Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2021) Volume 0, Issue 0
Special Considerations in the Diagnosis and Treatment of Acute Arterial Occlusion Caused by Tumor Embolization
Rohan HP McLachlan*Received: 09-Aug-2021 Published: 30-Aug-2021, DOI: 10.35248/2329-6925.21.s7.005
Abstract
Tumor embolism differs from other forms of thromboembolism with special considerations for diagnosis and treatment. This report summarises what we know about this unique pathological process and outlines an approach to surgical treatment. With the advent of new endovascular technologies, there may be several different options available for patients and each individual case needs to be carefully considered given there are no formal guidelines advising the best way to manage this distinct subset of patients.
Keywords
Tumor embolism; Acute ischemia; Acute arterial occlusion; Thrombectomy; Endovascular
Introduction
Thromboembolism is a universally recognised and suspected complication of malignancy. Treatment algorithms for coagulation disorders and associated arterial and venous thrombosis are well established in this context. However, acute arterial occlusion as a result of tumor embolism remains an under recognised entity, usually with catastrophic consequences. There are no treatment guidelines and so beyond traditional open thromboemboectomy, surgeons are using novel endovascular technologies with diseasespecific considerations to achieve good results.
Literature of Review
Epidemiology
A defining constituent of any embolic event is the source. In cases of tumor embolism clinicians have learnt to suspect atrial myxoma, a frequent source that confers rates of embolism ranging from 30- 40% [1,2]. A review of patients with intracranial arterial occlusion due to tumor embolism found that in 77% of cases were of cardiac origin [3]. However, non-myxomatous arterial emboli do occur and there are reported cases of tumor embolism from almost all cancer types. Lung tumors are the most frequently non-myxomatous source of tumor embolism reported. In a review of 104 cases, 76% of events were in patients with primary (46 patients) or secondary (33 patients) lung cancer [4]. In a vast majority of cases embolization occurred after surgical resection of the lung mass. This emphasizes the importance of monitoring for end-organ ischemia in cancer patients during the peri-operative period. Peripheral pulse status should be documented before surgery and assessed frequently afterwards. Brain, bowel, kidney and liver function should also be closely monitored. Tumor embolism should always be considered in patient with lung cancer who present with acute arterial embolism, particularly if their disease is advance or they are post-resection.
Pathophysiology
When lung cancer embolizes, it most frequently reaches the arterial system via the pulmonary veins [5,6]. Although there are reported cases of direct invasion through the left atrial wall and aortic arch, this mechanism is rare because direct invasion requires constant, contiguous connection between the tumor and site of invasion [1, 7]. Once tumor reaches the pulmonary veins it may extend into the left atrium. Acknowledgment of this pathological process is important given that up to 4% of advanced lung cancer patients have involvement of the pulmonary veins and up to 1% may have extension into the left atrium [8]. Once present in these structures macroscopic fragments of tumor can detached from the main tumour mass. In majority of cases this is related to surgical manipulation during resection but it may also occur spontaneously, related to cardiac contraction [3,9].
These fragments embolize throughout the arterial tree and occlusion results in acute ischemia of the downstream organ or tissue. Akin to thrombus, tumor emboli most frequently lodge in arterial bifurcations where the lumen of the vessel narrows. Around 50% of reported cases are to the aortic and femoral bifurcations resulting in acute lower limb ischemia. However, there are numerous cases describing embolization to visceral arteries and so end-organ ischemia in this subset of patients should raise suspicion for tumor embolism [9]. The most feared anatomical destination is the middle cerebral artery which appears to be the most common after aortic and femoral bifurcations and is almost always fatal [3,4].
Imaging
Certain patients may be considered high risk for tumor embolization, either due to previous embolization, planned surgical resection or pathoanatomical factors. Transoesophageal echocardiogram (TOE) is the diagnostic investigation of choice for diagnosing pulmonary vein or intracardiac tumour invasion [10]. TOE allows visualization of all four pulmonary veins in 87% of cases, compared to transthoracic echocardiogram which visualises only two pulmonary veins 71% of the time [11]. Patients can thus be identified as high-risk for embolization and the appropriate steps taken to reduce the chance of this devastating complication. These include meticulous surgical planning and dissection, early clamping of the pulmonary veins or early ligation of the pulmonary veins via either a direct in indirect intrapericardial approach [12].
In patients presenting with acute ischemia, computed tomography is utilized to assess the location and extent of occlusion, essential information for operative planning which can then be corroborated in cases that proceed to diagnostic plus therapeutic angiography. Other modalities such as duplex ultrasound and magnetic resonance angiography can be considered but their utility may be limited by time, availability, and user-dependence.
Surgical considerations
Surgeons have been refining techniques to treat arterial occlusion for decades and there is now a plethora of surgical options for patients with acute thromboembolism. Tumor embolism however, is a unique entity and the structural composition of tumor is a critical consideration when deciding on the modality of intervention.
An open approach should be considered in the first instance to ensure complete removal of tumor fragments and reduce the risk of downstream embolization associated with endovascular techniques. Open thromboembolectomy of the aorta, superior mesenteric artery and lower limb vessels have all been reported with resolution of acute ischemia and prevention of long-term ischemic sequelae [4,10,13]. In patients who are deemed at risk of foregut or mesenteric ischemia based on the site of occlusion, an open approach allows for inspection of the abdominal viscera. In some cases, such as embolization to the aorta or femoral bifurcations, a large tumor load mandates an open approach simply because endovascular equipment is not wide enough to retrieve the bulky embolic material (Figure 1). In easy to access anatomical sites such as the upper or lower limb arteries, open surgery may result in faster reperfusion than endovascular methods which can often be technically challenging and requires dynamic intra-operative decision-making.
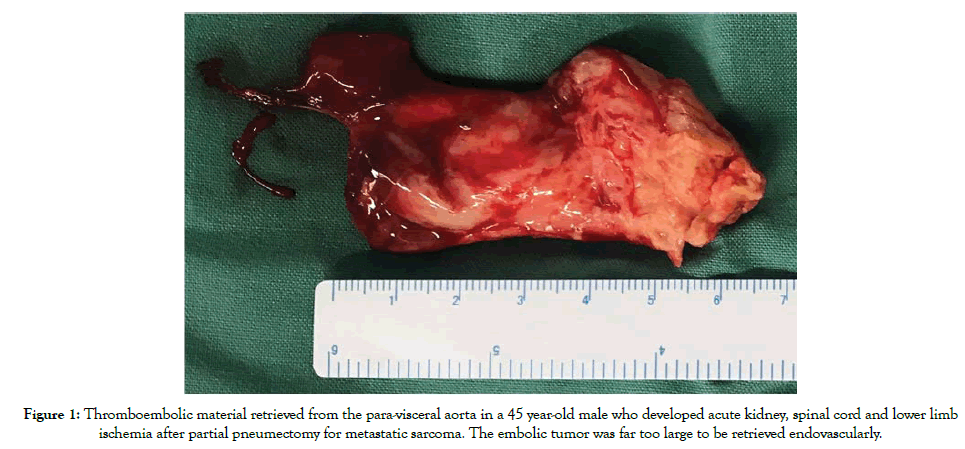
Figure 1: Thromboembolic material retrieved from the para-visceral aorta in a 45 year-old male who developed acute kidney, spinal cord and lower limb ischemia after partial pneumectomy for metastatic sarcoma. The embolic tumor was far too large to be retrieved endovascularly.
Thrombolysis has proven to be an excellent option for patients with acute thromboembolism because it is minimally invasive and concurrently treats macrovascular and microvascular thrombosis. In patients with fresh thrombus and with perfusion time permitting, thrombolysis often achieves excellent clearance of intramural thrombus with a simple percutaneous puncture. Unfortunately, this is not an option for patients with tumor embolism because thrombolytic agents target thrombus, not cancer.
There are endovascular techniques available for retrieval of thromboembolic material in the arterial system. Notable modalities include aspiration thrombectomy and clot retrieval devices. These methods were developed to improve outcomes for patients with acute ischemic stroke. In the early twenty-first century, the only treatment available to these patients was systemic thrombolysis. However, this therapy was limited by a 3-hour treatment window and poor recanalization rates of large vessel occlusion. Chemical thrombolysis was not effective in patients with a larger volume of thrombus, particularly firm cardiac thrombus. Thus, endovascular techniques to physically retrieve rather than chemical degrade thrombus were developed. Endovascular mechanical thrombectomy dramatically improved recanalization rates and decreased haemorrhagic complications in acute stroke patients [14]. These retrieval techniques confer the same advantages in patients with tumour embolism as they do for stroke patients with large volume mural thrombus because the structure of the occlusive material is comparable.
Aspiration thrombectomy is performed by advancing a specialized catheter to the site of occlusion. An external pump produces negative pressure within the catheter and hence aspirates material into the catheter, with or without simultaneous fragmentation. Fragmentation can cause microembolisation which is rarely a significant complication for patient with occlusive thrombus who are receiving concurrent thrombolysis. However, if tumor cells were to embolize downstream it would result in widespread seeding of the cancer and thus simultaneous fragmentation should be used with great caution in this subset of patients.
Clot retrieval devices function on the premise that thrombus can be captured on a catheter-mounted device, often a bare metal stent, and recovered into a sheath. These devices are available in a variety of designs, some of which may be more effective in negotiating a firm, non-friable tumor embolus. These technologies are often augmented with use of a proximal balloon-mounted catheter to arrest antegrade flow and reduce the risk for downstream embolization, the importance of which has been emphasized earlier.
Discussion
Numerous cases report the use of these endovascular techniques to restore flow in the setting of acute arterial occlusion caused by tumour embolism (Figure 2A-2C) [3,15]. These techniques are most commonly employed in anatomically difficult-to-access areas such as the distal internal carotid arteries or renal arteries, or where endorgan infarction occurs quickly. In some cases, multiple techniques were utilised in individual patients. The results are promising with low rates of long-term ischemic sequalae reported. However, longterm prognosis remains poor given the systemic spread of tumor cells and so surgical management should be reserved for patients who will have some reasonable benefit from relief of acute ischemia in the context of an ultimately terminal disease.
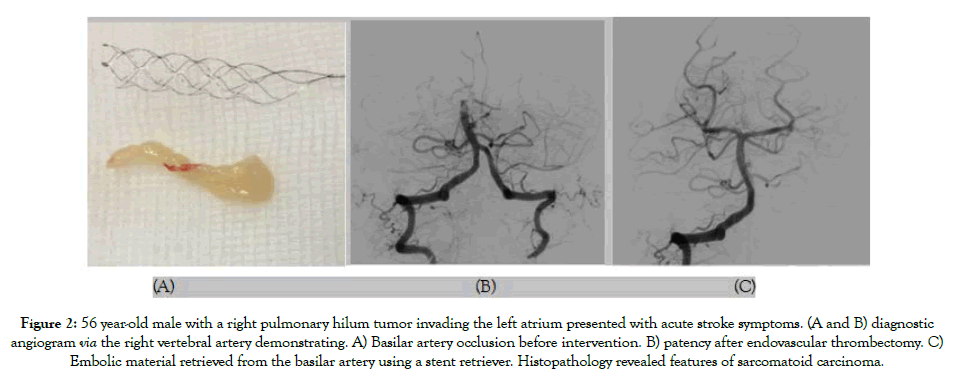
Figure 2: 56 year-old male with a right pulmonary hilum tumor invading the left atrium presented with acute stroke symptoms. (A and B) diagnostic angiogram via the right vertebral artery demonstrating. A) Basilar artery occlusion before intervention. B) patency after endovascular thrombectomy. C) Embolic material retrieved from the basilar artery using a stent retriever. Histopathology revealed features of sarcomatoid carcinoma.
Conclusion
Tumor embolism should be suspected in cancer patients with acute arterial occlusion, particularly in patients with lung cancer who are post-resection. Open thromboembolectomy should be consider in the first instance, although there are endovascular therapies available that may be more appropriate in certain clinical situations, and these have demonstrated promising results in restoring end-organ perfusion. Long-term outcomes remain poor however, due to systemic seeding of tumor cells.
REFERENCES
- Lioudaki S, Kontopodis N, Palioudakis S, Koutsopoulos AV, Drositis I, Ioannou CV. Acute aortic occlusion due to tumor embolism in a patient with lung malignancy. SAGE Open Med Case Rep. 2017;5:2050313X17720627.
- Tsao J-H, Lo H-C, How C-K, Yen DH-T, Huang C-I. Embolic occlusion of the aorta caused by cardiac myxoma. Resuscitation. 2010;81(5):511.
- Tsurusaki Y, Takahara K, Koga N, Amano T, Haga S, Arihiro S. A case of mechanical reperfusion therapy for cerebral infarction induced by tumor embolism from lung cancer. J Neuroendovascular Ther. 2019;13(8):342-347.
- Xiromeritis N, Klonaris C, Papas S, Valsamis M, Bastounis E. Recurrent peripheral arterial embolism from pulmonary cancer. Case report and review of the literature. Int Angiol. 2000;19:79-83.
- Starr DS, Lawrie GM, Morris Jr GC. Unusual presentation of bronchogenic carcinoma: case report and review of the literature. Cancer. 1981;47(2):398-401.
- Park JH, Seo H-S, Park SK, Suh J, Kim DH, Cho YH, et al. Spontaneous systemic tumor embolism caused by tumor invasion of pulmonary vein in a patient with advanced lung cancer. J Cardiovasc Ultrasound. 2010;18(4):148-50.
- Chin J, Migliozzi M, Nguyen G, Kviatkovsky B, Lomiguen C. Atrial invasion and showering phenomenon in primary lung cancer: A case report. Respir Med Case Rep. 2020;30:101064.
- Takahashi K, Furuse M, Hanaoka H, Yamada T, Mineta M, Ono H, et al. Pulmonary vein and left atrial invasion by lung cancer: assessment by breath-hold gadolinium-enhanced three-dimensional MR angiography. J Comput Assist Tomogr. 2000;24(4):557-61.
- Whyte RI, Starkey TD, Orringer MB. Tumor emboli from lung neoplasms involving the pulmonary vein. J Thorac Cardiovasc Surg. 1992;104(2):421-425.
- McLachlan RHP, Islam S, Sasidharan P, Loa J. Open thrombectomy for acute abdominal aortic occlusion due to tumor embolism after lung resection. Annals of Vascular Surgery. 2021;25:S0890-5096.
- Orihashi K, Goldiner PL, Oka Y. Intraoperative assessment of pulmonary vein flow. Echocardiography. 1990;7(3):261-271.
- Webb DF, Tomatis L, Taber RE, Ponka JL. Successful surgical management of superior mesenteric and femoral artery tumor emboli resulting from pneumonectomy. Henry Ford Hosp Med J. 1965;13(3):299-302.
- Smith WS, Furlan AJ. Brief history of endovascular acute ischemic stroke treatment. Stroke. 2016;47(2):e23-e6.
- Tsubouchi K, Ibusuki R, Makisumi K, Okamoto H, Iwasaki T, Okamatsu Y, et al. Tumor embolism as a cause of renal artery occlusion and acute kidney injury diagnosed and treated with endovascular intervention in a patient with mediastinal undifferentiated sarcoma. Intern Med. 2021;60(12):1907-1910.
- Pop R, Mihoc D, Manisor M, Richter JS, Lindner V, Janssen-Langenstein R, et al. Mechanical thrombectomy for repeated cerebral tumor embolism from a thoracic sarcomatoid carcinoma. BMJ Case Rep. 2017;2017:bcr2017013092.
Citation: McLachlan HP Rohan (2021) Special Considerations in the Diagnosis and Treatment of Acute Arterial Occlusion Caused By Tumor Embolization. J Vasc Med Surg. S7: 005.
Copyright: © 2021 McLachlan HP Rohan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.