PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
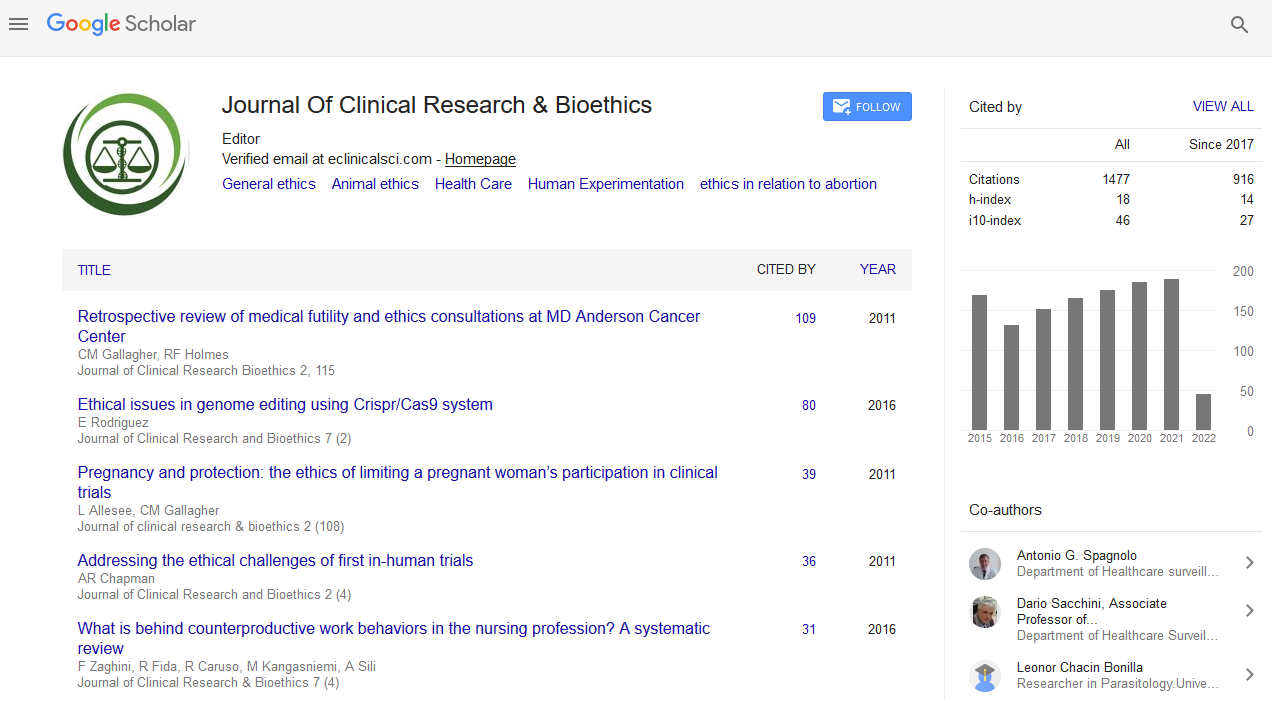
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 11, Issue 4
To Tell or Not? The Omission of Truth Becomes a Lie!
Hina Aslam1*, Mehdi Hayat Khan2, Saba Iqbal3 and Muhammad Arfan Ishaque42Nursing Instructor, Shalamar Nursing College, Lahore, Pakistan
3King Edward Medical University, Mayo Hospital, Lahore, Pakistan
4Hameed Latif Hospital, Lahore, Pakistan
Received: 17-Jul-2020 Published: 07-Aug-2020, DOI: 10.35248/2155-9627.20.11.356
Abstract
Truth telling (veracity) in health care is considered as a prominent phenomenon contributing to so many other ethical obligations. The principle of truth telling can influence the right of patients and their families of getting correct information about the disease, treatment plan, and other treatment options available. This paper discusses the HCP’ s decision for beneficence of patient life and keeping patient stigmatized status confidential which creates conflict between three principles. It is believed that truth telling and disclosing correct diagnosis should be done only if there is no risk to patient s life. Ethical principles conflicting here are the beneficence, confidentiality and veracity. HCP was in confusion that weather to tell the truth by disclosing the immoral act of the patient in front of her family, which could result in losing patient’s life or keep it confidential.
Keywords
Veracity; Benefience; Confidentiality; Ethical Dilemma; Health Care Provider (HCP)
Scenario
A 23 years old female patient was brought to the surgical emergency department by her mother with severe abdominal pain. On initial examination, perforation of appendix was suspected. Later on, detailed laboratory and radiological investigations revealed that it was a case of ruptured ectopic pregnancy. It was quite surprising and unexpected in a young unmarried girl. The disclosure of the fact of being pregnant to her family could bring a disaster in patient’s life. When the patient came to know about the reality, she begged not to disclose her pregnancy in front of her family due to serious foreseeable consequences. Keeping in mind the cultural norms, the surgical team decided to hide the true diagnosis from the family and went for emergency laprotomy. The laprotomy was done with the consent of perforation of appendix rather than declaring ectopic pregnancy.
Assumptions of Ethical Dilemma
In the above scenario, disclosure of true diagnosis of ectopic pregnancy could bring a threat to patient’s life. It is uncommon to conceive a pregnancy by an unmarried girl in Islamic culture and considered a great sin. On contrary, the discloser of real diagnose could have ended up with a destruction of that patient’s life. Therefore, the HCPs decided to proceed with the declaration of wrong diagnosis, which was necessary to save her life.
According to Beauchamp and Childress, beneficence refers to “ an obligation to act for the benefits of others ” while confidentiality is a term often refer to non-disclosure of patients’ information in front of others. On the other hand, truth telling (veracity) in health care is considered as a prominent phenomenon contributing to so many other ethical obligations [1]. Some concepts, which the veracity can influence, are right of family and patients to receive correct information, right to choose treatment, and right to know about the other possible treatment options. In current scenario, HCPs ’ decision for saving and keeping patient’s stigmatized status confidential was found conflicting with the principle of truth telling (veracity). On the other hand, there was a risk to patient’s life after truth telling because family could have refused to give consent of surgery.
Introduction
Ethical principles are the basic tools to measure the standards of health care decisions. Ethical principles work to enhance the quality of care in health care organizations. Ethical decision making is a key part of Health care practice for better functioning of the health care organizations [2]. The role of ethics and basic ethical principles in health care organization is vital and cannot be underestimated. Ethics can assist health care organizations and individuals to identify and work through ethical dilemmas or issues using a standardized decision making approach. Organizations ascend through effective ethical decision making, integration of process and support systems which enable organizational culture to develop [3]. The situation above is having some ethical and moral questions because having a pregnancy by an unmarried female is considered a sin, a taboo, and a moral misconduct. HCPs in our culture usually refuse to provide services to such illegal cases in pregnancy termination [4].
From the Lens of Health Care Provider
Health care providers (HCPs) are always committed to do everything in the best interest of their patients, as it is mentioned in their oath “I will apply, for the benefit of the sick, all measures which will be required” [5]. In the current case, HCPs followed two ethical principles to favor the patient. Firstly, the HCP’s decision to go for emergency surgery was completely in favor of patient and there was no other interest except patient’s beneficence. Secondly, the sensitive information of the patient was kept secret to respect the confidentiality of patient. In health care organizations, confidentiality has been viewed as one of the important part of ethics. Respecting the patients’ confidentiality and privacy, are considered the rights of patients.
If we analyze, in our case scenario, HCPs maintained confidentiality but the truth kept hidden from the patient’s family on patient’s request. So confidentiality was maintained but veracity was violated while providing beneficence. It is an interesting interplay of three ethical principles i-e confidentiality, veracity and beneficence. After keeping the patient ’ s information confidential, HCPs were able to save the patient’s life. On the other hand, the principle of veracity was violated by HCP. Even though, it was considered ethical to avoid the discloser of information on patient’s request.
From the Lens of Patient
Morality is a set of values and beliefs regarding human behavior and lifestyle choices. It refers to certain code of conduct to regulate human life. It plays a vital role in everyone's social, spiritual and religious life [6]. In this case, morality was not shown by the girl because she was brought to hospital in life threatening condition due to her immoral act. HCPs could have refused to provide services. However, that was matter of life and death and God knows that weather girl had done that immoral act deliberately or was rapped. On the other hand, moral health is not considered as the part of definition of “health”. HCPs therefore, opted for saving the patient’s life without taking care of the societal norms and religious beliefs [7].
From the Lens of Family
Two positions discussed above were in favor of patient. Here is the third aspect where it seems like injustice was done with the family members by conveying false information. According to the law of Pakistan, and other sociocultural norms, all kinds of abortion are considered as illegal. In Pakistan, abortions are only allowed where it was necessary to save mother’s life [8]. Literature suggests that truth telling (veracity) plays a key role to integrate with the patient, family, and health care team. The principle of truth telling is interrelated to so many other ethical and moral obligations among the medical professionals. One of them is the right of patient and family to receive correct information about the disease. In this case patient’s right is stronger than that of family [9].
Similarly, HCPs were in agreement with the patient and they violated the principle of veracity.
My Position
HCPs are primary communication channel among patients and their families. HCPs spend more time with patients and deal with difficult patient situations more frequently. I strongly agree with the decision of HCP’s team in this case, according to King and Lee [10]. if by telling a lie, someone’s life can be saved, the lie and deception is morally acceptable.
Recommendations
Hospitals and health care management must have ethical committee. In such sensitive issues, help and guidance must be taken from that team rather taking individual decisions. Other possibilities should also be discussed, such as the role of law and orders. HCPs are supposed to play a holistic and family centered role in dealing with such patients. Otherwise, young generation could get negative lesson by such favors. It was good that the patient’s life was saved but one should also feel the need of counseling this patient to avoid engaging in such unethical sinful practices in future.
Conclusion
Rules are meant to be broken. In health care settings, it stands true when there is a matter of life and death. Nothing is important more than saving a pernicious life, whatever the situation is, whatever the rules are. HCPs must strive for saving the lives of patients, as the patient’s life is above all ethical principles.
REFERENCES
- Beauchamp TL, Childress JF. Principles of biomedical ethics: Oxford University Press, USA. 2001.
- Yaqoob A, Muhammad SA. Healthcare organizational silence: Who is accountable? J Clin Res Bioeth. 2017;9(1).
- Frolic F. Ethics Framework. Hamilton Heath Sciences. 2010.
- Rehan N. Attitudes of health care providers to induced abortion in Pakistan. J Pak Med Assoc. 2003;53(7).
- Abdel Ghany T, Shater, A Negm M, Al Abboud M, Elhussieny N. Efficacy of botanical fungicides against Curvularia lunata at molecular levels. J Plant Pathol Microb. 2015;6(289):2.
- Hocutt M. Morality: What in the World Is It? Behavior and Ph. 2010;31-48.
- Lamb C. Conscientious objection: Understanding the right of conscience in health and healthcare practice. The New Bioethics. 2016;22(1): 33-44.
- Idrees S, Qarani WM. Saving life or trumping autonomy? A question for health care providers. J Clin Res Bioeth. 2015;6(5):1.
- Sisk B, Frankel R, Kodish E, Isaacson JH. The truth about truth-telling in American medicine: A brief history. The Permanente Journal. 2016;20(3):74.
- King F. D., Lee A. Consuming surfaces: Decadent aesthetics in the debt to pleasure. Journal of Modern Literature. 2019;42(3):151-168.
Citation: Aslam H, Khan MH, Iqbal S , Arfan Ishaque M (2020)To Tell or Not? The Omission of Truth Becomes a Lie! J Clin Res Bioeth. 11:356. doi: 10.35248/2155-9627.20.11.356.
Copyright: © 2020 Aslam H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.