PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
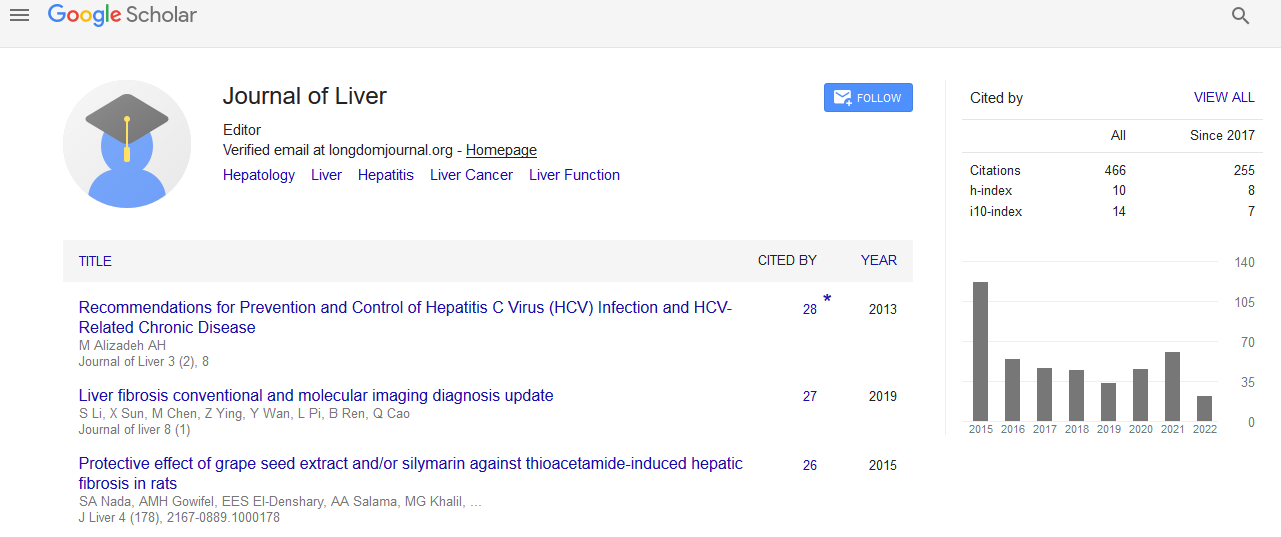
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
HBsAg Quantification: Useful for monitoring natural history and treatment outcome
World Congress on Hepatitis
July 20-22, 2015 Orlando, Florida, USA
Michelle Martinot-Peignoux
Posters-Accepted Abstracts: J Liver
Abstract:
Serum hepatitis B surface antigen (HBsAg) level reflects the transcriptional activity of the covalently closed circular DNA in the liver. In clinical practice, quantification of HBsAg (qHBsAg) is a simple and reproducible tool that may be used in association with HBV-DNA to classify patients during the natural history of HBV and to monitor therapy. There is a growing interest in serum HBsAg quantification (qHbsAg). In hepatitis B e antigen (HBeAg) positive chronic hepatitis B, HBsAg level is higher in the immune tolerance phase than the immune clearance phase, HBsAg titers are negatively correlated with liver fibrosis. In HBeAg negative patients HBsAg level <1000 IU/ml and HBV-DNA titer <2000 IU/ml accurately identify inactive carriers. In HBeAg-negative patients, combination of low hepatitis B virus (HBV) DNA and low HBsAg levels may predict low risk of HCC, and probability of HBsAg loss. During PEG-IFN treatment qHBsAg identifies patients with no benefit from therapy at week 12, allowing stopping or switched therapy so call the ?week 12 stopping rule?: Absence of any decline at week 12: Prediction of non response therapy should be ended or switched to nucleos(t)ide analogues, Any decline at week 24 prediction of response continue the 48 weeks therapy. During nucleos(t)ide analogues therapy the role of qHBsAg need to be clarified. Although the HBsAg decline is slow with nucleos(t)ide analogue therapy, a rapid decline may predict future HbsAg seroclearance. More recently an HBsAg titer <1000 IU/ml during at least 3 measurements during nucleos(t)ide analogue therapy might allow to end therapy with los risk of relapse.