PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
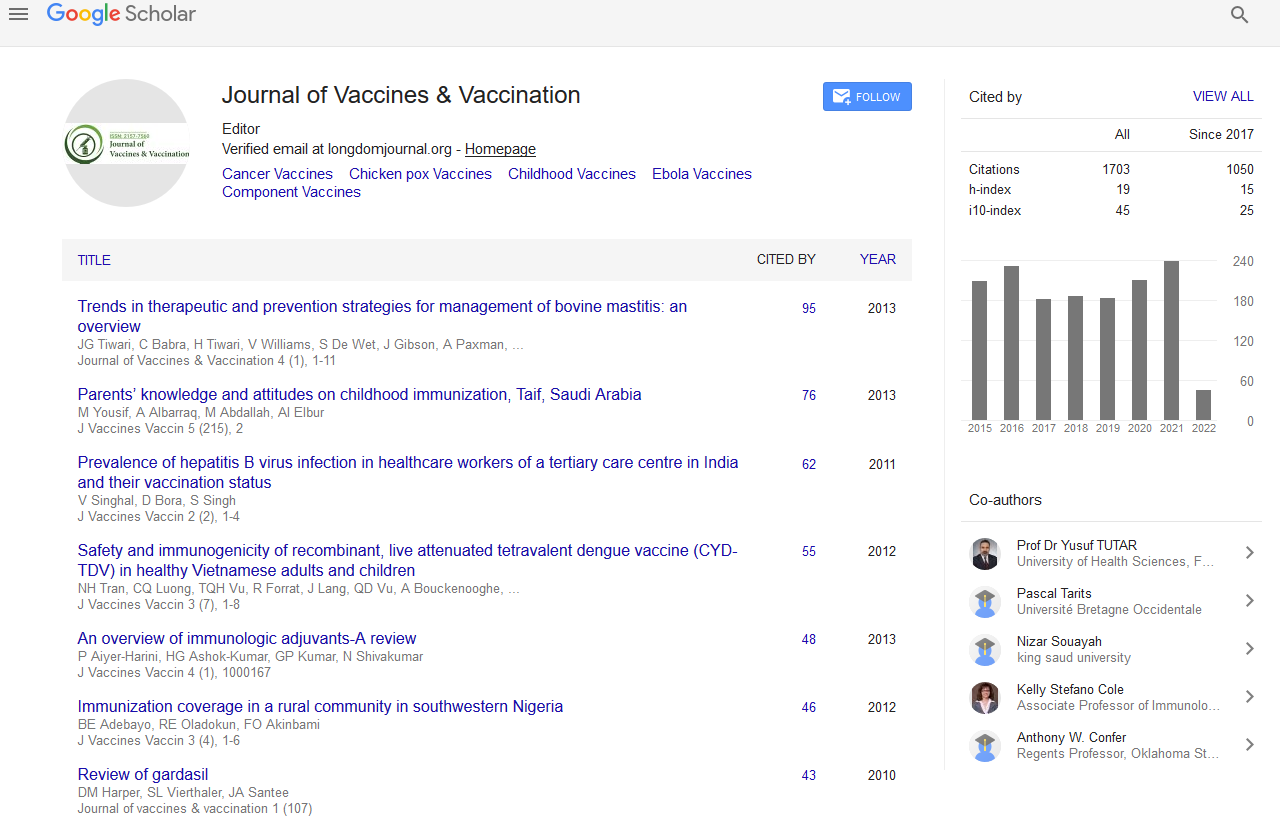
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Editorial - (2021) Volume 0, Issue 0
Risk Factors of COVID 19 Vaccination
Wenjun Lee*Received: 01-Jul-2021 Published: 22-Jul-2021, DOI: 10.35248/2157-7560.21.s14.e001
Description
Vaccines prevent the spread of contagious and deadly diseases. The early and nonspecific innate immune response, which can cause adverse effects like tiredness, malaise, and irritability, causes inflammatory markers to rise within hours following vaccination. The inflammatory reaction, as the first stage of the immune response, normally lasts a few days but can last longer in some people, such as those who are depressed. The adaptive immune system is in charge of the immune response's second prong. Because it focuses on certain vaccine components, it takes longer to deploy. Vaccines are intended to imbue the adaptive immune system with a long-term memory of viral or bacterial components, allowing it to respond rapidly and efficiently when challenged with infections. The adaptive immune system responds to the vaccination by (a) multiplying T cells, which can be programmed to recognize and kill pathogen-infected cells, and (b) producing antibodies, which are proteins that neutralize viruses and bacteria.
Although there was evidence that stress altered several elements of immune function, the clinical significance was unknown. Vaccination is a useful model for assessing the immune system's ability to respond to infections because everyone receives the same standardized dose but responses might vary greatly. We gave medical students the normal series of three hepatitis B inoculations over the course of six months, each on the third of three days of rigorous academic examination blocks. After the first treatment, 25% of the pupils exhibited a hepatitis B antibody response. Early responders reported feeling less stressed and anxious than those who responded later. Surprisingly, the stress, anxiety, and social support of earlier and later responders did not differ over the previous academic year, implying that their divergent vaccine responses were attributable to the more proximal stressful examination time. These findings were confirmed a year later. Following that, studies among healthy young adults indicated that self-reported stress levels 10 days after vaccination may have a greater impact on antibody response than stress in the preceding two days, with stress-related sleep loss being a key culprit.
If the vaccine recipient has already seen the antigen-the protein on the pathogen's surface-either through infection or vaccination, this reaction is modulated. If this is the case, the body develops a stronger and faster antibody response (secondary immunological reaction) than it did during the initial contact. Some studies do not adequately account for earlier exposure, making it impossible to determine whether the primary or secondary immune response is reported. Failure to account for earlier exposure, on the other hand, can obscure the severity of stress's influence. It's safe to presume that certain antigens have already been encountered by older adults, and that they will produce a secondary immune response. Given that approximately 10% of Americans have past exposure as of September 2020, this is a critical consideration for the SARSCoV- 2 vaccination. Many more people have been exposed to other coronaviruses, which could affect immune responses to SARS-CoV-2, and several vaccine candidates require multiple doses.
Conclusion
Immune responses to vaccinations are even worse in younger caretakers. When compared to parents of generally developing children, parental caregivers of children with developmental disabilities exhibited lower antibody responses to the influenza virus vaccine and the pneumococcal pneumonia vaccine, which elicits a primary immune response. These data suggest that providing intense care, especially to children, can increase vulnerability to bacterial and viral illnesses.
Citation: Lee W (2021) Risk Factors of COVID 19 Vaccination. J Vaccines Vaccin. S14:e001
Copyright: © 2021 Lee W. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.