Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 5, Issue 4
The Preventive Effect of Subhypnotic Dose of Propofol in Preventing Laryngospasm in Children undergoing Adeno-tonsillectomy in Addis Ababa Hospitals, Addis Ababa Ethiopia. A Prospective Cohort Study
Geresu Gebeyehu1*, Betelhem Ayele2, Adugna Aregawi1 and Zewetir Ashebir12Department of Anesthesia, College of Health Sciences, Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia
Received: 14-May-2021 Published: 04-Jun-2021, DOI: 10.37421/2684-1606.2021.5.151
Abstract
Introduction: Laryngospasm is defined as the sustained closure of the vocal cords, well-known problem typically occurring immediately following tracheal extubation. Incidence of laryngospasm is as high as 25% in patients undergoing tonsillectomy and adenoidectomy. Propofol is an intravenous drug use for the induction of general anesthesia and for moderate to deep sedation, which is also known to strongly suppress airway responses. At a lower concentration than the anesthetic dose, propofol may help to reduce or prevent laryngospasm after extubation in pediatric patients. This study assessed the effectiveness of propofol in preventing laryngospasm during adeno-tonsillectomy surgery under general anesthesia.
Methods: This prospective cohort study conducted on 66 pediatric patients aged up to 9 years and underwent elective adenotonsilectomy under general anesthesia from december 2019-March 2020 at Tikur anbessa specialized hospital, Yekatit 12 hospital and Menilke hospital. The data was recorded as group P if anesthesia providers gave propofol 0.5 mg/kg one minute before extubation or group C if the anesthesia provider just extubate without giving propofol. The incidence and severity of laryngospasm was compared between the two groups. Moreover, vital signs were compared among the two groups. Data was analyzed using student t test and Mann–Whitney U test for normally and non-normally distributed data respectively and chi-square test for categorical data. P-value less than 0.05 considered as statistically significant.
Results: The occurrence of laryngospasm between propofol group and control group was 9.1% and 42.4% respectively (p<0.05). The comparison of severity of laryngospasm and vital sign changes showed no significant difference between the groups. (p>0.05).
Conclusion: Subhypnotic dose of propofol (0.5 mg/kg) decreases the occurrence of laryngospasm upon tracheal extubation in children undergoing tonsillectomy with or without adenoidectomy. We recommend anesthetists to use 0.5 mg/kg of propofol one minute before extubation to prevent post extubation laryngospasm.
Keywords
Adeno-tonsillectony; Extubation; General anesthesia; Laryngospasm; Propofol
Introduction
The most dreaded respiratory complications during pediatric anesthesia occurs due to low FRC, small residual volume and exaggerated tendency to airway closure making to become easily hypoxic and other secondary effects. Moreover, a high vagal tone in children can be rapidly changed to apnea and laryngospasm in a state of any stimulating events such as secretion, tracheal intubation or extubation and pulmonary aspiration. Hypoxia and laryngospasm accounts for approximately 30% of respiratory events during pediatric anesthesia and this problem expected to be high in surgical problems involving respiratory tracts. Oral procedures promoting an increased secretion with blood in the airways, like tonsillectomy and laryngeal surgery, are associated with a higher risk. Some studies have reported a 21% to 26% incidence of laryngospasm after adenoidectomy and tonsillectomy, which are the most common surgical procedures performed in children [1,2].
Even though laryngospasm is essentially a protective reflex, the presence of these reflex results in impairment to adequate breathing, and it becomes a sudden obstruction of upper airway. It has a feature that the airway closure is maintained even after the initial causal stimulus disappears. This blockage can lead to hypoxemia, negative-pressure pulmonary edema, pulmonary aspiration, and cardiac arrest [3,4].
Surgical removal of enlarged tonsils with or without adenoids has become most popular treatment for a complicated tonsilopharyngitis that may complicate with rheumatic heart diseases. An increased infection with group A beta hemolytic streptococcus bacteria in developing world made adenotonsilectomy as a standard preventive treatment for such complications [5]. Airway complications after adenotonsilectomy are many fold since surgical procedure is too close to airway itself, bleeding into the airways is very common, stimulation during surgery and instrumentation by surgical devices can make these complications especially laryngospasm more commonly occur during tracheal extubation. Since laryngospasm has severe and fatal consequences it demands prompt treatment when it is diagnosed, many investigators have concentrated their efforts on preventing this reflex [6].
Approaches to airway complication after adenotonsilectomy should be immediate and fast enough to avoid secondary effects; overall achieving smooth tracheal extubation would be superior to all but it would be difficult to have smooth extubation with already stimulated airways. Treatment of perioperative laryngospasm usually involves the removal of the stimulus, including: stopping the surgical procedure, administering CPAP with 100% O2, deepening the plane of anesthesia, if it is caused by a painful stimulus, short-acting opioids should be administered; and we have to consider the use of succinylcholine if the stated measures so far were not effective. Succinylcholine has long been a preferred pharmacologic agent for treating laryngospasm because of its rapid onset and short duration of action although very effective at treating laryngospasm, comes with potential serious side effects such as bradycardia and arrhythmias [2,4,5].
Treatments are often not without side effects and usually put additional anesthetic cost on the patients. we can reduce or avoid these side effects of treatments by using different preventive approaches and also decrease the incidence of laryngospasm by using physical interventions to prevent it following adenotonsilectomy including emphasizing hemostasis at the time of surgery, gentle suctioning of the oropharynx just before extubation to remove any retained blood and secretions, tracheal extubation in either a very deep plane of anesthesia. Agents like magnesium sulfate, lidocaine, and intermediate muscle relaxants, such as rocuronium can prevent laryngospasm in pediatric patients. Recently, low-dose propofol was shown to relieve laryngeal spasm in most children following tonsillectomy Propofol at the anesthetic dose is known to strongly suppress airway responses. The reports suggest that it may help to prevent laryngospasm during extubation in pediatric patients it depresses the laryngeal reflex, producing a low incidence of obstructive problems [7-10].
Methods
This is an institution based multicenter, prospective cohort study conducted in Tikur Anbessa specialized, Yekatit 12 and Minilik II specialized hospitals from December 2019 to March 2020. The study was conducted after obtaining an institutional ethical approval for the study. A total of 66 participants whom were scheduled for elective adenotonsilectomy under general anesthesia were recruited into this study after taking informed consent from the parents or other family members of the children. The aim and objectives of the study were also explained to the parents before they sign an informed consent.
Sample size for study was calculated using double population proportion formula for comparison of two proportions based on the following assumptions: significance level 5%(α=0.05), power of study (1-β) of 80%. We used the study conducted in Kuwait by, because we lack related study conducted in our country. Based on this, the incidence of laryngospasm within control group (not took propofol) is 20% and propofol group is 6.6% [7]. Taking this into consideration, the sample size was calculated as:
(P1.q1+p2.q2)f(a.B)/(p1-p2)2=n1=n2
n1=n2= (0.2 × 0.8+0.06 × 0.94)(1.96.0.84)2/(0.06-0.2)2=30.
n=Sample size in each group
α =significance level (1.96)
1-β=power of study at 80% (0.84)
q1= 1-p1
q2=1-p2
P1= incidence of laryngospasm in control group
P2= incidence of laryngospasm in propofol group
Adding attrition rate of 10% to each group made the sample size in each group 33. Thus, the total sample size was 66.
Systematic random sampling technique was used to select participants. Children with recent URTI, history of asthma, predicted difficult intubation, and those whom induced with propofol were excluded from the study. Anesthesia management for adenotonsilectomy patients in study hospitals are usually carried out by BSc and MSc anesthesia professional. Per practice all patents were preoxygenated with 100% oxygen via face mask before induction of anesthesia under standard monitors applied and after baseline vital signs is recorded. They induce anesthesia with IV inductional agent in children who preferred IV induction. After induction of anesthesia, suxamethonium 1-2 mg/kg) IV is given to facilitate tracheal intubation. The anesthesia maintained with isoflurane or halothane in oxygen. After recovery from suxamethonium some anesthetists administer non-depolarizing muscle relaxant and the others continue with the suxametonium. All patients receive intravenous fluids per protocol using preexisting guidelines to replace preoperative deficits and provide standard maintenance fluids. As routinely practiced patients took intraoperative analgesia fentanyl 1-2 mcg/ kg or petidine 0.5-1 mg/kg. At the end of the procedure, blood and secretions in the pharynx is carefully suctioned, inhalational anesthesia is discontinued and the child is allowed to breathe 100% oxygen. When the child started to react to the tracheal tube (swallowing, grimacing and making purposeful movements), most anesthetists used to give small dose of propofol (0.5 mg/ kg) sixty seconds before they perform tracheal extubation believing its potent depressant effect on airway reflexes will make extubation smooth while some of them just extubate them without giving propofol fearing there may be prolonged sedation during extubation. Therefore, patients were grouped based on whether small dose propofol was given by anesthetist on charge at one minute to extubation. At the end of surgical procedures and confirmed hemostasis, oropharynx was suctioned carefully and throat pack removed, tracheal extubation took place. During and immediately after extubation, the occurrence and severity of laryngospasm was graded as a condition occurring within 2 min after extubation, characterized by the following findings [11].
(i) Stridor;
(ii) Total occlusion of the cords (respiratory efforts with no air movement);
(iii) Cyanosis with evidence for airway obstruction at the level of vocal cords
Vital signs were also recorded; the pulse, mean arterial blood pressure and oxygen saturation at different time interval at the end of surgery, after extubation, 1 min after propofol, 5 min, 10 min, 15 min, 20 min and 30 min post operatively.
The data was analyzed using SPSS version 20 after it is cleaned and coded. The numeric data was described in terms of mean and SD, median (IQR) or frequencies when appropriate. Comparison of numerical variable between study groups using independent t test for normally distributed data and Mann-Whitney-U test for non-normally distribution. Chi square test was employed to compare for categorical variables. Paired t test was used to compare the before and after propofol vital signs. A statistical Significance was determined at p value less than 0.05.
Results
A total of 66 ASA I and II patients were finally involved in the study and grouped into propofol group and control group. The comparison of demographic and operative characteristics including age, sex, weight, ASA status, duration of surgery, estimated blood loss and presence of OSA showed no statistically significant difference among the groups (Tables 1 and 2).
| Group p | Group c | P-value | |
|---|---|---|---|
| Age (yrs) | 5.64 ± 2.572 | 5.94 ± 2.499 | 0.629 |
| Sex n: M/F | 17/16 | 17/16 | |
| Weight (kg) | 21.1 ± 5.46 | 21.18 ± 5.37 | 1.000 |
| ASA n (%) I II |
32(96.6%) | 31(93.9%) | 0.555 |
| 1(3%) | 2(6%) | ||
| Duration of surgery | 44.39 ± 8.54 | 45.15 ± 7.23 | 0.699 |
| Blood loss | 63.67 ± 16.89 | 64.24 ± 16.25 | 0.889 |
| Presence of OSA | 24(72%) | 19(57.6%) | 0.301 |
Table 1: Demographic and operative characteristics between group p and group c of patients who undergone Tonsillectomy at Tikur Anbessa specialized, Menilk II referal and yekatit 12 Hospital , Addis Ababa, Ethiopia.
| Induction | Group p | Group c | P-value |
|---|---|---|---|
| Thiopental | 17(51%) | 18(54%) | 0.52 |
| Ketamine | 16(48%) | 15(45%) | |
| Mantainance | |||
| Halotane | 13(39%) | 13(39.3%) | 0.59 |
| Isoflurane | 20(60%) | 20(60%) | |
Table 2: Operative characteristics between group p and group c of patients who undergone Tonsilictomy at Tikur Anbessa specialized, Menilik II referal and Yekatit 12 Hospital , Addis Ababa, Ethiopia.
Incidence and severity of laryngospasm
Fourteen patients in the control group developed laryngospasm (42.4%), in the propofol group, three children suffered laryngospasm (9.1) (Figure 1). The overall incidence of laryngospasm was significantly lower in the propofol group versus control group (P<0.05) (Table 3).
| Parameter | Group P(n=33) | Group C(n=33) | P-value | |
|---|---|---|---|---|
| Incidence | 3(9.1%) | 14(42.4%) | ||
| Stridor | 2(66.7%) | 6(42.9%) | ||
| Laryngospasm | Occlusion | 1(33.3%) | 7(50%) | 0.002 |
| Cyanosis | 0(0%) | 1(5.9%) |
Table 3: Severity of laryngospasm in patents between group P and group C patients who undergone Tonsilictomy at Tikur Anbessa specialized, Menilik II referal and Yekatit 12 Hospital, Addis Ababa, Ethiopia.
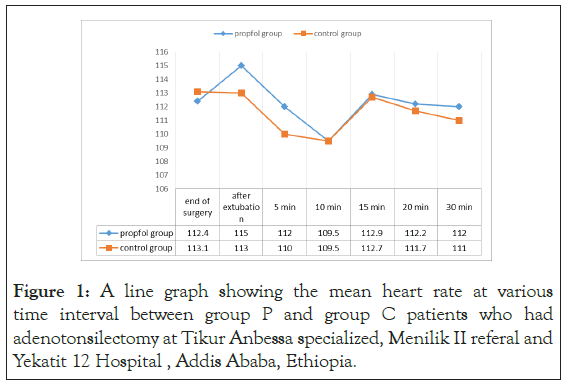
Figure 1: A line graph showing the mean heart rate at various time interval between group P and group C patients who had adenotonsilectomy at Tikur Anbessa specialized, Menilik II referal and Yekatit 12 Hospital , Addis Ababa, Ethiopia.
Hemodynamic and respiratory parameters
Mean heart rate: There was no statistically significant difference in mean heart rate at end of surgery, after extubation, 5 min, 10 min, 15 min, 20 min, and 30 min. (p=0.656,0.370,0.572,0.991, 0.967, 0.84 and 0.814 respectively) in both groups as shown in (Figure 1).
Mean arterial pressure: There was no statistically significant difference in mean arterial blood pressure end of surgery, after extubation, 5 min, 10 min, 15 min, 20 min, and 30 min. (p=0.857, 0.950, 0.561, 0.929, 0.929, 0.706 and 0.980 respectively) in both groups (Figure 2).
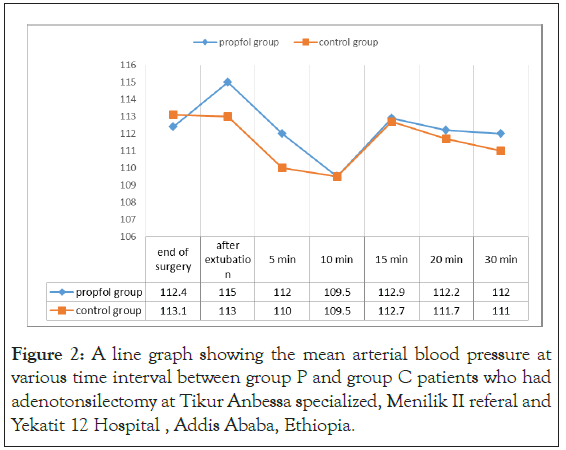
Figure 2: A line graph showing the mean arterial blood pressure at various time interval between group P and group C patients who had adenotonsilectomy at Tikur Anbessa specialized, Menilik II referal and Yekatit 12 Hospital , Addis Ababa, Ethiopia.
Arterial oxygen saturation
The Mann Whitney U test showed that the median SpO2 score was comparable in the 15 min, 20 min and 30 minute after extubation between the control and propofol groups. But the median SpO2 score were lower in control group at the end of surgery, immediately after extubation, 10 min and 15 min after extubation hours and there was statistical significant difference at the end of surgery, immediately after extubation and 10 min after extubation postoperatively between propofol and control groups (p<0.005) (Table 4).
| SPO2 in (Median and IQR) | Group P | Group C | P-value |
|---|---|---|---|
| End of surgery | 100(99-100) | 99(99-100) | 0.004 |
| After extubation SPO2 | 98(97-99) | 95(90-99) | 0.005 |
| 5 min SPO2 | 98(97-99) | 96(93-99) | 0.001 |
| 10 min SPO2 | 99(98-99) | 97(95-98) | 0.001 |
| 15 min SPO2 | 98(98-99) | 97(97-99) | 0.071 |
| 20 min SPO2 | 99(98-99) | 98(97-99) | 0.123 |
| 30 min SPO2 | 99(98-99) | 99(97-100) | 0.473 |
Table 4: Comparison of respiratory parameter between group P and group C group analyzed by Mann Whitney U test at Tikur Anbessa specialized, Menilik II referal and Yekatit 12 Hospital, Addis Ababa, Ethiopia.
Discussion
Upper airway surgeries especially adenotonsilectomy is associated with high incidence of laryngospasm and the reported incidence of laryngospasm during emergence in patients undergoing tonsillectomy and adenoidectomy under general anesthesia ranges from 21% to 26% when no prophylactic is given. Laryngospasm also represent approximately 30% of respiratory events during pediatric anesthesia [12].
From short review above, key patient data’s like the demographic characteristics (age, sex, weight, ASA status), agents used for induction and maintenance, duration of surgery, blood loss and presence of OSA were not statistically significant between the groups, p>0.05.As it has different magnitude on the incidence and severity of laryngospasm [13].
This study showed that low dose propofol is effective in lowering the rate of post extubation laryngospasm. The overall incidence of laryngospasm was 9.1% in propofol and 42.4% control which was significantly lower in the propofol group versus control group (P<0.05).This result coincides with randomized double blind study done in Egypt by, on comparison of the effectiveness of small dose of propofol and midazolam in preventing laryngospasm following extubation they conclude that intravenous administration of small dose of propofol or midazolam before tracheal extubation decreases the incidence and severity of laryngospasm in adult patients undergoing oropharyngeal surgeries. In another randomized, double blind study done in Kuwait by. on the efficacy of a subhypnotic dose of propofol in preventing post extubation laryngospasm who got 20% control group and 6.6% in propofol which is significantly lower incidence of laryngospasm [7,13].
In contrast to the present study, a randomized, double-blinded control trial study done in Thailand by. Compared the effects of intravenous propofol and propofol with low-dose ketamine on preventing post-extubation cough and laryngospasm among patients awakening from general anesthesia. They found no significant difference in the incidence and severity of laryngospasm between comparison groups. The use of very small dose of propofol might be the reason of the result [14].
Mean arterial pressure was also compared between the two groups in the study and no significant difference in MAP was observed with P>0.05. This finding shows that propofol at low dose has little or no effect on blood pressure. This is consistent with a randomized double blind study conducted in Korea by, which revealed sub hypnotic dose of propofol (0.3 mg/kg) for the prevention of coughing in adults during emergence had no significant effect on arterial pressure. However, a study done in Egypt by has shown a contrary result to this. Their study showed significant decrease in mean arterial pressure and significant increase pulse rate after propofol administration up to 5 min after extubation. The most likely reason for this could be due to slightly large dose of propofol (0.8 mg/kg) usage by the investigators [15,16].
Arterial oxygen saturation was compared between the groups and revealed a significant difference at the end of surgery, immediately after extubation and 10 min after extubation SpO2 between propofol and control groups (p<0.005). The possible explanation for this would be due to high occurrence of laryngospasm which led to oxygen desaturation in the control group in the first 10 minutes.
The strength of this study is it tried to explore the most neglected approaches to respiratory events during airway surgeries and its limitation was inability to conduct double blind control study.
Conclusion
Based on the findings of this study, we conclude that use of subhypnotic dose of propofol (0.5 mg/kg) could successfully minimize the risk of post-extubation laryngospasm without affecting the hemodynamic and respiratory parameters in children undergoing tonsillectomy with or without adenoidectomy. We recommend anesthetists in practice to use subhypnotic dose (0.5 mg/kg) of propofol one minute before extubation to prevent post extubation laryngospasm.
Funding Disclosure
This study was supported by Addis Ababa University
Acknowledgements
Our special thanks for Addis Ababa University, College of Health Sciences, and Department of Anesthesia for their cooperation to invest our time in this study and those who provided constructive support to this research project.
REFERENCES
- Isono S. Developmental changes of pharyngeal airway patency: Implications for pediatric anesthesia. Pediatr Anesth 2006;16(2):109-122.
- AB. Hobaika, MN. Lorentz. Laryngospasm. Rev Bras Anestesiol. 2009; 59(4): 487-495.
- Enrique Hernández-Cortez E. Update on the management of laryngospasm. J Anesth Crit Care Open Access.2018;8(2):1–6.
- Shawn Collins. Prevention and Treatment of Laryngospasm in the Pediatric Patient. AANA Journal. 2019 ;87(2): 145-151.
- Ralph F. Wetmorea. Surgical management of the tonsillectomy and adenoidectomy patient. World J Otorhinolaryngol Head Neck Surg. 2017; 3(3): 176–182.
- Ludlow CL. Central nervous system control of the laryngeal muscles in humans. Respir Physiol Neurobiol 2005; 147(2): 205-222.
- Batra YK, Ivanova M, Ali SS, Shamsah M, Al Qattan AR, Belani KG. The efficacy of a subhypnotic dose of propofol in preventing laryngospasm following tonsillectomy and adenoidectomy in children. Paediatr Anaesth. 2005; 15(12):1094-1097.
- Mc Keating K, Bali IM, Dundee JW. The effects of thiopentone and propofol on upper airway integrity. Anaesthesia. 1988; 43(8): 638-640.
- Sundman E, Witt H, Sandin R, Kuylenstierna R, Bodén K, Ekberg O, et al. Pharyngeal function and airway protection during subhypnotic concentrations of propofol, isoflurane, and sevoflurane: Volunteers examined by pharyngeal videoradiography and simultaneous manometry. Anesthesiology. 2001; 95(5): 1125-1132.
- Hae Jin Pak. Effect of a small dose of propofol or ketamine to prevent coughing and laryngospasm in children awakening from general anesthesia. Korean J Anesthesiol. 2011; 60(1): 25-29.
- Tsui BCH, Wagner A, Cave D, Elliott C, Hamdy EI H, Malherbe S. The incidence of laryngospasm with a no touch extubation technique after tonsil-lectomy and adenoidectomy. Anesth Analg. 2004; 98(2): 327–329.
- Gil Gavel, Robert WM Walker. Laryngospasm in anaesthesia. Continuing Education in Anaesthesia Critical Care & Pain. 2014; 14(2): 47–51.
- Amira A. Shaban. Effect of small dose propofol or midazolam to prevent laryngospasm and coughing following oropharyngeal surgeries. Egyptian Journal of Anaesthesia. 2016; 32(1): 13–19.
- Yanipan Chungsamarnyart, Pairart J, Munjupong S. Comparison of the effects of intravenous propofol and propofol with low-dose ketamine on preventing postextubation cough and laryngospasm among patients awakening from general anaesthesia. J Perioper Pract. 2020; 30(4): 83-108.
- Soon Yong Jung, Hee Bin Park, Ju Kim. The effect of a subhypnotic dose of propofol for the prevention of coughing in adults during emergence from anesthesia with sevoflurane and remifentanil. Korean J Anesthesiol. 2014; 66(2): 120-126.
- Nawfal M, Baraka A. Propofol for relief of extubation laryngospasm. Anaesthesia. 2002; 57(10): 1028-1036.
Citation: Gebeyehu G, Ayele B, Aregawi A, Ashebir Z (2021) The Preventive Effect of Subhypnotic Dose of Propofol in Preventing Laryngospasm in Children undergoing Adeno-tonsillectomy in Addis Ababa Hospitals, Addis Ababa Ethiopia. A Prospective Cohort Study. J Surg Anesth. 5:151.
Copyright: © 2021 Gebeyehu G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.