PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
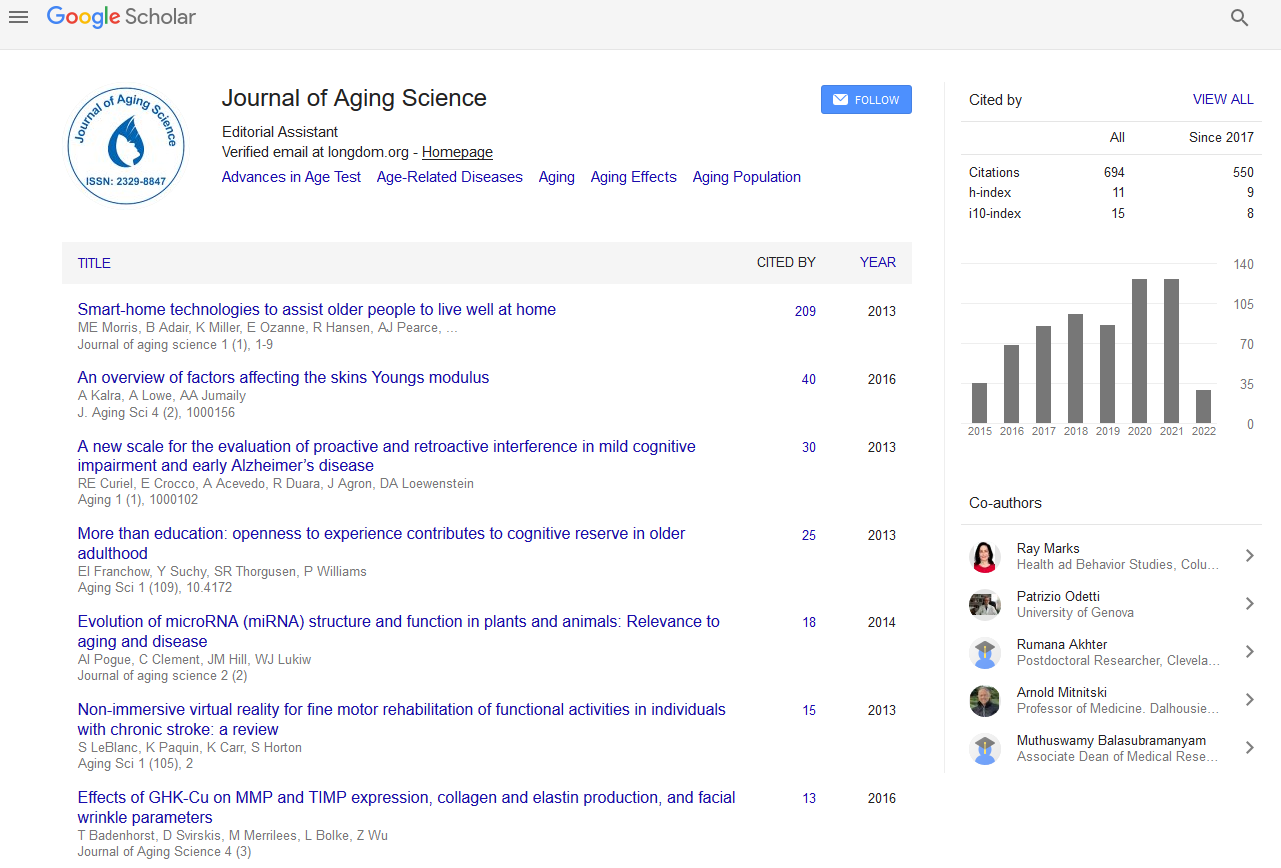
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2020) Volume 8, Issue 1
Schizoaffective Disorder: A Challenge
Ueberberg Bianca and Assion Hans-Joerg*Received: 10-Mar-2020 Published: 31-Mar-2020, DOI: 10.35248/2329-8847.20.08.221
About the Study
Schizoaffective Disorder (SAD) is a mental disorder characterized by symptoms of schizophrenia and affective disorder like depression and/or mania, which occur simultaneously or alternately. In the international classification of mental disorders, ICD-10, it is subsumed under the spectrum of schizophrenia, schizotypal and delusional disorders. However, the available research results do not allow a final decision whether SAD is more appropriate classified in the affective disorder chapter [1].
The term "schizoaffective" can be traced back to the American psychiatrist John Kasanin (1933). In an article published in the American Journal of Psychiatry, he described nine cases of patients in good constitution and with appropriate social adjustment, who suddenly developed a dramatic psychosis consisting of both schizophrenic and affective symptoms. The duration of these episodes lasted not very long and the prognosis was favorable. Today, however, schizoaffective psychoses are clinically understood as symptoms that are close to the "incidents" of Kurt Schneider's clinical psychopathology. These are cases in which the differential typology of schizophrenia or cyclothymia (manic-depressive illness) can only hardly be decided [2]. However, no agreement has yet been reached on the nosological status of SAD, so that several hypotheses exist [3]:
(i) SAD is a type of schizophrenia
(ii) SAD is a type of affective disorder
(iii) SAD represents a third, independent disease entity
(vi) SAD is in the transition zone between schizophrenia and affective disorder (continuum)
(v) SAD is a combination of schizophrenia and affective disorder (comorbidity)
(vi) SAD is a heterogeneous syndrome.
In the clinical field, various studies are available, that support and contradict individual hypotheses.
In Germany, the diagnosis is based on the International Classification of Diseases (ICD-10), which differs in some points from the definition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), commonly used in many other countries. The ICD-10 conceptualizes SAD as an episodic disease and is strongly oriented towards the cross-sectional symptoms of the episode. Both affective and schizophrenic symptoms occur in the same episode. According to DSM-5, the focus is more on the longitudinal symptoms, and psychotic symptoms must be present for at least two weeks without affective symptoms (in contrast to ICD-10). The differentiation of SAD from bipolar affective disorders is also often difficult. While bipolar affective disorder is an affective disorder characterized by changes in motivation, activity and mood towards mania/depression and has been widely studied, schizoaffective disorder remains comparatively little researched despite frequent diagnosis in clinical practice.
Due to the open discussion on diagnostic classification, information on epidemiology and etiopathogenesis of SAD is also difficult to collect. According to Tavcar, exact epidemiological statements are not possible due to a limited number of studies. A lifetime prevalence of 0.5%-0.8% is estimated, whereby Angst assumes that 10%-25% of psychoses diagnosed as schizophrenia or affective psychoses can be assigned to schizoaffective psychoses [4-6]. Aetiopathogenetically, similar to schizophrenia and affective disorders, a multifactorial genesis can probably be postulated [7]. Molecular genetic data show that bipolar disorder and schizophrenia are not completely separate disease entities and that SAD has a genetic relationship to both schizophrenia and bipolar disorder [8].
For treatment of SAD no guidelines have been developed and only a few controlled studies have examined the pharmacological treatment of this disorder. The best evidence is provided by atypical antipsychotics. Nevertheless, the aim should be to enable individual therapy, possibly supported by psychotherapy or in cases of resistance to therapy by electroconvulsive therapy [9].
In terms of their long-term prognosis, SADs are placed somewhere between schizophrenia and bipolar affective disorders [10,11]. In 50% of cases residual symptoms develop [12]. SAD remains still a challenge in diagnosis and treatment [13,14].
REFERENCES
- Dilling H, Mombour W, Schmidt MH. Internationale Klassifikation Psychischer Störungen. ICD-10 Kapitel V (F). Klinisch-diagnostische Leitlinien. 8. Auflage. Verlag Hans Huber, Bern. 2011.
- Schneider K. Klinische Psychopathologie, 12. Aufl. Thieme Stuttgart, New York, USA. 1980.
- Marneros A. Das neue Handbuch der Bipolaren und Depressiven Erkrankungen. Thieme, Stuttgart, New York, USA. 2004.
- Angst J. The course of schizoaffective disorders. In: Maneros A, Tsuang MT (eds), Schizoaffective Psychoses. Springer-Verlag, Berlin Heidelberg New York, USA, 1986; pp: 63-93.
- Maurer K, Schneider B. Die Bedeutung der pharmakologischen Behandlung bei schizoaffektiven Störungen. In: Hartwich P, Barocka A (eds), Schizoaffektive Psychosen: Diagnostik und Therapie. Verlag Wissenschaft und Praxis, Sternenfels. 2005; pp: 131-141.
- Tavcar R. Schizoaffective disorder: from Kraepelin to gene. Psychiatria Danubina. 2008;20(3): 396-398.
- Hartwich P. Zur Psychodynamik und Psychotherapie schizoaffektiver Psychosen. In: Hartwich P, Barocka A (eds), Schizoaffektive Psychosen: Diagnostik und Therapie. Springer Verlag Wissenschaft und Praxis publisher, Sternenfels. 2005; pp: 47-76.
- Craddock N. (2011). Genetics of schizoaffective disorder. Psychiatry. 2011;8(2): 82-90.
- Vieta E. Developing an Individualized Treatment Plan for Patients With Schizoaffective Disorder: From Pharmacotherapy to Psychoeducation. J Clin Psychiatry. 2010;71: 14-19.
- Studentkowski G, Scheele D, Calabrese P, Balkau F, Höffler J, Aubel T, et al. Cognitive impairment in patients with a schizoaffective disorder: a comparison with bipolar patients in euthymia. Eur J Med Res. 2010;15(2): 70-78.
- Marneros A. Schizoaffektive Störungen. Psychiatr Psychother. 2011;5(1): 17-30.
- Assion HJ, Schweppe H, Reinbold H, Frommberger U. Pharmacological treatment for schizoaffective disorder. A comparison with schizophrenia and bipolar disoreder. Der Nervenarzt. 2019;(90): 1-8.
- Balkau F, Juckel G, Assion HJ. Migration als Belastungsfaktor einer schizoaffektiven Störung. Psychiat Prax. 2007;34(7): 354-356.
- Marneros A. Das Konzept der schizoaffektiven Psychosen: Kämpfe um eine klinische Realität. In: Hartwich P, Barocka A (eds), Schizoaffektive Psychosen: Diagnostik und Therapie. Verlag Wissenschaft und Praxis, Sternenfels. 2005; pp: 11-38.
Citation: Hans-Jorg A, Bianca U (2020) Schizoaffective Disorder: A Challenge. J Aging Sci. 8: 221. Doi: 10.35248/2329-8847.20.08.221
Copyright: © 2020 Hans-Jorg A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.