PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
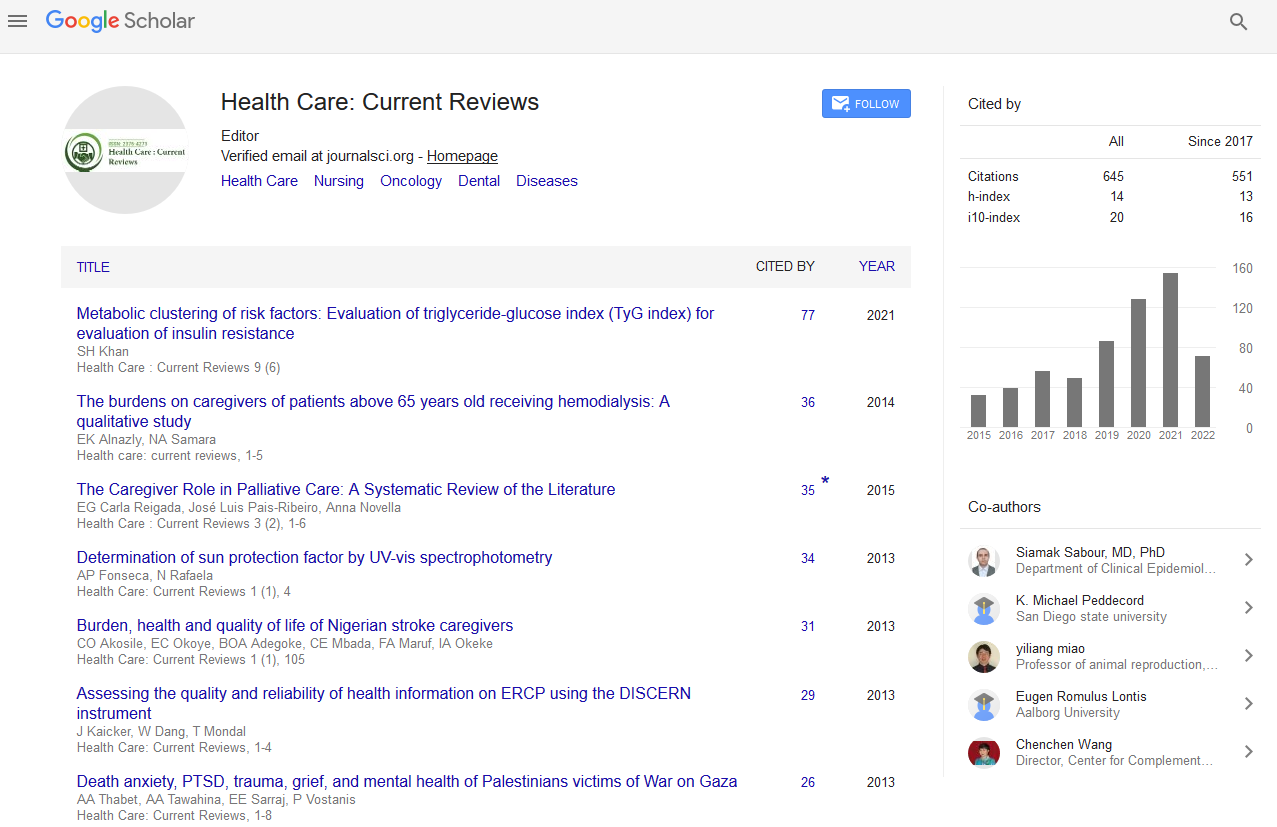
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Are current assessment protocols capable of identifying people at risk of HIV associated cognitive impairment?
4th Asia-Pacific Global Summit & Expo on Healthcare
July 18-20, 2016 Brisbane, Australia
Denise Cummins, Donna Waters, Christina Aggar and Catherine C O Connor
University of Sydney, Australia
Sydney District Nursing, Australia
Community Health Australia, Australia
The Kirby Institute, Australia
Scientific Tracks Abstracts: Health Care Current Reviews
Abstract:
Background: As People Living with HIV (PLHIV) are susceptible to chronic and comorbid health conditions, including an increased risk of cognitive impairment, HIV Associated Neurocognitive Disorder (HAND) can affect up to 50% of PLHIV causing various levels of disability. HAND is difficult to identify as signs and symptoms are nonspecific and diagnosis is by exclusion. The study is on how health professionals collect information which can show impact on patient�??s current and future clinical care. Aim: The aim of this study was to review protocols for which patient information from two specialist HIV interdisciplinary community teams in Sydney, Australia was collected to ascertain if the patient data methods could identify individuals at risk of HAND. Results: A total of 262 files were audited to determine patient demographics, clinical and social history. Results showed mean age of 50 years, a HIV diagnosis of 15 years, 74% lived alone and 45% referred for case management. Those older than 50 years were more likely to have hypertension p=0.057, hyperlipidaemia p=0.04 and hypercholesterolemia p=0.007. HIV clinical risk factors for HAND (CD4 Nadir, current CD4 count, HIV viral load) were inconsistently collected. Conclusion: PLHIV are an ageing population and may develop chronic conditions potentially increasing their risk of HAND. Routine collection of accurate information is important to assist clinicians to identify PLHIV at increased risk of HAND. Additionally, community care teams providing care to PLHIV may be well placed to notice cognitive changes in PLHIV who live alone and may have no other means of continuous clinical observation.
Biography :
Denise Cummins has been working as a Clinical Expert in the area of HIV disease for over 20 years, in acute and ambulatory care settings. Currently, she is working in community health. She has a Master’s in Public Health and purusing her PhD at the University of Sydney. She has published 19 articles and has been the primary investigator in several research projects. She has experience in developing and facilitating workshops in Thailand, Nepal, Papua New Guinea and Myanmar in a voluntary capacity and was a co-author for Asia Pacific Manual and Training Resource on counseling skills for HIV support workers.
Email: so.jo@bigpond.com