Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
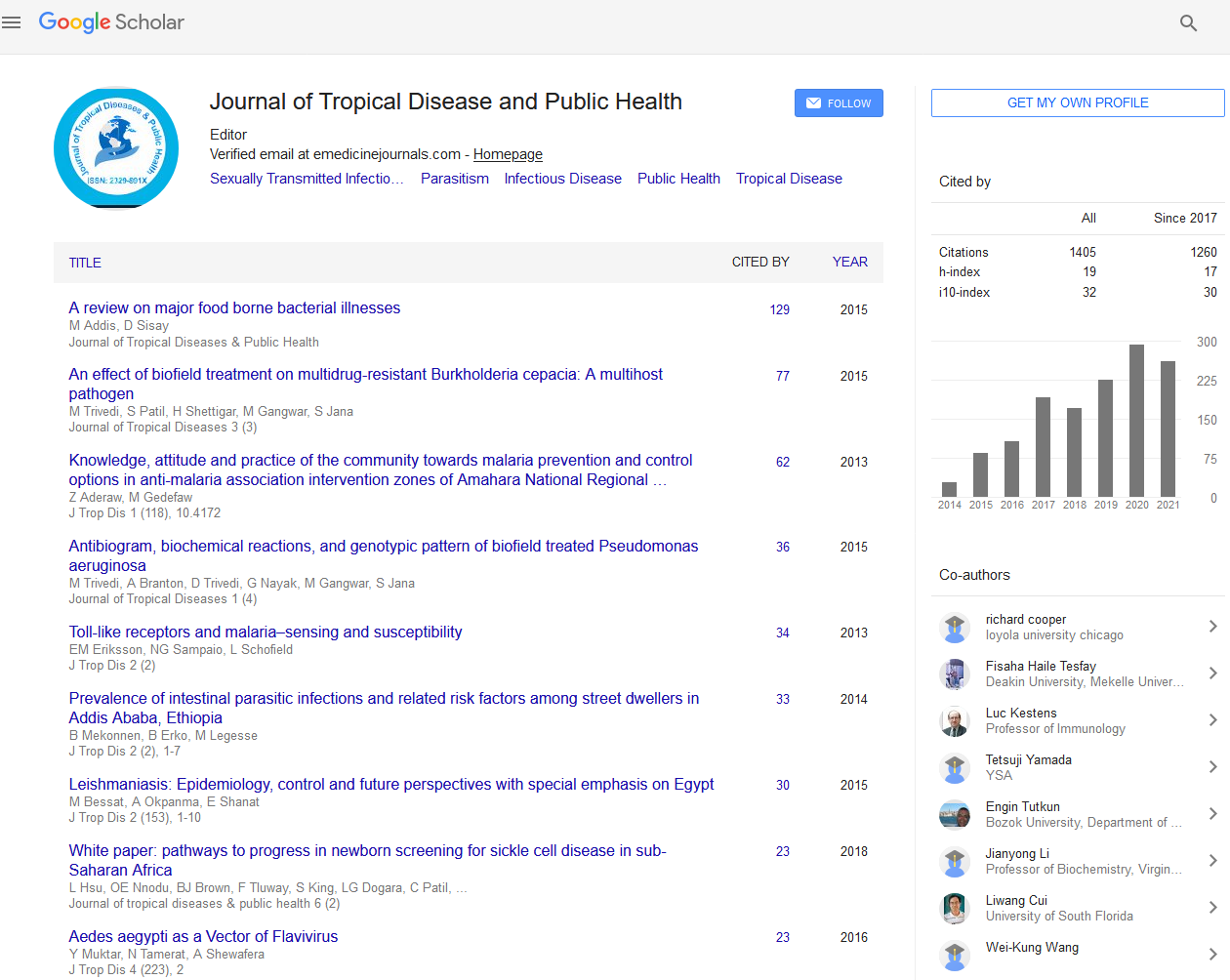
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 9, Issue 2
Sickle Cell Disease (SCD) and COVID-19: Case Series
Awaji Q Al-Naami, Liaqat Ali Khan*, Faisal I Zaidan, Hussam M Halawi, Laila E Asiri, Taher A Sumaili, Amal A Qaisi, Ibrahim A Al-Naami and Turki M DarweeshReceived: 03-Dec-2020 Published: 14-Dec-2020, DOI: 10.35248/2329-891X.2021.9.268
Abstract
The ongoing pandemic of COVID-19 that started in the Hubei province of China in late December 2019, caused by severe acute respiratory syndrome corona virus-2 (SARS CoV-2). Globally millions affected by the disease so far. The risk of COVID-19 severity and its complications increases with age and other comorbidities. The course of SARS-CoV-2 infection or its related complications has yet to be established in patients with sickle cell disease (SCD), once more evidence is available. It is clear from the available data that the course of COVID-19 in patients with SCD is mild to moderate, seldom severe, and rarely fatal. Herein we report three known cases of SCD with confirmed COVID-19, in whom the course of the disease was mild to moderate and uncomplicated with uneventful recoveries.
Keywords
SARS CoV-2; COVID-19; Infection; Sickle cell disease; Vaso-occlusive crisis
Introduction
The current pandemic of COVID-19 caused by SARS-CoV-2 affects millions worldwide. As of November 26, 2020, worldwide confirmed infections are over 60 million in 191 countries/territories [1]. The disease brought challenges to almost every sector of life, specifically health. The more vulnerable individuals are aged and with comorbidities [2]. The most challenging aspect of healthcare is the care of patients with comorbidities that necessitate balancing the care needed with their exposure to SARS CoV-2 infection.
Sickle cell disease (SCD) an autosomal recessive disorder due to a single point mutation of glutamic acid by valine at position six. Patients with SCD pose a management challenge for healthcare due to the complexity of the disease and the scarce published data on pathophysiological interaction of SARS CoV-2 infection in sickle cell disease. Herein, we report a case series of three known patients of SCD with confirmed infection of SARS CoV-2.
Case 1
A 23 year old female, a known patient of SCD with HbSS, presented to the emergency department with history of Vaso- Occlusive Crisis (VOC) and nasal congestion. There was no history of cough or fever. The patient’s history is suggestive of SCD with repeated VOC. Due to the current COVID-19 pandemic, clinical evaluation was done under standard precautions and was unremarkable. Vitals were; pulse, 86/min, BP, 117/78mmHg, and respiratory rate, 20/min. Laboratory workup shows; Hb 10.3g/dL, WBCs 9.1x103/μL, 375x103/μL. Oxygen saturation was 96% with 3lit supplemental oxygen by face mask. IV fluids initiated in ED with IV morphine 0.1mg/kg. After two hours of management in the ED, the patient shifted to an isolation unit for close observation and management. Biochemistry result shows urea, 2.34mmol/L, creatinine, 60mmol/L, Na+135mmol/L and K+, 3.2mmol/L. Nasopharyngeal swab, taken for RT-PCR, which came out positive the next day. Medications includes hydroxyurea as the patient’s medication, IV ceftriaxone, paracetamol, Vitamin-D, and calcium carbonate. The pain severity improved the next day, and the patient was discharged home after two days with specific COVID-19 recommendations (Figure 1).
Case 2
A 30 year old male, a known patient of SCD with HbSS, presented to the emergency department with fever and generalized body aches since last night but no history of cough. Under the standard protocol, clinical evaluation was unremarkable with vitals as; Temp 39°C, pulse 91/min, BP 115/75 mmHg. Oxygen saturation was 95% with 3lit oxygen by face mask. Initial laboratory workup in the ED shows; Hb 13g/dL, WBCs 8.7x103μL, 305x103/μL. With early initiation of IV fluids and IV analgesics (morphine) with oxygen supplementation, the patient’s symptoms improved. After initial management in the ED, the patient shifted to the isolation ward with standard protocol. COVID-19 test requested, a nasopharyngeal swab taken by the assigned team for real-time polymerase chain reaction (RT-PCR) with a positive report a day after. Biochemistry workup was within normal limits. CXR showed no positive findings. The patient was put on regular doses of IV ceftriaxone, IV morphine, tab favipiravir, calcium carbonate, and Vitamin-D as per protocol. The patient’s symptoms improved with no further intervention and discharged home on 3rd day of admission with standard recommendations (Figure 2).
Case 3
A 21 year old male patient, a known case of SCD with HbSS with a history of contact to COVID-19 positive patient, presented to the primary care center with a history of sore throat and two episodes of loose motion. There was no history of cough or fever. Due to contact with a COVID-19 patient, RT-PCR requested. The patient was advised for quarantine after primary care management, to be followed, if needed. The test result came positive, a day after. The patient followed for the next ten days with no mishap.
Discussion
The present pandemic of COVID-19 caused by severe acute respiratory syndrome corona virus-2 (SARS CoV-2) is a public health crisis of the century. The disease affected millions globally. Individuals with comorbid conditions are more vulnerable than healthy ones. The course of COVID-19 varies from asymptomatic to more severe. Despite the comorbid condition of SCD, the patient clinical course is mild, and the severity is less in this group.
Nur et al [3]. reported two SCD patients with HSS. Both were positive for COVID-19, and their presenting symptom was pain and both recovered well. Three patients of one family reported by Abdulqader et.al [4], the symptoms ranged from asymptomatic to VOC and ACS in one patient with the un-eventful recovery of all the three.
Mass screening in Bahrain reports a total of 378 patients with SCD, 1% of the screened population [5]. A total of six patients were positive for COVID-19. All six patients were HSS genotype, of whom three remained asymptomatic, two had mild symptoms, and only one required supplemental oxygenation. All patients recovered well. Menapace and Thein concluded the same observation of less severe outcome of COVID-19 in SCD patients, and the usual presentation was pain not fever [6].
There is conflicting evidence of COVID-19 severity in SCD. In the UK, a massive survey over 4-weeks, there were 195 confirmed or clinically suspected cases of COVID-19, the majority of the cases (n=166) were patients with SCD. Severe course of disease and mortality recorded in aged patients and not in children [7].
Pre-exposure prophylaxis is a hallmark of patient management with SCD during the pandemic of COVID-19. Patients are advised and encouraged to adhere strictly to social distancing, hand hygiene, and avoiding unnecessary exposure to public places, and also to adhere to their disease-modifying medications to minimize the frequencies of VOC, thus subsequently hospital visits [8].
From the limited published data, it is not clear whether SCD increases the possibility of SARS CoV-2 infection but, it is clear from the available data of case reports that the course of COVID-19 was mild-moderate and rarely severe. The protective factors in SCD patients for SARS CoV-2 infection need to be explored with a clearer understanding of the relationship between SCD and COVID-19 once more evidence is available [9].
Conclusion
The course of COVID-19 in these patients was mild to moderate with un-eventful recovery. Considering SCD patients with concurrent COVID-19 as high-risk individuals and should be managed with established protocols.
Ethical Approval
Not applicable.
Consent
Written informed consent was taken from patients for publication of their cases.
Conflict of Interest
The authors declare that they have no conflict of interest.
REFERENCES
- The Johns Hopkins University of Medicine. COVID-19 dashboard by the Center for Systems Science and Engineering at Johns Hopkins University. 2020.
- Hussain FA, Njoku FU, Saraf SL, Molokie RE, Gordeuk VR, et al. COVID– 19 infection in patients with sickle cell disease. British J Haematol. 2020;189:851-852.
- Nur E, Gaartman AE, Van T, Tang MW, Biemond BJ. Vaso– occlusive crisis and acute chest syndrome in sickle cell disease due to 2019 novel coronavirus disease (COVID– 19). Am J Hematol. 2020;95:725-726.
- Al-Hebshi A, Mohammed Z, Amer A, Ghaya AQ, Sofyan Y, Naif H, et al. A Saudi family with sickle cell disease presented with acute crises and COVID– 19 infection. Pediatric Blood Cancer. 2020;67:e28547.
- Abdulkarim AR, Salman AA, Omar Y, Mohammed S, Sameer O, Stephen L, et al. COVID-19 and Sickle Cell Disease in Bahrain, Int J Infect Dis. 2020;101:1-16.
- Laurel A. Menapace and Swee Lay Thein. COVID-19 and sickle cell disease. Haemtologica. 2020;105:255398.
- Telfer P, Fuente J, Sohal M, Brown R, Eleftheriou P, Roy N, et al. Real-time national survey of COVID-19 in hemoglobinopathy and rare inherited anemia patients. Haematologica 2020;105:2651-2654.
- Chakravorty S, Padmore-Payne G, Ike F, Tshibanguet V, Graham C, Rees D, et al. COVID-19 in patients with sickle cell disease - A case series from a UK Tertiary Hospital. Haematologica. 2020;105:2691-2693.
- Azerad MA, Bayoudh F, Weber T, Jean-Marc M, Ketelslegers O, Hoyoux M, et al. Sickle cell disease and COVID-19: A typical presentations and favorable outcomes. EJ Haem. 2020;2:70-74.
Citation: Al-Naami AQ, Khan LA, Zaidan FI, Halawi HM, Asiri LE, Suamili TA, et al. (2021) Sickle Cell Disease (SCD) and COVID-19â??Case series. J Trop Dis 9:269. doi: 10.35248/2329-891X.2021.9.269
Copyright: © 2021 Al-Naami AQ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.