Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 4, Issue 2
Ventral Hernia Repair: A National Survey in the Republic of Ireland
Mannion Jennifer*, Horan Michelle, Tewatia Vikram, Vu Mary, Johnston Sean and Hehir DermotReceived: 09-Jun-2020 Published: 01-Jul-2020, DOI: 10.35248/2684-1606.2020.4.131
Abstract
Introduction: Abdominal wall herniation is a common surgical problem and repair is associated with high complication and recurrence rates. The operative approach is variable depending on patient and hernia characteristics. While there has been a gradual trend towards minimally invasive techniques internationally, surgical practice in the Republic of Ireland is currently undocumented.
Aim: To establish current surgical practice for the repair of ventral hernias in the Republic of Ireland
Methods: A national survey was disseminated via email and standard postage to all identifiable General Surgeons (N=168) to include those employed in the public and additionally those working in the private health sectors. The questionnaire consisted of 11 questions pertaining to the respondents current practice.
Results: The response rate was 61% (N=103).Analysis was performed using Survey Monkey software. 45% of respondents identified as colorectal surgeons and 54% operated in model four public hospitals. 64% perform less than five repairs per month and an open approach predominates for small (87%) and large (70%) hernias. Laparoscopic repair accounted for 40% of medium sized defects. There was equal use of extraperitoneal or intraperitoneal mesh placement. Component separation was utilized by 63% with open anterior being the most common approach.
Conclusion: This study demonstrates an unexpected trend towards low volume practice; these data also indicate frequent use of open anterior component separation which does not concur with current international data. Further research is required and prompt introduction of a national database must be a priority
Keywords
Ventral Hernia; Ireland; Mesh; Laparoscopic repair
Introduction
A ventral hernia comprises a defect in the abdominal wall and may be spontaneous; alternatively, herniation can result from previous trauma or surgical insult to the abdominal wall in which case it is referred to as an incisional hernia. Such herniation is estimated to occur in 10-50% of patients following midline laparotomy depending on the operation performed [1]. Incisional hernia associated with impaired healing of the facial defect, is a common post-operative complication and may constitute a significant challenge for the restoration of abdominal wall integrity. Risk factors include obesity, smoking, aneurysmal disease, malnourishment, steroid therapy, renal disease, and malignancy [2].
While herniation may be relatively asymptomatic, larger defects may be associated with considerable personal and socioeconomic hardship, gastrointestinal upset, pain and poor mobility. Furthermore, the risk of intestinal incarceration, obstruction or ischemia may be life threatening. Additionally, patients may be limited in their ability to work and participate in socially inclusive activity. Successful repair therefore can markedly improve a patient’s quality of life [3].
In Ireland, ventral hernia repair is a common surgical procedure and is usually performed by general surgeons [4] there is little consensus amongst surgeons as to the most appropriate, cost effective and technically feasible procedure. The surgical options for repair have expanded rapidly in recent years and can be influenced by the nature of the hernia as well as patient co-morbidities and the surgeons’ technical ability. Internationally there has been a trend towards minimally invasive surgery hybrid, laparoscopic and robotic with concepts such as chemical and surgical component separation being advocated in surgical literature [5].
Much of the current data is generated from hernia databases in Europe [6-8] and the USA [9]. Unfortunately, at present there in no equivalent registry in the Republic of Ireland; there is a paucity of practice documentation. This study is the first to our knowledge which engages with Irish Surgeons on the topic of ventral hernia repair.
Aim and objective
Our aim was to establish current practice in relation to ventral hernia repair and to identify variations based on subspecialty, workload, grade of hospital and surgical approach based on the size of the hernia defect.
Methods
A questionnaire to interrogate subspecialty, workload and surgical approach to ventral hernia repair was designed. In November 2018, utilizing email/standard postage, it was disseminated to all identified General Surgeons (N=168); it aimed to include where possible, individuals practicing in the public service (model 3 and 4 hospitals) and also those practicing exclusively in private hospitals in the state. Responses were compiled and analyzed using Survey MonkeyTM software.
Results
The response rate was 61% (N=103). The majority of respondents (45%) were colorectal surgeons while the remainder identified as Breast (17.5%), Upper Gastro-intestinal (13.5%) and Hepato-biliary surgeons (6.8%). The majority of (54%) were employed in model 4 hospitals with 30% operating in model 3 hospitals; 14% were employed in a private institution.
When quantifying workload, 65% performed less than 5 ventral hernia repairs per month, 24% between 5-10 repairs; 4% performed more than 10 per month. The monthly workload was explored with 34% performing less than 10, 31% between 10-20 and 35% more than 20 laparoscopic procedures per month (Figures 1-3).
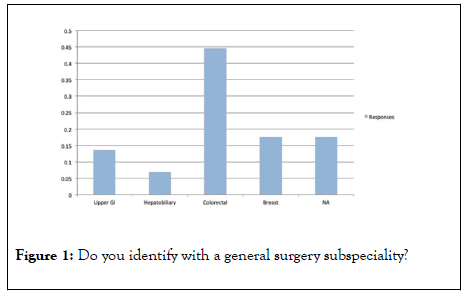
Figure 1: Do you identify with a general surgery subspeciality?
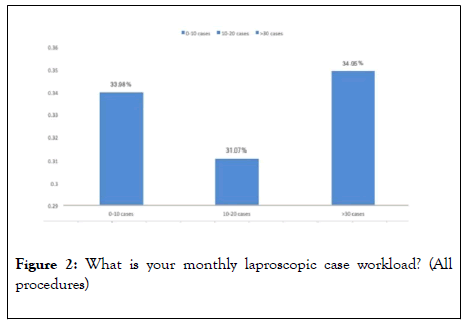
Figure 2: What is your monthly laproscopic case workload? (All procedures)
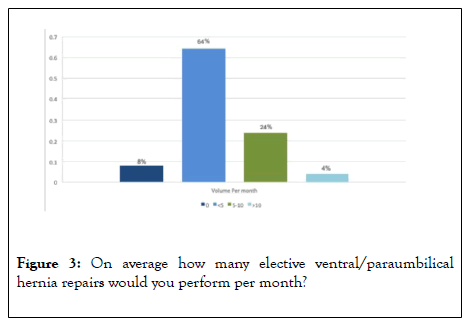
Figure 3: On average how many elective ventral/paraumbilical hernia repairs would you perform per month?
In relation to the surgical technique, defect size influenced operative choice; for defects less than 3 cm, 60% surgeons performed primary tissue repair, 35% used mesh and 5% managed conservatively. 86% performed open approach with only 11% using a laparoscopic Transabdominal pre-peritoneal (TAPP) and 1% a laparoscopic extended total extraperitoneal pre-peritoneal (E-TEPP) approach.
For defects measuring 3-10 cm, 93% used mesh, 4% employed conservative management and 3% used primary tissue repair without mesh augmentation. 51% would do an open repair, 30% laparoscopic TAPP and 1% laparoscopic E-TEPP (Figure 4).
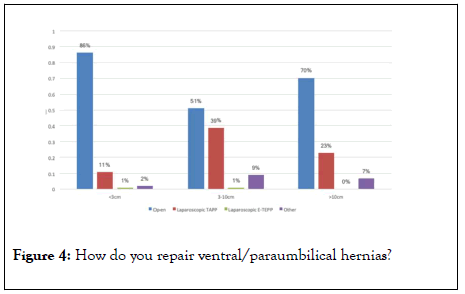
Figure 4: How do you repair ventral/paraumbilical hernias?
In large hernias with a defect greater than 10 cm, 90% favoured mesh augmentation, the remaining 10% favouring conservative management. An open approach was favoured by 70% of respondents with 23% opting for laparoscopic TAPP and remaining 7% choosing ‘other’.
When asked about their choice of mesh, 57% reported using synthetic mesh, 40% used synthetic semi absorbable and 3% a biological mesh. Mesh placement was evenly distributed between onlay (32%) sublay/extraperitoneal (34%) and intraperitoneal (34%) (Figures 5-8).
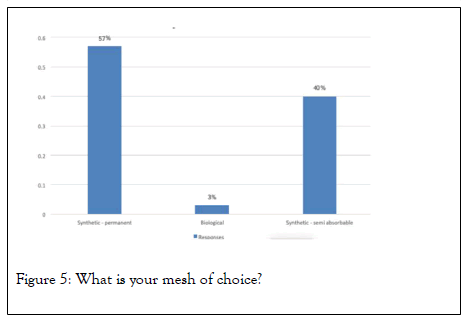
Figure 5: What is your mesh of choice?
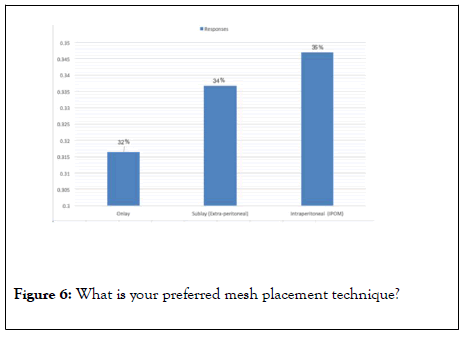
Figure 6: What is your preferred mesh placement technique?
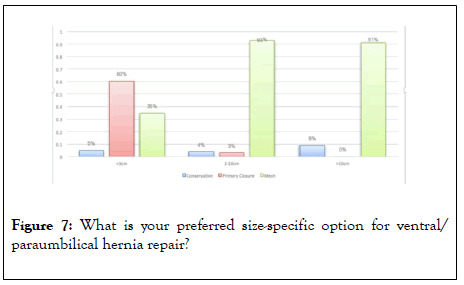
Figure 7: What is your preferred size-specific option for ventral/ paraumbilical hernia repair?
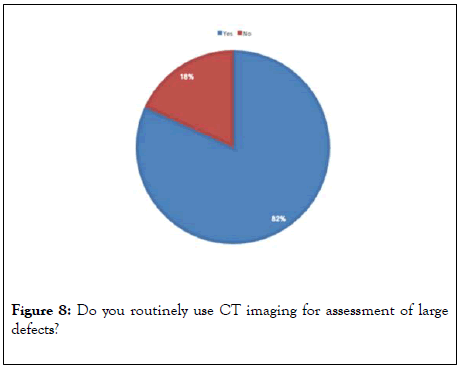
Figure 8: Do you routinely use CT imaging for assessment of large defects?
Use of components separation was 4% in defects less than 10 cm and 59% in defects greater than 10 cm. notably, 37% of respondents report that they do not perform component separation. Of those who do use this technique 57% perform an open anterior component separation, 36% open posterior/ transverses abdominus release (TAR), 3% perform endoscopic anterior release and just 3% opting for laparoscopic posterior components separation/TAR.
Lastly when asked about the usage of Computed Topography (CT) in the assessment of hernias with large defects, 82% reported routine usage.
Discussion
This original quantitative research explores the current management of ventral herniation by surgeons in the republic of Ireland. There is a pattern of low volume practice with the majority of surgeons performing less than 5 repairs per month. Current literature suggests that high volume practice is associated with better outcomes in ventral hernia repair [10] and a comparative study of inguinal hernia repair demonstrated a significantly higher recurrence rate for general surgeons who are not specialists as compared with hernia specialists [11].
Internationally, there has been a trend over the last 25 years towards minimally invasive techniques [12]. In Ireland, open surgery remains the preferred procedure, regardless of defect size, although laparoscopic repair was utilized by a third of surgeons for the repair of medium sized defects and case series from regional centers have been reported with favorable results [13]. This trend seems to mirror recent SAGES guidelines suggesting laparoscopic repair has less surgical site complications in medium sized defects, whereas open repair may be advantageous compared to laparoscopy in small and large hernias due to the associated higher conversion rates and potentially suboptimal outcomes. The predominant use of primary tissue repair for small defects is therefore unsurprising although some studies advocate the use of mesh even for small defects [14].
One third of respondents regularly utilized onlay. This practice should be reconsidered; a recent review of mesh augmentation revealed recurrence rates of 12.9% with onlay mesh in comparison to 5.8% with retromuscular placement [15].
Open anterior component separation was favoured by the majority of respondents; there are valid concerns regarding the operation however, mainly due to risks of devascularization and tissue flap necrosis. In a 2018 review wound complications are reported to be as high as 50%, which compelled the author to suggest that the classic open anterior component technique should be abandoned in favour of an endoscopic anterior approach, perforator sparing anterior approach or alternatively posterior component separation [16]. Recent systematic review of open, endoscopic and laparoscopic techniques suggests that the open anterior approach has the highest recurrence rate at 11.9% although a similar rates of surgical site occurrence [17]. The valid concerns in relation to anterior component separation and the data from this study may suggest reevaluation of our current practice is urgently required given the absence of national data reporting outcomes.
The routine use of CT is prevalent and while there is currently insufficient evidence to advocate this practice, it is acknowledged that for detecting occult defects particularly in obese patients, post traumatic hernias or in recurrent hernias that CT may be valuable [13,18,19].
Conclusion
This study is the first attempt, to our knowledge, to evaluate current practices for ventral hernia repair in Ireland. The marked increase in available surgical techniques can be overwhelming, particularly in the absence of clear consensus or guidelines. This study clearly demonstrates deviation from international trends. In the absence of high quality research and without a mechanism to monitor and evaluate our outcomes we are in a vulnerable position and we strongly advocate for the prompt implementation of a national registry.
REFERENCES
- Kossler-Ebs JB, Grummich K, Jensen K, Hüttner FJ, Müller-StichB, Seiler CM, et al. Incisional Hernia Rates After Laparoscopic or Open Abdominal Surgery-ASystematic Review and Meta-Analysis. World J Surg. 2016; 40: 2319-2330.
- Rosen MJ. Atlas of abdominal wall reconstruction. 1st Edn. 2017.
- Dietz UA, Wiegering A,Germer CT. Indications for laparoscopic treatment of large incisional hernias. Chirurg. 2015; 86: 338-345.
- Mikami DJ, Melvin WS, Murayama MJ, Murayama KM. Impact of minimally invasive surgery on healthcare utilization, cost, and workplace absenteeism in patients with Incisional/Ventral Hernia (IVH). Surg Endosc. 2017; 31: 4412-4418.
- Alam NN, Narang SK, Pathak S, Daniels IR, Smart NJ. Methods of abdominal wall expansion for repair of incisional herniae: A systematic review. Hernia. 2016; 20: 191-199.
- Stechemesser B, Jacob DA, Schug-Paß C,Köckerling F.Herniamed: An internet-based registry for outcome research in hernia surgery. Hernia. 2012; 16: 269-276.
- Kyle-Leinhase I,Köckerling F,Jørgensen LN, Montgomery A, Gillion JF, Rodriguez JAP, et al., Comparison of hernia registries: The CORE project. Hernia. 2018; 22: 561-575.
- HelgstrandF, Jorgensen LN. The Danish Ventral Hernia Database-A valuable tool for quality assessment and research. Clin Epidemiol. 2016; 8: 719-723.
- Poulose BK, Roll S, Murphy JW, Matthews BD, Heniford BT, Voeller G, et al., Design and implementation of the Americas Hernia Society Quality Collaborative (AHSQC): Improving value in hernia care. Hernia. 2016; 20: 177-89.
- Chattha A, Muste J, A Patel. The impact of hospital volume on clinical and economic outcomes in ventral hernia repair: An analysis with national policy implications. Hernia. 2018; 22: 793-799.
- Gilbert AI, Graham MF, Young J, Shaw K. Closer to an ideal solution for inguinal hernia repair: Comparison between general surgeons and hernia specialists. Hernia. 2006; 10: 162-168.
- Köckerling F, D Berger JO Jost. What is a certified hernia center? The example of the German hernia Society and German society of general and visceral surgery. Frontiers in Surgery. 2014; 1(26).
- De Marchi J, Sferle FR, Hehir D. Laparoscopic ventral hernia repair with intraperitonealonlay mesh-results from a general surgical unit. Ir J Med Sci. 2019; 188: 1357-1362.
- Heniford BT. SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc. 2016; 30: 3161-3162.
- Wassenberg D, Zarmpis N, Seip N, Ambe PC. Closure of small and medium size umbilical hernias with the Proceed Ventral Patch in obese patients: A single center experience. Springer Plus. 2014; 3: 686.
- Sosin M, Nahabedian MY, Bhanot P. The Perfect Plane: A Systematic Review of Mesh Location and Outcomes,Update 2018. PlastReconstr Surg. 2018; 142: 107S-116S.
- Scheuerlein H, Thiessen A, Schug-Pass C, Köckerling F. What do we know about component separation techniques for abdominal wall hernia hepair? Front Surg. 2018; 5: 24.
- Cornette B, De Bacquer D, Berrevoet F. Component separation technique for giant incisional hernia: A systematic review. Am J Surg. 2018; 215: 719-726.
- Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc. 2014; 28: 2-29.
Citation: Jennifer M (2020) Ventral Hernia Repair: A National Survey in the Republic of Ireland. J Surg Anesth 4:131.
Copyright: © 2020 Jennifer M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.