PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
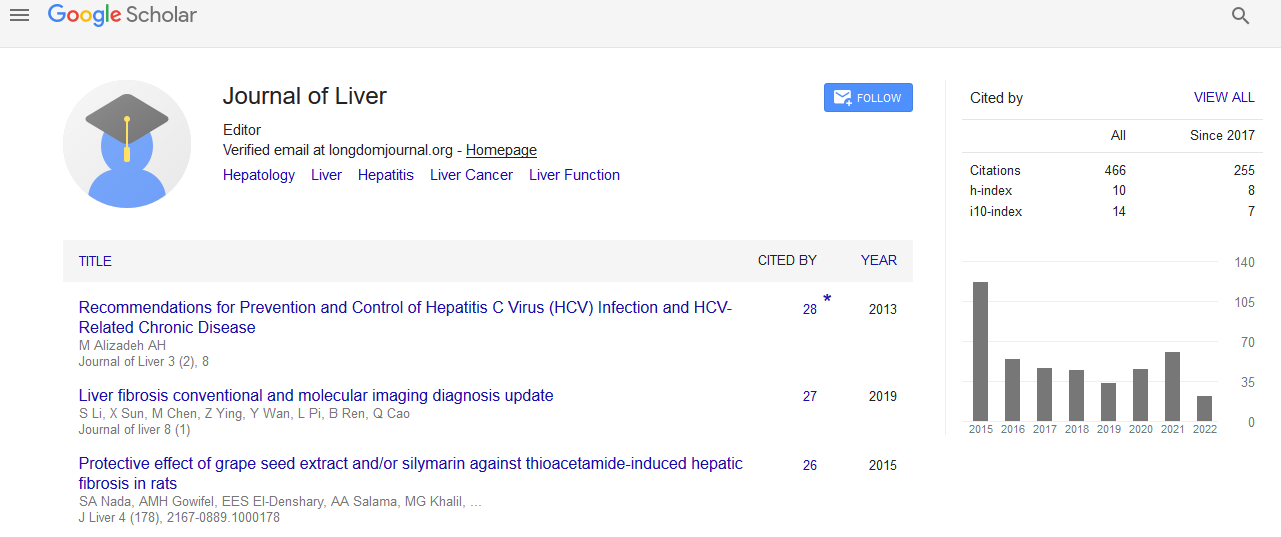
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Evolving role of minimally invasive (laparoscopic and robotic) donor hepatectomy
4th International Conference on Hepatology
April 27-28, 2017 Dubai, UAE
Rehan Saif
Aster Medcity, India
Aster CMI Hospital, India
Scientific Tracks Abstracts: J Liver
Abstract:
Liver transplantation has become an established modality of treatment for patients with end stage liver disease. The shortage of deceased donor organs has led to living donor liver transplantation (LDLT) becoming a valid alternative in selected transplant centers, and its safety and feasibility have been well determined. Minimally invasive surgery mainly laparoscopic surgery has been adopted in various surgical fields over the last two decades with well validated advantages such as reduced blood loss, reduced postoperative morbidity, shorter hospital stay and excellent cosmetic outcome in comparison to conventional open surgery. However, despite inception over 15 years ago laparoscopic liver resection has remained mainly in the domain of selected centers and enthusiasts. The delay in the wide application of minimally invasive liver surgery can probably be explained by the requirement of extensive open liver resection experience, in-depth understanding of anatomy, and potential for massive bleeding, need for considerable laparoscopic technical expertise and a protracted learning curve. Given that a liver resection is ideally suited for a minimally invasive approach as there is no anastomosis and a very large incision is required in the open approach, there has been an increasing interest in this technique worldwide. However the actual experience is limited to a few selected centers and guidelines remain inadequate. Furthermore, the application of minimally invasive liver surgery to liver graft procurement in LDLT have been delayed significantly due to concerns about donor safety, graft outcome and the requirement of expertise both in laparoscopic liver surgery and LDLT. Some experienced centers now routinely employ laparoscopic left lateral segmentectomy as standard of care in adult-to-pediatric LDLT. There has been a recent shift in the application of minimally invasive approach towards the procurement of left lobe and right lobe grafts in adult-to-adult LDLT. However the number of cases is too small and restricted to very few centers. The use of newer technology such as the robotic platform offers certain distinct advantages over traditional laparoscopy such as a stable magnified field with 3-D vision and enhanced instrument articulation, enhanced ability for suture ligation and an additional fourth robotic arm. This facilitates and improves the possibility of minimally invasive liver resection even in challenging major liver resection such as liver graft procurement in LDLT. Minimally invasive live donor hepatectomy is technically feasible with outcomes comparable to conventional open surgery. However careful validation of larger sample sizes is necessary to achieve standardization and wider application. The most important concern remains donor safety.
Biography :
Rehan Saif is a Consultant in HPB Surgery and Abdominal Multi-Organ Transplantation. He is associated with the Integrated Liver Care Team at Aster DM Healthcare Group in India running multi-organ transplant centers at Aster Medcity, Kochi and Aster CMI Hospital, Bangalore. He completed his Post-graduate General Surgical training in India following which he spent 12 years gaining further specialist higher surgical training in the United Kingdom. He obtained his MRCS and FRCS (HPB and Transplantation) from The Royal College of Surgeons of Edinburgh leading on to CCT (UK). He also completed the European Diploma in Transplantation (European Society for Organ Transplantation) and is accredited by the UEMS (European Board of Surgery) where he obtained his FEBS (HPB Surgery). This was followed by a period of further fellowships and training in the field of Liver Transplantation first at the Institute of Transplantation, Newcastle upon Tyne, UK (Post CCT Senior Fellowship) and then an International Travelling Fellowship in Living Donor Liver Transplantation at the Kaohsiung Chang Gung Memorial Hospital, Taiwan (RCSEd Ethicon Travelling Fellowship). He is also trained in the Field of Robotic Minimally Invasive HPB Surgery in the UK, Europe and has done an International Fellowship in Robotic HPB Surgery at UIC Medical Center, Chicago (USA). He is an expert in highly advanced procedures including liver transplantation (live donor and cadaveric), pancreas transplant, kidney transplant, complex HPB surgery and minimally invasive robotic HPB surgery.