Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
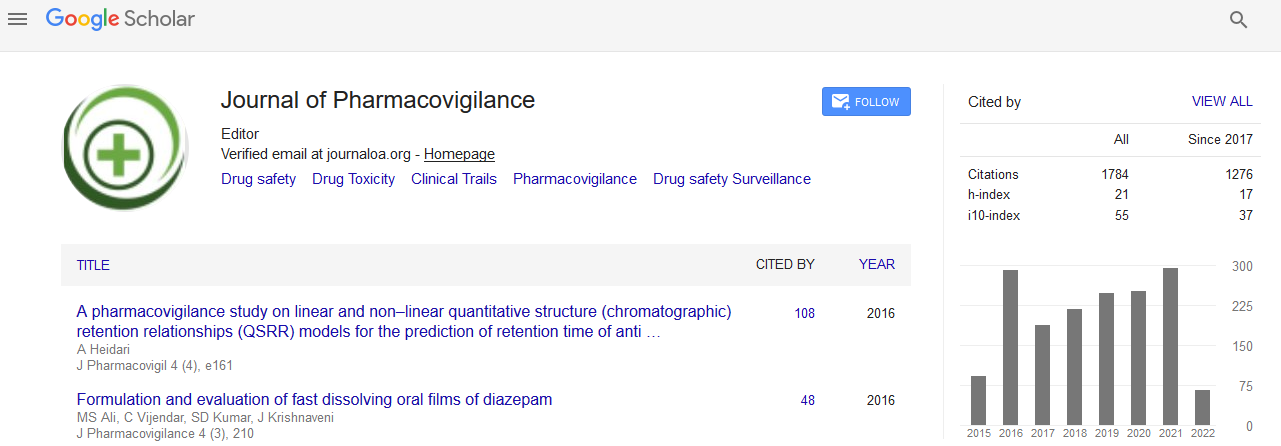
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2021) Volume 9, Issue 2
Principles and Difficulties in Developing Causality Assesment
Archana Guyya*Received: 03-Feb-2021 Published: 24-Feb-2021, DOI: 10.35248/2329-6887.21.9.300
Abstract
Causality assessment of ADRs is a technique utilized for assessing the strength of connection between drug(s) openness and event of antagonistic reaction(s). Causality assessment of ADRs might be embraced by clinicians, academics, the drug business and controllers, and in various settings, including clinical trials. At an individual level, medical care suppliers evaluate causality casually when managing ADRs in patients to settle on choices with respect to future treatment.
Keywords
Pharmacovigilance; Clinical trials; Adverse drug reactions.
Introduction
Causality assessment basically implies finding a causal affiliation or connection between a medication and a medication reaction. It is an evaluation of the likelihood that a particular treatment is the explanation behind a saw ominous event (AE). This is a critical and testing part of pharmacovigilance, in which attempts are made to find the particular medicine liable for causing drug reaction [1]. This is huge in clinical practice as a consistently expanding number of prescriptions are flooding the market and are used by our patients and bound to cause results other than its assets. Pursuing feasibility, security of these drugs is normally disregarded. As the prosperity of the patients is a higher need than feasibility, recognizing the guilty party drugs ends up being altogether more crucial. The principles and methods for causality appraisal or causality evaluation device (CAT) help clinicians with perceiving the guilty party drugs. There are various models or figuring’s open as of now for developing a causal relationship in cases of disagreeable medicine reaction (ADR), indicating that none of them is unequivocal or complete [2].
Principles of Causality Assessment
All causality evaluation techniques or devices follow 4 cardinal standards of conclusion of ADR: (I) worldly relationship of medication with the medication response, (ii) organic credibility, (iii) de-challenge, and (iv) re-challenge. When de-challenge or rechallenge has happened before, it is called positive pre-challenge or negative pre-challenge.
A patient with loose bowels is surrendered metronidazole and assembles a fixed-drug response (FDR) following 2 days of starting metronidazole. As the patient makes speculated medicine reaction, metronidazole is stopped and the patient is put on antihistamines and skin corticosteroids [3]. The patient recuperates well in the wake of halting the medication yet with post provocative hyperpigmentation (fruitful de-challenge). Following 3 months, the patient takes metronidazole in isolation and presents to a dermatologist with the start of FDR at comparative site following 2 days of metronidazole utilization, dermatologist will dissect metronidazole as the purpose behind FDR with more noticeable assurance (successful re-challenge) [4]. As FDR started after the prescription was begun, there is a conspicuous transient association of the medicine with the drug related cutaneous appearance. To the most astonishing perspective our understanding about metronidazole, it is normally possible that metronidazole can cause FDR. Hence, previously mentioned model thinks about all cardinal parts of causality of ADR. The majority of methods that are recorded underneath rely upon these cardinal principles that help clinicians with reaching a particular conclusion result concerning the likelihood of an assumed medication causing a given medication response [5].
Nonetheless, when a patient of upper respiratory parcel disease of suspected viral etiology is put on anti-toxins builds up a maculopapular rash following 2 days of anti-microbial use, it is hard to tell whether the rash is because of viral contamination or because of a medication as the two of them are transiently related and are conceivable to cause a rash. De-challenge of the two of them can bring about effective goal of the rash while re-challenge is hard to perform morally [6]. For such down to earth reasons, we require some different techniques for building up causality.
Conclusion
Thusly, challenges in causality assessment are lacking information of ADR, polypharmacy, variable clinical responses, powerless appreciation of normal acceptability, other elective causes, and nonappearance of planning to clinicians. A portion of these elements, for example, factor clinical reactions and organic believability are hereditarily or immunologically decided and in this way very little should be possible about them. Perceiving causality in polypharmacy is a tricky situation as dechallenge– rechallenge examination is crazy or considered every individual drug that is a piece of polypharmacy. Moreover, there are no target immunological tests in hypersensitive medication responses as medication is a deficient antigen or hapten. Because of these variables, the greater part of the causality evaluation strategies referenced underneath are not full-evidence.
REFERENCES
- Anderson N, Borlak J. Correlation versus causation? Pharmacovigilance of the analgesic flupirtine exemplifies the need for refined spontaneous ADR reporting. PloS one. 2011 Oct 11;6(10):e25221.
- McConaughy SH. Clinical interviews for children and adolescents: Assessment to intervention. Guilford Press; 2013 Feb 25.
- Baroody FM, Shenaq D, DeTineo M, Wang J, Naclerio RM. Fluticasone furoate nasal spray reduces the nasal-ocular reflex: a mechanism for the efficacy of topical steroids in controlling allergic eye symptoms. Journal of allergy and clinical immunology. 2009 Jun 1;123(6):1342-8.
- Miremont-Salamé G, Théophile H, Haramburu F, Bégaud B. Causality assessment in pharmacovigilance: the French method and its successive updates. Therapies. 2016 Apr 1;71(2):179-86.
- Kiene H, Hamre HJ, Kienle GS. In support of clinical case reports: a system of causality assessment. Global Advances in Health and Medicine. 2013 Mar;2(2):64-75.
- Gallagher RM, Kirkham JJ, Mason JR, Bird KA, Williamson PR et al. Development and inter-rater reliability of the Liverpool adverse drug reaction causality assessment tool. PloS one. 2011 Dec 14;6(12):e28096.
Citation: Guyya A (2021) Principles and Difficulties in Developing Causality Assesment, J. Pharamacovigil. 9:300. doi-10.35248/2329-6887.21.9.300.
Copyright: © 2021 Guyya A This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.