Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
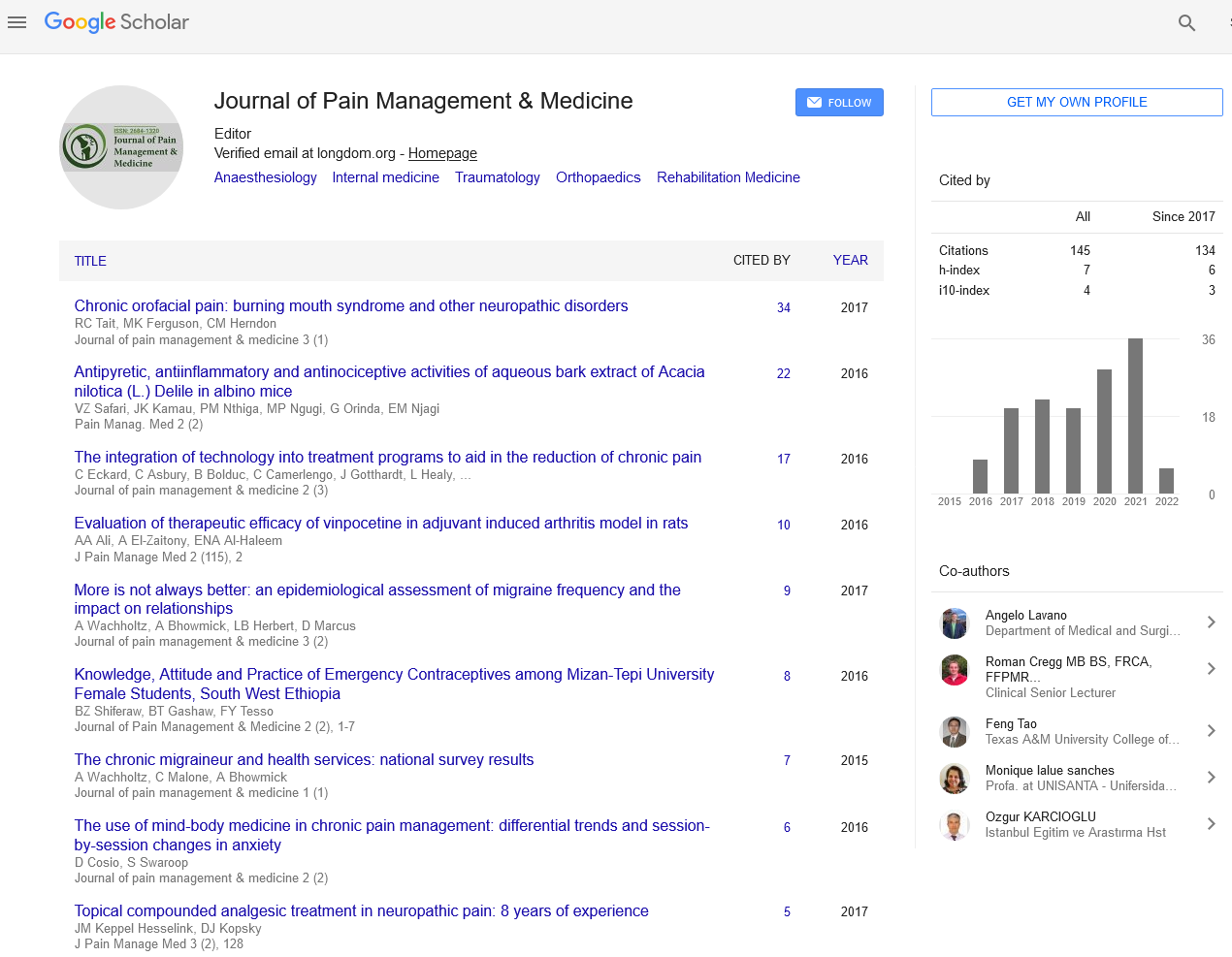
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2020) Volume 6, Issue 2
Spinal Canal Drug Administration for Chronic Pain
Rupesh Kumar Singh*Received: 16-Jul-2020 Published: 28-Jul-2020, DOI: 10.35248/2684-1320.20.6.141
Commentary
The presentation of intrathecal narcotics has been viewed as one of the most significant discoveries in torment the board in the previous three decades. By imbuing a modest quantity of narcotic analgesics into the cerebrospinal liquid in closeness to the receptor locales in the spinal line, significant absense of pain might be accomplished while saving a portion of the reactions brought about by high portion fundamental narcotics. Spinal canal medicate conveyance (IDD) has been progressively used since 1980's, at first in patients with disease torment, and along these lines in patients with incessant, immovable non-dangerous agony. Alongside this fundamentally expanded use of IDD for extreme nonmalignant torment, the subpopulation of patients with implantable Spinal canal imbuement siphons has expanded significantly.
In any case, there have not been any rules, suggestions, or even agreement proclamations from all significant torment social orders either inside or outside US, relating to the usage of narcotics for postoperative agony control when these patients need to experience surgeries, for example, hip or knee substitution and so forth. The past clamor (2007) in endeavor to achieve an accord conclusion in helping managing these troublesome circumstances was lamentably overlooked [1].
The normal, worn out inquiries are: When patients who are on intrathecal narcotic mixture for incessant torment go for surgeries, for example, hip substitution or knee substitution, and so forth., what ought to be finished with their intrathecal narcotic routine? Do we go up, descend, proceed, or cease their routine intrathecal narcotic implantation before medical procedure? What would it be advisable for us to accomplish for their postoperative torment a short time later? Would we be able to in any case utilize routine modalities, for example, intravenous patient-controlled absense of pain (IV PCA) or epidural absense of pain in such patients for their postoperative torment control? Would we be able to utilize extra intrathecal narcotic for postoperative torment control since the patients as of now have intrathecal catheters embedded?
One clinical methodology has been: keeping the intrathecal narcotic imbuement the equivalent pre-and post-medical procedure, while using IV narcotic PCA for post employable agony [1]. In the course of the last 7-8 years, more than 60 patients, while on a similar routine intrathecal narcotic implantation routine for ceaseless non-harmful agony, experienced surgeries, for example, lumbar combination, cervical combination, all out hip substitution, complete knee substitution, and so on, and got IV narcotic PCA (morphine, hydromorphone) for post employable torment, without experiencing any inconveniences or reactions of narcotic overdose. (Individual perception) This methodology has additionally been used by some other interventional torment authorities who oversee interminable torment patients on IDD treatments. (Dr. J. Patrick Couch, Dr. Tao Chen, individual correspondences) It appears to be sensible to accept that the routine intrathecal implantation fulfills the narcotic prerequisite for the ceaseless torment part, while the IV narcotic PCA meets the extra narcotic necessity for intense postoperative agony because of medical procedure.
In late 2008, Grider et al [2] announced their experience of effective perioperative torment control in 3 patients on routine IDD for ceaseless torment, while utilizing IV PCA narcotics for perioperative torment.
As far as I could possibly know, there has been no other writing other than the over two references [1,2] address such circumstances. Strikingly, both of the above reports agreed on keeping up same IDD mixture portion for constant agony while starting IV PCA narcotic for intense postoperative torment. In any case, this end clearly ought not be deciphered as "principles of care".
The absence of writing, rules, suggestions, or accord proclamations have brought about doctors including torment authorities, anesthesiologists, and specialists having little pieces of information when managing these uncommon circumstances. This is particularly significant from clinical legitimate viewpoint, as difficulty/antagonistic impacts do occur, regardless of whether great medication is drilled.
Clearly, further exploration work and collaboration in defining some handy rules are in critical need, to support our patients and ourselves. The motivation behind this publication is, ideally, to achieve some past due consideration and some exploration exertion to assist us with handling this undeniably experienced yet "ignored" quandary.
REFERENCES
- Ruan X. Acute pain management in patient on intrathecal opioid infusion for chronic pain. Pain Physician. 2007;10:779-780.
- Grider JS, Brown RE, Colclough GW. Perioperative management of patients with an intrathecal drug delivery system for chronic pain. Anesth Analg. 2008;107:1393-1396.
Citation: Rupesh KS (2020) Spinal Canal Drug Administration for Chronic Pain. J Pain Manage Med 6: 141. doi: 10.35248/2684-1320.20.6.141
Copyright: © 2020 Rupesh KS. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.