PMC/PubMed Indexed Articles
Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
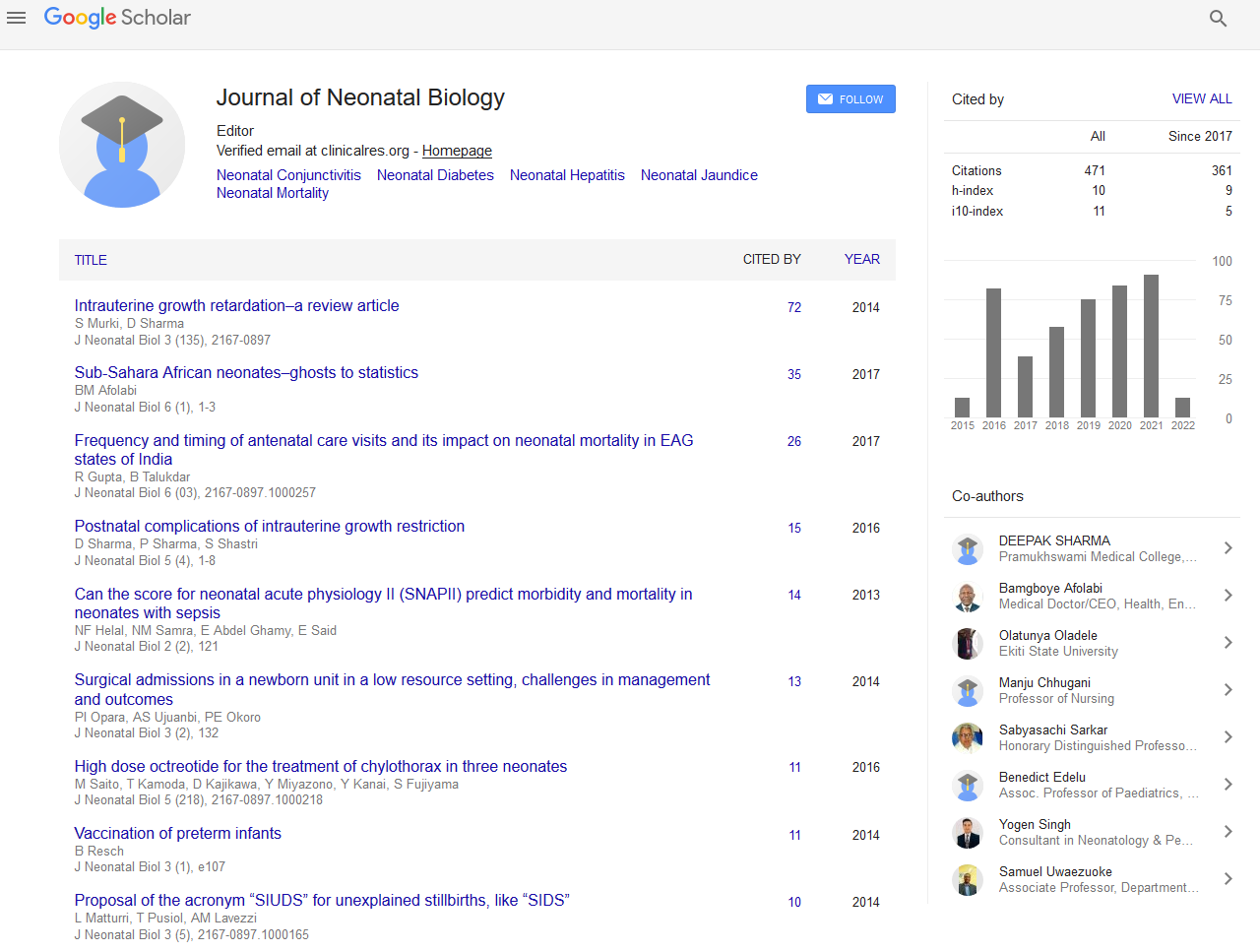
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Chronic obstructive pulmonary disease of prematurity in preschool children: Our experience
9th International Conference on Neonatology and Pediatric Neurology
November 28-30, 2016 Valencia, Spain
Pietro Sciacca
NICU- University of Catania, Italy
Keynote: J Neonatal Biol
Abstract:
Bronchopulmonary Dysplasia (BPD) is the most common respiratory disorder that affects chronically preterms with immature lungs. On this base it seems extremely pressing to investigate the consequences of BPD also in preschool children to assess the incidence of respiratory disease and the cardiovascular impact, focusing on functional study of right ventricle whose parameters can be used as an index of bronchopulmonary impairment. The population study includes 105 premature born between January 2008 and December 2012 with GA<33 week; BW<1800 gr; No malformations or surgeries. The echocardiography study has evaluated: L Ventricular Ejection Fraction (EFVS %); Tricuspidal Annular Plane Systolic Excursion (TAPSE); Pulmonary Artery Pressure (PAP); Right Ventricle Isovolumic Relaxation Time (IVRT); Right Ventricle Isovolumic Contraction Time (IVCT). The control group included 30 pre-school children born at term. In 35 cooperating infants, we have evaluated the lung function by the opening interrupter technique (OIT) with the measurement of airway resistance (RINT) (ratio between pressure change and flow). The presence of airway obstruction was detected as a value of RINT higher than 1.20. As results our data have shown: recurrent respiratory infections in 45.7%; upper air way obstruction in 22.3%. We found higher values of RINT in 69/105 (65.7%). The echocardiography assessment has highlighted higher values of PAP (30 versus 20.7 mmHG) and lower values IVCT (64.75 versus 74.55) in preterm than in the control group, both with a statistical difference (p<0.05). Our data have shown: recurrent respiratory infections in 45.7%; upper air way obstruction in 22.3%. We found higher values of RINT in 69/105 (65.7%). Our results showed a significantly higher incidence of respiratory issues, also before 4 years of age, in ex-preterm subjects than in the general population. The subclinical cardiovascular involvement of right cardiac sections, with an increment of PAP and an alteration of IVCT was significantly related to the incidence of respiratory issues. Right ventricle parameters have also been demonstrated useful for lung disease�??s follow-up in preschool children because they are easy to obtain and repeat and need just a bit of cooperation usually obtainable in almost all infants. Our data concerning not only increased incidence of wheezing, but of other respiratory issues contribute to recent definition of �??chronic obstructive pulmonary disease of prematurity�?� as a nosographic entity encompassing: asthma, need for respiratory hospitalization, more frequent bronchopulmonary infec tions and clinical subclinical pulmonary hypertension with right ventricle impairment that is typical of grown Bronchodisplastic survivors. Graph 1. Demonstrated higher values of Pulmonary Artery Pression (PAP) in preterm preschool children than in the control group, p<0.001 (BOXPLOT PAP); among preterm group, a statistically significant evidence versus control group was observed also for Isovolumic Contraction Time (IVCT), p<0.05 (BOXPLOT IVCT).
Biography :
Pietro Sciacca, PhD, works in the Department of Pediatrics of the University of Catania (Italy) as Pediatrician and Neonatologist with main interest in Pediatric Cardiology and Pediatric Bronchopneumology since 1985. He is a Professor of Clinic of Heart Malformations in Neonatologic Cardiology Post-graduate Course, of BAN of the University of Catania and of the Pediatric Cardiology Master of University of Messina.
Email: pietrosciacca@hotmail.it