PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
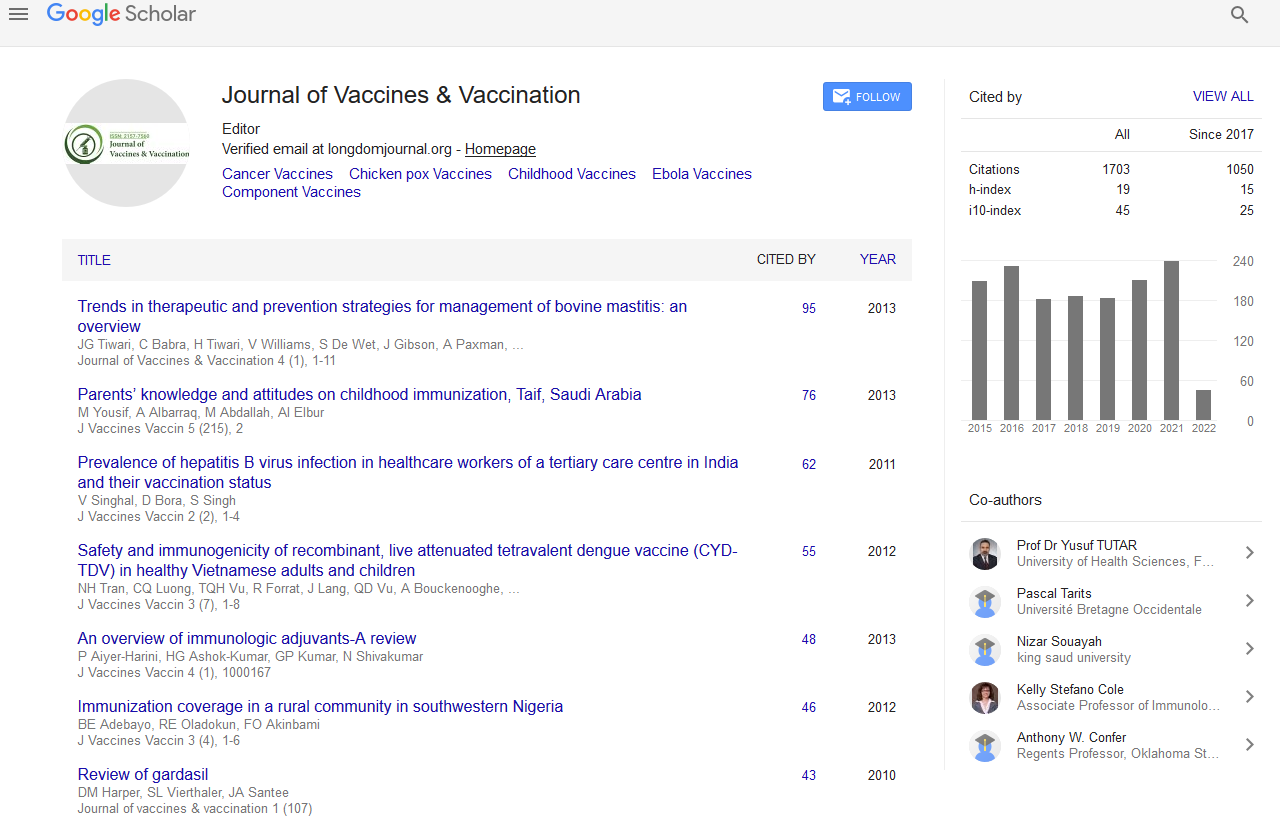
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Editorial - (2020) Volume 11, Issue 6
Rheumatoid Arthritis Vaccine
Lu Zhoa*Received: 25-Nov-2020 Published: 17-Dec-2020, DOI: 10.35248/2157-7560.20.11.e432
Abstract
Rheumatoid Arthritis (RA) is an autoimmune disorder which will cause joint pain and damage throughout your body. The joint damage that RA causes usually happens on each side of the body. So, if a joint is affected in one among your arms or legs, an equivalent joint within the other arm or leg will probably be affected, too.
Keywords
Autoimmune Disorder; Rheumatoid arthritis; Physiotherapy
Introduction
In atrophic arthritis, the body's system attacks its own tissue, including joints. In severe cases, it attacks internal organs.
Rheumatoid arthritis affects joint linings, causing painful swelling. Over long periods of your time, the inflammation related to atrophic arthritis can cause bone erosion and joint deformity.
While there is no cure for atrophic arthritis, physiotherapy and drugs can help slow the disease's progression. Most cases can be managed with a class of medications called anti-rheumatic drugs.
Your system normally makes antibodies that attack bacteria and viruses, helping to fight infection.
Stages of Rheumatoid Arthritis Progression
The 4 Stages of Rheumatoid Arthritis Progression
• Stage 1: Early RA.
• Stage 2: Antibodies Develop and Swelling Worsens.
• Stage 3: Symptoms Are Visible.
• Stage 4: Joints Become Fused.
There is no cure for atrophic arthritis (RA), but remission can desire it [1]. Today, early and aggressive treatment with disease- modifying anti rheumatic drugs (DMARDs) and biologics makes remission more achievable than ever before.
Signs and symptoms
Signs and symptoms of rheumatoid arthritis may include:
• Tender, warm, swollen joints
• Joint stiffness that is usually worse in the mornings and after inactivity
• Fatigue, fever and loss of appetite.
Rheumatoid arthritis increases your risk of developing
• Skin Nodules: About half people with RA develop rheumatoid nodules.
• Bones Thinning: Chronic inflammation from RA results in loss of bone density, not only round the joints, but throughout the body, resulting in thin, brittle bones.
• Eyes, Mouth, Lungs, Heart and Blood Vessels, Liver, Kidneys.
• Osteoporosis- Rheumatoid arthritis itself, alongside some medications used for treating atrophic arthritis, can increase your risk of osteoporosis — a condition that weakens your bones and makes them more prone to fracture [2].
• Rheumatoid nodules- These firm bumps of tissue most ordinarily form around pressure points, like the elbows. However, these nodules can form anywhere within the body, including the lungs.
• Dry eyes and mouth- People who have atrophic arthritis are far more likely to experience Sjogren's syndrome, a disorder that decreases the quantity of moisture in your eyes and mouth.
• Infections- The disease itself and lots of the medications wont to combat atrophic arthritis can impair the system, resulting in increased infections.
• Abnormal body composition- The proportion of fat to lean mass is usually higher in people that have atrophic arthritis, even in people that have a traditional body Mass Index (BMI).
• Carpal tunnel syndrome- If atrophic arthritis affects your wrists, the inflammation can compress the nerve that serves most of your hand and fingers.
• Heart problems- Rheumatoid arthritis can increase your risk of hardened and blocked arteries, also as inflammation of the sac that encloses your heart.
• Lung disease- People with atrophic arthritis have an increased risk of inflammation and scarring of the lung tissues, which may cause progressive shortness of breath.
• Lymphoma- Rheumatoid arthritis increases the danger of lymphoma, a gaggle of blood cancers that develop within the lymph system.
Causes
The cause of rheumatoid arthritis is unknown. Even though infectious agents like viruses, bacteria, and fungi have long been suspected, none has been proven because the cause. The explanation for atrophic arthritis may be a very active area of worldwide research. It is believed that the tendency to develop atrophic arthritis could also be genetically inherited (hereditary) [3]. Certain genes are identified that increase the danger for atrophic arthritis. It is also suspected that certain infections or factors within the environment might trigger the activation of the system in susceptible individuals. This misdirected system then attacks the body's own tissues. This results in inflammation within the joints and sometimes in various organs of the body, like the lungs or eyes.
Diagnosis
RA is diagnosed by examining biopsy results, examining the joints and organs, and reviewing x-ray or ultrasound images. There is no one test to diagnose RA [4]. Blood tests are run to seem for antibodies within the blood which will be seen in RA. Antibodies are small proteins within the bloodstream that help fight against foreign substances called antigens. Sometimes these antibodies are found in people without RA. This is called a false positive result. Blood tests are also run to look for high levels of inflammation. The symptoms of RA are often very mild making the diagnosis harder. Some viral infections can cause symptoms which will be mistaken for RA. A rheumatologist is a physician with the skill and knowledge to reach a correct diagnosis of RA and to recommend a treatment plan.
Treatment
Treatment options include medications, physical therapy, occupational therapy, counselling, and surgery.
• Non-Steroidal Anti-Inflammatory drugs (NSAIDs).
• Corticosteroids.
• Disease-Modifying Anti Rheumatic Drugs (DMARDs).
• Tumour Necrosis Factor-alpha inhibitors (TNF-alpha inhibitors).
REFERENCES
- FPaul BJ, Kandy HI, Krishnan V. Pre-rheumatoid arthritis and its prevention. Eur J Rheumatol. 2017;4(2):161-165.
- Liao KP, Alfredsson L, Karlson EW. Environmental influences on risk for rheumatoid arthritis. Curr Opin Rheumatol. 2009;21(3):279- 283.
- Honda K, Littman DR. The microbiota in adaptive immune homeostasis and disease. Nature. 2016;535(7610):75-84.
- Zamanpoor M. The genetic pathogenesis, diagnosis and therapeutic insight of rheumatoid arthritis. Clin Genet. 2019;95(5):547-557.
Citation: Zhoa L (2020) Rheumatoid arthritis Vaccine. J Vaccines Vaccin. 11:e432.
Copyright: © 2020 Zhoa L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.