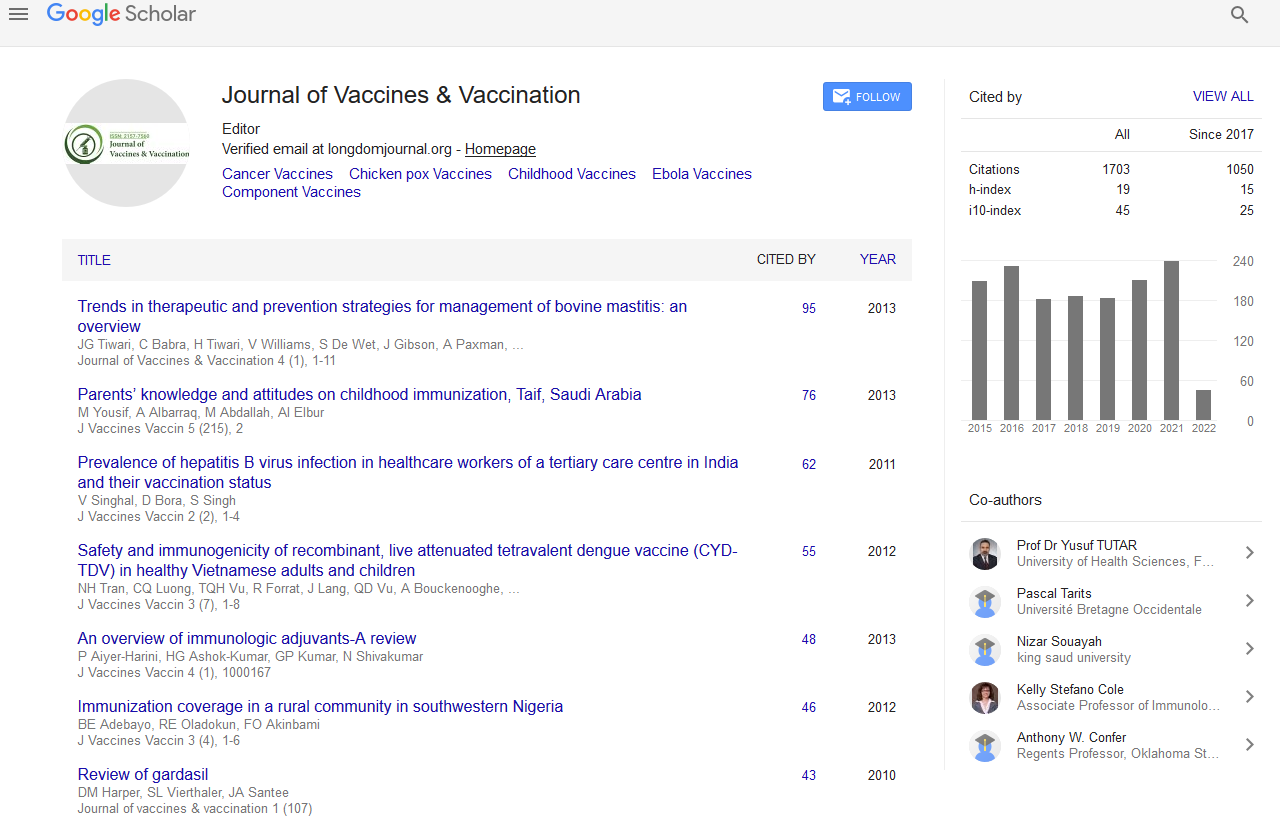
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
HPV vaccination in ARV-treated HIV-infected adolescents and young adults induces strong HPV-specific cell-mediated immune responses
3rd International Conference on Vaccines & Vaccination
July 29-31, 2013 Embassy Suites Las Vegas, NV, USA
Veronica Rainone, Daria Trabattoni, Francesca Penagini, Francesca Dinello, Gian Vincenzo Zuccotti, Vania Giacomet, Alessandra Vigano and Mario Clerici
Accepted Abstracts: J Vaccines Vaccin
Abstract:
Background: Human Papilloma Virus (HPV)-associated ano-genital infections represent the most common sexually transmitted disease in the general population. The incidence of HPV-associated cancers has been increasing in HIV-infected patients. HPV vaccination may be an important approach to reduce the risk of HPV-associated cancers in HIV-infected patients and a combined strategy of screening and HPV vaccination may guarantee a more adequate prevention of HPV-associated lesions. Immunogenicity of HPV vaccines in HIV-infected patients is still not adequately evaluated. We analysed safety, immunogenicity and efficacy of a quadrivalent HPV vaccine in HIV-infected patients without baseline molecular evidence of vaccine-type HPV infection focusing on HPV-specific cell mediated immunity (CMI). Methods: 31 ARV-treated HIV-infected adolescents (age range 28-14 years, mostly with undetectable viremia and effective CD4 recovery) and 25 sex- and age-matched HIV-seronegative healthy controls were enrolled in the study. Quadrivalent HPV- 16/18/6/11 VLP vaccine (Gardasil?) was administered at baseline, 2 months and 6 months. Safety was evaluated in terms of rate and severity of vaccine-related adverse events. Immune activation (CD4/CD25/HLADRII, CD8/CD25/HLADRII), naїve and memory T-cell patterns and HPV-specific immune responses (CD4/IFN-γ/IL-2, CD8/IFN-γ/TNF-γ, CD8/Perforin/GranzymeB) were evaluated at baseline and after vaccine administrations. Results: Results obtained after the first immunization in HIV-infected individuals show: 1) no changes in CD4 counts, percentage of CD4 cells and HIV viral load; 2) a significant increase in naїve CD8 T-cells, activated CD8 T-cells and in central memory CD4 and CD8 T-cells; 3) a significant reduction in terminally differentiated CD8 T-cells; and 4) a significant augmentation of unstimulated and HPV-specific IL2+/CD4+, IFN-γ+/CD4+, IFN-γ+/CD8+ and TNF-α+/CD8+ T-cells. No differences were observed in Perforin- or Granzyme B-secreting CD8 T-cells. Similar results were obtained in healthy controls. Conclusions: Quadrivalent HPV-16/18/6/11 VLP vaccine induces strong HPV-specific cell-mediated immune responses in ARV-treated HIV-infected individuals that are comparable to those observed in HIV-seronegative controls. HPV-specific CMI is likely an important component of the protective effect of this vaccine, data herein indicating that this component is not impaired in ARV-treated HIV infected individuals.