Citations : 1817
Dentistry received 1817 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 10, Issue 1
The Clinical Efficacy of an Ultrasonic Device with Built-In Electronic Apex Locator when Preparing Vertical Root Fracture Lines Through the Root Canal
Megumi Kudou*, Youji Motoki, Kana Inoue, Saori Tanaka, Hirofumi Miyaji, Masamitsu Kawanami and Tsutomu SugayaReceived: 26-Dec-2019 Published: 10-Jan-2020, DOI: 10.35248/2161-1122.20.10.549
Abstract
The aim of the present study was to compare treatment outcomes of preparing vertical root fractures from within the root canal using ultrasonic devices with and without a built-in electronic apex locator before sealing the fracture gap. A total of 178 teeth with vertical root fractures, in which the fracture lines had been prepared from within the root canal using an ultrasound device before sealing the gap, were classified into S and E groups based on the device used. In the S group, an apex locator was used with the ultrasonic device. Probing depth and bone defect were significantly improved after treatment as compared with before treatment in both groups. Moreover, probing depth was significantly shallower in the S group as compared with the E group. Our findings indicate that using an ultrasonic device with a built-in electronic apex locator may improve treatment outcomes.
Keywords
Vertical root fracture; Electronic apex locator; Ultrasonic device; Gap sealing; 4-META/MMA-TBB resin
Introduction
When tooth roots are vertically fractured, periodontal tissue destruction progresses rapidly and tooth extraction is generally indicated in the case of a single-rooted tooth, whereas root resection and hemisection are indicated in the case of multirooted teeth [1-4]. Ricucci et al. [5] reported the formation of biofilm in the cracks. Biofilms, which also form within fracture gaps in vertical root fractures, are responsible for the inflammation in periodontal tissue. Kimura et al. [6] histopathologically evaluated the roots of beagles with experimental vertical fractures and found that a short time after fracture, bacteria that had grown in the root canal and fracture gap were the main cause of periodontal inflammation regardless of the probing depth. They also reported that there was almost no downward growth of epithelium although a pocket probe penetrated the inflammatory connective tissue. Tomita et al. [7] fractured the tooth roots of beagles and sealed the fracture gap with 4-methacryloxyethyl trimellitate anhydride/methyl methacrylate-tri-n-butyl borane (4-META/MMA-TBB) resin. They found that sealing the fracture gap improved inflammation that had occurred in the periodontal tissue, and that bone loss around the fracture line was repaired with a shallower probing depth.
Some studies reported successful clinical preservation with 4- META/MMA-TBB resin bonding [8-13]. Masaka [8] reports cases of fractured roots that were preserved for 10 years through 4- META/MMA-TBB resin bonding. In addition, Sugaya et al. [9] performed the same bonding treatment using 4-META/MMATBB resin in 23 teeth with vertical root fractures and found that 18 teeth (78%) were successfully preserved over a 6-74 month follow-up period. Hayashi et al. [10] extracted 26 teeth with vertical root fractures, which they replanted after bonding, and 14 teeth were successfully preserved over a follow-up period of 4-74 months. However, methods of bonding from within the root canal have been found to result in insufficient improvement in periodontal pockets and bone loss [9]. Possible causes of this are that bacteria are prone to remain in the fracture gap and that fully bonding the fracture gap from within the root canal is difficult.
Preparing the fracture line from within the root canal using an ultrasonic device can improve scalability by enabling both removals of infected dentin in the fracture gap and formation of a space for the resin to penetrate [14]. In the abovementioned experiment, the fracture line was prepared while measuring the impedance between the ultrasonic tip and artificial periodontal ligament using an ultrasonic device with a built-in electronic apex locator. The findings stated that the appropriate use of an automatic apical stop system where ultrasonic vibrations stop when the set value of the electronic apex locator is reached would be effective at preventing excessive or insufficient preparation.
The aim of the present study was therefore to compare treatment outcomes of preparing vertical root fractures from within the root canal using ultrasonic devices with and without a built-in electronic apex locator.
Materials and Methods
This retrospective study was carried out in teeth diagnosed with vertical root fracture and in which the fracture gap was sealed from within the root canal at Hokkaido University Hospital, Department of Endodontics and Periodontics between 1994 and 2012. The study was approved by the Institutional Review Board of Hokkaido University Hospital for Clinical Research (011-0305). Items examined were patient age, sex, tooth type, fracture site, pretreatment, and posttreatment probing depth and bone defect from dental radiographs. If the same tooth had 2 or more fracture lines, the line with the deeper probing depth was subject to examination.
Fracture lines were prepared under a microscope without irrigation using an ultrasonic device. The debris was intermittently washed away with irrigation. The teeth were classified into an S group and E group according to the ultrasonic device used. In the S group, an ultrasonic device with a built-in electronic apex locator (Solfy ZX or Solfy F, J. Morita MFG. Corp., Kyoto, Japan) and a Micro Endo File (Mani, Tochigi, Japan) were used. The Solfy F and Solfy ZX both have the same vibration frequency and electronic apex locator system. In the E group, the ENAC 10WA (Osada Electric Co., Ltd., Tokyo, Japan) and Ultrasonic SC Point 4-17 (Osada Electric Co., Ltd., Tokyo, Japan) were used. In both groups, the ultrasonic tip diameter was 0.25 mm with the same 0.05 taper. The automatic apical stop system was set to 1.0 in the Solfy ZX and Solfy F and preparation was performed with the tip only vibrating in areas larger than the set value by slowly touching the tip from one end of the fracture line to the other. In the S group, preparation was stopped at the point where 1.0 was shown no matter the part of the fracture line. In the E group, preparation was performed until continuous, slight bleeding throughout the entire fracture line was seen under a microscope.
When bleeding or pus discharge from the fracture gap did not stop after stopping fracture line preparation in either group, calcium hydroxide was applied and the root canal was temporarily sealed. In cases where the indirect method was performed, calcium hydroxide was applied to the root canal after post-site preparation and impression-taking and the root canal was temporarily sealed. At the next visit, the root canal was thoroughly washed using an ultrasonic device and the fracture gap was bonded and sealed if pus discharge and bleeding from the fracture gap had disappeared. To start, 10% citric acid with 3% ferric chloride solution (Green activator, Sun Medical Co., Ltd, Shiga, Japan) was injected into the root canal, and 10 seconds later, the root canal was washed using a three-way syringe fitted with a 24G needle, after which the water was removed by suction and the root canal was dried using a mild air blow. 4-META/MMA-TBB resin (Super Bond, Sun Medical Co., Ltd, Shiga, Japan) was mixed with monomer solution, a catalyst, and polymer powder according to the manufacturer ’ s instructions and loaded in a syringe (Terumo, Tokyo, Japan). The mixture was injected into the root canal, after which a cast post or fiber post resin core (i-TFC system, Sun Medical Co., Ltd, Shiga, Japan) was inserted. In cases where the direct method was used, a fiber post was inserted into the root canal filled with Super Bond and the core was built up with a composite resin (i-TFC system, Sun Medical Co., Ltd, Shiga, Japan).
In both groups, teeth underwent re-evaluation 1-2 months after bonding treatment. The clinical examination involved checking probing depth, presence of sinus tract or abscesses, and improvement of bone defect based on radiographs. Improvement of bone defect was classified into the disappearance of bone defect, a decrease of bone defect and no change or increase of bone defect. Crown prostheses were fabricated at the time of re-evaluation, except in cases with deepened probing depth, presence of sinus tract or abscesses and no improvement in the bone defect.
For statistical analysis, the Chi-square test, Mann-Whitney U test and Wilcoxon signed-rank test were performed using SPSS Statistics Version 21 (IBM, Armonk, NY, USA).
Results
Patients in the S group included 29 men and 63 women aged 54.5 ± 12.4 years (mean ± standard deviation), while patients in the E group included 27 men and 42 women aged 54.6 ± 10.1 years. Two patients belonged to both groups, bringing the total number of subjects to 159. The most common tooth type in either group was the maxillary premolar, although no significant difference was seen between the 2 groups (p=0.41) (Table 1). The most common fracture region in the longitudinal axial direction in either group was fracture from the apical region, with no significant difference between the 2 groups (p=0.87) (Table 2).
| Maxillary | Mandibular | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Incisor | Canine | Premolar | Molar | Incisor | Canine | Premolar | Molar | ||
| S group | 15 | 4 | 33 | 12 | 1 | 0 | 16 | 24 | 105 |
| E group | 7 | 1 | 24 | 10 | 0 | 3 | 11 | 17 | 73 |
| Total | 22 | 5 | 57 | 22 | 1 | 3 | 27 | 41 | 178 |
Table 1: Tooth types.
| Complete fracture | Incomplete fracture | |||
|---|---|---|---|---|
| Apical region | Mid-region | Cervical region | ||
| S group | 26 | 46 | 2 | 31 |
| E group | 21 | 28 | 1 | 23 |
| Total | 47 | 74 | 3 | 54 |
Table 2: Fracture region in the longitudinal axial direction.
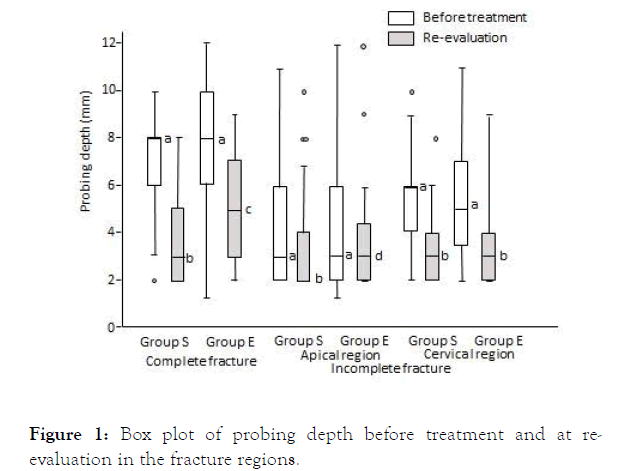
Pretreatment probing depth did not differ significantly between the two groups at any of the fracture sites (complete fracture: p=0.37, apical region fracture: p=0.18, cervical region fracture: p=0.94). However, a comparison of pretreatment and reevaluation probing depth revealed significantly shallower depths at re-evaluation in all fracture regions in the S group (p<0.001). In the E group, probing depth at re-evaluation was significantly shallower in complete fractures and cervical region fractures (p<0.022). Furthermore, an intergroup comparison of probing depth at re-evaluation revealed that complete fractures were significantly shallower in the S group than the E group (p=0.014) (Figure 1).
Figure 1. Box plot of probing depth before treatment and at reevaluation in the fracture regions.
A significant difference between a and b, and a and c (Wilcoxon signed-rank test, p<0.001)
A significant difference between b and c (Mann-Whitney U test, p=0.004)
Pretreatment bone defects were seen in the S group in 17 of the 26 teeth with complete fracture (65.4%), 40 of the 46 teeth with apical region fracture (87.0%), and 19 of the 31 teeth with cervical region fracture (61.3%). In the E group, pretreatment bone defects were seen in 13 of the 21 teeth with complete fracture (61.9%), 21 of the 28 teeth with apical region fracture (75.0%), and 15 of the 23 teeth with cervical region fracture (65.2%). No significant differences were seen between the two groups (p>0.28). Comparison of bone defects before treatment and at re-evaluation revealed significant improvement in complete fractures (p=0.020) and cervical region fractures (p=0.002) in the S group, and in cervical region fractures (p=0.019) in the E group (Tables 3-5). A comparison of the state of improvement of bone defects of both groups at re-evaluation revealed no significant difference (p>0.19).
| Disappearance | Decrease | No change/increase | Total | |
|---|---|---|---|---|
| S group | 3 | 11 | 3 | 17 |
| E group | 5 | 4 | 4 | 13 |
Table 3: Improvement of bone defects in complete fracture with pretreatment bone defect.
| Disappearance | Decrease | No change/increase | Total | |
|---|---|---|---|---|
| S group | 18 | 15 | 7 | 40 |
| E group | 11 | 7 | 3 | 21 |
Table 4: Improvement of bone defects in apical region fracture with pre-treatment bone defect.
| Disappearance | Decrease | No change/increase | Total | |
|---|---|---|---|---|
| S group | 7 | 7 | 5 | 19 |
| E group | 6 | 5 | 4 | 15 |
Table 5: Improvement of bone defects in cervical region fracture with pre-treatment bone defect.
Abscesses remained or formed during the period up to reevaluation in 1 apical region fracture and 2 cervical region fractures in the S group, and in 1 complete fracture and 2 cervical region fractures in the E group. Sinus tracts were present in 1 complete fracture and 3 apical region fractures in the S group, and in 3 apical region fractures in the E group.
Discussion
Cases in which the fracture gap had already widened and granulation tissue had penetrated by the time a definitive diagnosis of vertical fracture was made were excluded from the sample population of this study. This was because granulation tissue hinders the removal of infected dentin in the fracture line through the root canal and granulation tissue, exudate, and bleeding during sealing of the fracture gap make proper bonding of the resin difficult.
An ultrasonic tip with a diameter of 0.25 mm and taper of 0.05 was used to prepare fracture lines. Preparing the fracture line with a tapered tip exposes the dentinal tubules with an oblique angle on the dentin surface even if the fracture is parallel to the dentinal tubule. This is reported to improve bond strength after bonding [14] and using a tapered tip is considered an effective means of preventing recurrent fracture.
Fracture lines were prepared in the S group using an automatic apical stop system set to a value of 1.0. The manufacturer specifies a set value of 0.5 as standard when determining root canal length. However, in experiments where fracture lines are prepared in extracted teeth, setting a value of 0.5 unavoidably results in excessive preparation; thus, the closest value that allows adequate root preparation is reported to be 1.0 [15]. That is why the automatic apical stop was set at 1.0 in this study.
The results of the present study indicated the possibility of different treatment outcomes depending on the fracture region. Complete fractures, apical region fractures, and cervical region fractures were therefore analyzed separately. Mid-region fractures were present in few cases and were thus excluded from the analysis. Probing depth was significantly shallower at reevaluation compared with before treatment in all fracture regions in the S group and in complete fractures and cervical region fractures in the E group. When the periodontal tissue is inflamed due to periodontitis, the periodontal probe can easily penetrate into the inflamed connective tissue through the epithelial attachment, whereas it would not reach the epithelial attachment if there is no inflammation [16,17]. In addition, a study that histopathologically examined periodontal tissue destruction over time in the roots of beagles where vertical root fractures had been made, found that hardly any epithelial down growth occurred regardless of the probing depth and that a probe could easily penetrate deep into the periodontal tissue when inflammation had occurred as a result of vertical root fracture [6]. The findings of these studies strongly suggest that probing depth may have improved in the present study because before treatment the probe penetrated into the periodontal tissue along the fracture line due to inflammation, and after treatment, the probe could no longer penetrate due to improvement of inflammation.
An intergroup comparison of probing depth at the re-evaluation revealed that the depth was significantly shallower in the complete fracture of the S group as compared with the E group. The shape of the ultrasonic tip was the same in both groups, which makes it highly likely that the presence of an automatic apical stop system in conjunction with an electronic apex locator caused differences in pocket improvement. Preparation was considered completed in the E group despite insufficient preparation because any bleeding caused by the tip coming into contact with the periodontal ligament flowed along the fracture line. Meanwhile, the impedance ratio measured at different wavelengths by the automatic apical stop system in the S group stopped tip vibration once a set value was reached. Root canal length found by measuring the impedance ratio with 2 wavelengths is not easily affected by conductivity within the root canal [18,19], and even if a small amount of bleeding occurred as a result of preparation, the impact was negligible in the S group, likely resulting in higher preparation accuracy than in the E group, where completion of preparation was determined by visual inspection. In the S group, the probing depth after pretreatment differed significantly in all fracture regions, whereas in the E group, no significant improvement was seen in the apical region. Significant improvement was also seen in bone defects after treatment in complete fractures and cervical region fractures in the S group, but a significant difference was only seen in cervical region fractures in the E group. This may indicate that the apical stop system has a greater impact in the apical region where fracture lines are less likely to prepare. However, there were cases in the S group where no improvement in probing depth or bone defect was seen. These findings suggest that preparing fracture lines even with an apex locator may not be accurate; this may have led to residual infection in fracture gaps and incomplete closure. Irrigation with antiseptic or antibacterial solutions may be an effective means of rectifying this problem, although the further investigation into this matter is needed. Biofilm may have also formed on the outer root surface around the fracture line, as it does in the cementum surface around the apical foramen in apical periodontitis [20-26]. In such cases there are limitations to treatment from within the root canal, making surgical treatment such as intentional replantation necessary.
Calcium hydroxide was injected into the root canals of many cases with a deep pretreatment probing depth and bone defects. Calcium hydroxide has a disinfectant action and is effective in controlling inflammation [27,28]. however, the use of calcium hydroxide is unlikely to affect the difference in treatment outcomes because the same usage criteria were applied in both groups. Calcium hydroxide also inhibits adhesion by remaining on the dentin surface [29,30]. While this residual calcium hydroxide can result in the formation of dead space and refractures, long-term observation is needed to determine if clinical outcomes are affected. The effectiveness of injections of calcium hydroxide into the root canal in treatment for vertical root fracture is a complex problem that requires further study.
This treatment led to disappearance or decrease in bone defects in a large number of cases. The lack of downgrowth of the pocket epithelium in these cases may have caused the repair of bone along with the removal of infection from the fracture line. This is consistent with the results of an animal experiment in which fracture gaps were successfully sealed and the bone defect repaired a short time after vertical root fracture because the amount of downgrowth of the epithelium was very small [7]. Moreover, no significant difference in bone defect improvement was seen between the 2 groups in this study. This is because it takes time for radiolucency to be reduced even after periodontal inflammation has resolved; the follow-up period of 1-2 months after fracture gap bonding until re-evaluation may have been short. However, long-term observation can lead to findings of refracture and deterioration of the periodontal pocket, which may obfuscate the repair of fracture lines and the effects of bonding and sealing. That is why the present study comprised a follow-up period of 1-2 months to evaluate the initial improvement of inflammation. The long-term prognostic evaluation will be needed to determine if this method is effective for the treatment of vertical root fractures. Bone defects were also evaluated in the present study by dental radiographs, although the use of Cone Beam Computed Tomography (CBCT) might further improve the accuracy of evaluation of apical region bone defects [31]. Artifacts caused by metals near the cervical region may, however, inhibit the evaluation of bone morphometry. A more accurate evaluation may be possible in cases with no artifacts by using CBCT.
Conclusion
The fact that improvement was seen in many cases in the present study suggests that the method of bonding and sealing after preparation of the fracture line from within the root canal could be developed as a treatment for vertical root fracture. Our findings indicate that using an ultrasonic device with a built-in electronic apex locator may improve treatment outcomes as compared with a simple ultrasonic device.
Acknowledgement
The authors declare that they have no conflicts of interest related to this study.
REFERENCES
- Polson AM. Periodontal destruction associated with vertical root fractures. J Periodontol. 1977;48:27-32.
- Pitts DL, Natkin E. Diagnosis and treatment of vertical root fractures. J Endod. 1983; 98:338-346.
- Lommel TJ, Meister F, Gerstein H, Davies E, Tilk MA. Alveolar bone loss associated with vertical root fractures. Oral Surg Oral Med Oral Oathol. 1978; 45:909-919.
- Barkhordar RA. Treatment of vertical root fracture: a case report. Quintessence Int. 1991;22:707-709.
- Ricucci D, Siqueira JF Jr, Loghin S, Berman LH. The cracked tooth: histopathologic and histobacteriologic aspects. J Endod. 2015; 41:343-352.
- Kimura K, Sugaya T, Kato H. Histopathological study of periodontal destruction after vertical root fractures. Jpn J Periodontol. 2000;42:255-266.
- Tomita M, Sugaya T, Kawanami M. Periodontal healing after intra-oral and extra-oral bonding treatment of experimental vertical root fracture. Jpn J Conserv Dent. 2002;45:787-796.
- Masaka N. Long-term observation of fractured tooth roots preserved by adhesion. Adhes Dent. 1995;13:156-170.
- Sugaya T, Kawanami M, Noguchi H, Kato H, Masaka N. Periodontal healing after bonding treatment of vertical root fracture. Dent Traumatol. 2001;17:174-179.
- Hayashi M, Kinomoto Y, Takeshige F, Ebisu S. Prognosis of intentional replantation of vertically fractured roots reconstructed with dentin-bonded resin. J Endod. 2004;30:145-158.
- Kawai K, Masaka N. Vertical root fracture treated by bonding fragments and rotational replantation. Dent Traumatol. 2002;18:42-45.
- Kudou Y, Kubota M. Replantation with intentional rotation of a complete vertically fractured root using adhesive resin cement. Dent Traumatol. 2003;19:115-117.
- Unver S, Onay EO, Ungor M. Intentional re-plantation of a vertically fractured tooth repaired with an adhesive resin. Int Endod J. 2011;44:1069-1078.
- Liu J, Kawada E, Oda Y. Effects of surface treatment and joint shape on microtensile bond strength of reattached root dentin segments. J Prosthet Dent. 2004;91:46-54.
- Kawabata S, Sugaya T, Kawanami M. Ultrasonic grinding of vertical fractured gap surfaces using an electric apex locater. Hokkaido J Dent Sci. 2013:53-61.
- Listgarten MA, Mao R, Robinson PJ. Periodontal probing and the relationship of the probe tip to periodontal tissues. J Periodontol. 1976;47:511-513.
- Armitage GC, Svanberg GK, Löe H. Microscopic evaluation of clinical measurements of connective tissue attachment levels. J Clin Periodontol. 1977;4:173-190.
- Kobayashi C, Suda H. New electronic canal measuring device based on the ratio method. J Endod. 1994;20:111-114.
- Gordon MP, Chandler NP. Electronic apex locators. Int Endod J. 2004;37:425-437.
- Tronstad L, Barnett F, Riso K, Slots J. Extraradicular endodontic infections. Endod Dent Traumatol. 1987;3:86-90.
- Tronstad L, Kreshtool D, Barnett F. Microbiological monitoring and results of treatment of extraradicular endodontic infection. Endod Dent Traumatol. 1990;6:129-136.
- Kiryu T, Hoshino E, Iwaku M. Bacteria invading periapical cementum. J Endod. 1994;20:169-172.
- Lomçali G, Sen BH, Cankaya H. Scanning electron microscopic observations of apical root surfaces of teeth with apical periodontitis. Endod Dent Traumatol. 1996;12:70-76.
- Noiri Y, Ehara A, Kawahara T, Takemura N, Ebisu S. Participation of bacterial biofilms in refractory and chronic periapical periodontitis. J Endod. 2002; 28(10):679-683.
- Leonardo MR, Rossi MA, Silva LA, Ito IY, Bonifácio KC. EM evaluation of bacterial biofilm and microorganisms on the apical external root surface of human teeth. J Endod. 2002;28:815-818.
- Wang J, Jiang Y, Chen W, Zhu C, Liang J. Bacterial flora and extraradicular biofilm associated with the apical segment of teeth with post-treatment apical periodontitis. J Endod. 2012;38:954-959.
- Sathorn C, Parashos P, Messer H. Antibacterial efficacy of calcium hydroxide intracanal dressing: a systematic review and meta-analysis. Int Endod J. 2007;40:2-10.
- Mohammadi Z, Dummer PM. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011;44:697-730.
- Barbizam JV, Trope M, Teixeira EC, Tanomaru-Filho M, Teixeira FB. Effect of calcium hydroxide intracanal dressing on the bond strength of a resin-based endodontic sealer. Braz Dent J. 2008;19:224-227.
- Lee BS, Lin YC, Chen SF, Chen SY, Chang CC. Influence of calcium hydroxide dressing and acid etching on the push-out bond strengths of three luting resins to root canal dentin. Clin Oral Investig. 2014;18:489-498.
- Venskutonis T, Plotino G, Juodzbalys G, Mickevičienė L. The importance of cone-beam computed tomography in the management of endodontic problems: a review of the literature. J Endod. 2014;40:1895-1901.
Citation: Kudou M, Motoki Y, Inoue K, Tanaka S, Miyaji H, Kawanami M, et al. (2020) The Clinical Efficacy of an Ultrasonic Device with Built-In Electronic Apex Locator when Preparing Vertical Root Fracture Lines Through the Root Canal. Dentistry 10:549. doi: 10.35248/2161-1122.20.10.549
Copyright: © 2020 Kudou M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited