PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2020) Volume 11, Issue 3
Safety is Absolutely Essential during Laparoscopic Liver Resection in Cancer Patients
Miyazawa M1,2*, Aikawa M2, Takashima J1 and Kobayashi H12Department of Gastroenterological Surgery, Saitama Medical University International Medical Center, Saitama, Japan
Received: 25-Apr-2020 Published: 15-May-2020, DOI: 10.35248/2157-2518.20.11.350
Abstract
To date, many cancer surgeries in the 21st century have involved minimally invasive laparoscopic procedures. In such cases, it is essential for liver cancer patients that laparoscopic surgery 1) provides equivalent or superior treatment results to those provided and 2) is less invasive. These general principles also apply to liver cancer patients (LLR), and both must be met to ensure a meaningful and satisfactory outcome.
Keywords
Monopolar Soft-Coagulation Device; Cancer Patients; Metastasis; Oncogenes; Liver Cancer
Introduction
Many previous reports have described equivalent or better results with LLR than with laparotomy surgery for the treatment of primary and metastatic liver cancer [1-3]. When used during a cancer resection procedure, LLR may be associated with a smaller surgical margin than laparotomy, which could lead to worse treatment outcomes. However, surgeons performing LLR should aim for true minimal invasiveness, rather than the achievement of a clean-looking surgery for publication.
Laparoscopic Liver Resection in Cancer Patients
However, many reports suggest that LLR reduces the amount of intraoperative bleeding and thus reduces the requirement for blood transfusion. Potentially, therefore, the advantages and disadvantages of LLR during the perioperative period are balanced, and the resulting treatment outcomes are equivalent to or better than those achieved with open cancer resection surgery [4,5]. Compared to open surgery, LLR is associated with less postoperative pain and a shorter postoperative hospital stay [6,7]. However, these parameters alone are not sufficient to designate LLR as less invasive than open surgery. A patient may select LLR surgery over laparotomy because they expect that the former will cause less postoperative pain and enable a more rapid discharge, and surgeons must strive to meet patients ’ expectation in this regard.
The operating surgeon also advises the patient about LLR surgery by explaining that LLR causes fewer complications and less postoperative pain. A disappointing experience for a patient who then states that “ I would not have had the same complications if I had undergone laparotomy surgery,” indicates a failure of the expected minimal invasiveness of LLR. The most common complication that leads to mortality after hepatectomy is intraoperative bleeding [8,9]. Surgical mortality due to a large amount of intraoperative blood loss has also been reported for LLR, which is completely contrary to the minimally invasive characteristic of the procedure. If the surgeon chooses LLR instead of laparotomy, the surgical mortality rate, at least, should be zero.
The liver contains a large number of vascular networks. Therefore, transection of the liver is synonymous with transection of the blood vessels. To prevent bleeding during liver transection, both sides of the blood vessel to be transected must be clipped, or a certain length must be sealed to enable a cut through the central portion. However, when a vasculature-rich tumor such as hepatocellular carcinoma must be excised, it would be impossible to identify all blood vessels to ensure a bleeding-free operation. Several videos have demonstrated the reliable identification and clipping of blood vessels and the performance of advanced liver transection and anatomical hepatectomy with reduced bleeding [10]. However, those reports describe very successful surgical cases. In actual clinical practice, it is not uncommon for copious intraoperative bleeding to occur but is successfully stopped when, for example, surgeons attempt dissection of a large blood vessel using a cavitron ultrasonic surgical aspirator or similar device. Such large hemodynamic changes can cause liver failure.
Discussion
Furthermore, one cannot state with certainty that LLR is mentally minimally invasive for the operating surgeon. Compared to open surgery, it is more difficult to stop bleeding instantly during LLR, and uncontrolled bleeding could fill the abdominal cavity with blood. The immediate stoppage of even a small amount of bleeding or the use of a technique such as monopolar soft-coagulation device to coagulate small blood vessels and detach large blood vessels during LLR may not yield a clean and video-worthy surgical procedure (Figure 1). However, these steps may reduce the amount of intraoperative bleeding and improve the safety of the procedure [11].
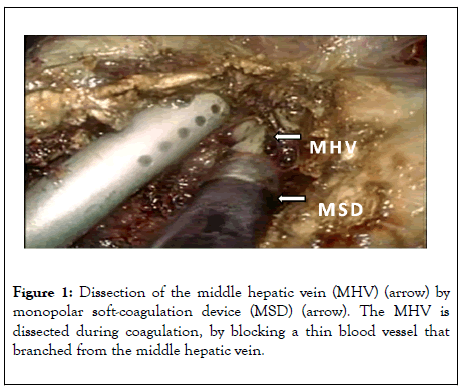
Figure 1: Dissection of the middle hepatic vein (MHV) (arrow) by monopolar soft-coagulation device (MSD) (arrow). The MHV is dissected during coagulation, by blocking a thin blood vessel that branched from the middle hepatic vein.
Conclusion
In conclusion, reductions in intraoperative bleeding and perioperative complications are required during minimally invasive LLR. However, surgeons performing LLR should aim for true minimal invasiveness, rather than the achievement of a clean-looking surgery for publication.
REFERENCES
- Xiangfei M, Yinzhe X, Yingwei P, Shichun L, Weidong D. Open versus laparoscopic hepatic resection for hepatocellular carcinoma: a systematic review and meta-analysis. Surg Endosc. 2019;33(3):2396-2418.
- Beppu T, Wakabayashi G, Hasegawa K, Gotohda N, Mizuguchi T, Takahashi Y, et al. Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci. 2015;22(10):721-727.
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250(5):831-841.
- Li N, Wu YR, Wu B, Lu MQ. Surgical and oncologic outcomes following laparoscopic versus open liver resection for hepatocellular carcinoma: A meta-analysis. Hepatol Res. 2012;42(1):51-59.
- Kasai M, Cipriani F, Gayet B, Aldrighetti L, Ratti F, Sarmiento JM, et al. Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient data. Surgery. 2018;163(5):985-995.
- Reddy SK, Tsung A, Geller DA. Laparoscopic liver resection. World J Surg. 2011;35(4):1478-1486.
- Piardi T, Sommacale D, Baumert T, Mutter D, Marescaux J, Pessaux P, et al. Laparoscopic resection for hepatocellular carcinoma: comparison between Middle Eastern and Western experience. Hepatobiliary Surg Nutr. 2014;3(2):60-72.
- Pai M, Frampton AE, Mikhail S, Resende V, Kornasiewicz O, Splading DR, et al. Radiofrequency assisted liver resection: analysis of 604 consecutive cases. Eur J Surg Oncol. 2012;38(3):274-280.
- Kim JH, Cho BS, Jang JH. Pure laparoscopic anatomical segment VI resection using the Glissonian approach, Rouviere's sulcus as a landmark, and a modified liver hanging maneuver (with video). Langenbecks. Arch Surg. 2018;403(1):131-135.
- Moisan F, Gayet B, Ward MA, Tabchouri N, Fuks D. Segment 7 Laparoscopic Liver Resection: Is It Possible to Resect When Metastatic Lesions Border Suprahepatic Veins. J Gastrointest Surg. 2018;22(5):1643-1644.
- Miyazawa M, Aikawa M, Okada K, Watanabe Y, Okamoto K, Koyama I, et al. Laparoscopic liver resection using a monopolar soft-coagulation device to provide maximum intraoperative bleeding control for the treatment of hepatocellular carcinoma. Surg Endosc. 2018;32(9):2157-2158.
Citation: Miyazawa M, Aikawa M, Takashima J, Kobayashi H (2020) Safety is Absolutely Essential during Laparoscopic Liver Resection in Cancer Patients. J Carcinog Mutagen. 11:350. DOI: 10.35248/ 2157-2518.20.11.350.
Copyright: © 2020 Miyazawa M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


